Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
Patient Stories
The 2025 holiday season took an unexpected turn for Ethelyn St. John when a simple walk into a friend’s home outside of Dayton ended in a serious injury. As she and two friends headed inside for Thanksgiving dinner, one friend lost her balance and fell backward, knocking St. John to the ground.
Family quickly gathered to help, initially focusing on St. John’s friend, who was bleeding from a head wound. When a friend asked St. John if she could stand, she realized she couldn’t.
“It didn’t really hurt at that moment,” she recalled. “It just felt like there was nothing there.”
Soon, both women were on their way to Sheridan Memorial Hospital’s Emergency Department. While her friend’s head injury initially drew attention, an X-ray quickly revealed the seriousness of St. John’s injury: a shattered hip.
That diagnosis set in motion a swift and efficient chain of events.
“They admitted me and got me into a hospital room right away,” St. John explained. “I saw Dr. Brian Laman quickly, and my surgery was scheduled for the next day.”
St. John was able to stay in Sheridan for her entire surgery and recovery process, surrounded by familiar faces and supported by her family in town, as well as her children, who flew in from Arizona and Oklahoma to be by her side.
Dr. Laman, an orthopedic surgeon at Sheridan Orthopedic Associates, performed St. John’s hip replacement.
“He did a good job,” St. John shared. “He got me in and out pretty fast, and he was so positive about it. He acted like I’d get up off the operating table, get in my car and head home.”
After surgery, St. John moved to Sheridan Memorial Hospital’s Transitional Care Unit (TCU), where she focused on recovery and rehabilitation through occupational and physical therapy with Lexie Prosinski, MOTR/L, and Tiffany Sutton, DPT, PT. During her therapy sessions, St. John practiced walking up and down stairs, built confidence in her movement by walking the hallway while tossing a ball back and forth with her caregivers and learned how to safely get in and out of a car.
That final milestone came full circle for St. John, who volunteers with the hospital’s Auxiliary, which helped fund the car simulator she used during therapy.
St. John’s confidence in her care was reinforced by long-standing relationships at Sheridan Memorial Hospital. During her stay, her primary care provider—Internal Medicine physician Dr. Hannah Hall—stopped by while on duty, and hospital staff members St. John recognized from her 17 years of volunteering checked in on her.
Despite receiving care across multiple service lines, St. John said the transition between departments felt smooth and well-coordinated.
“It didn’t feel strange at all,” she said. “Everything felt seamless.”
Today, St. John admits she’s a bit impatient to be fully back to normal, but she’s staying active, considering chair-based exercise classes and continuing to build strength.
Despite the unexpected nature of her injury, St. John looks back on her experience with gratitude. When asked if she would recommend Dr. Laman, her answer was clear.
“Yes,” she said. “Everyone I know who’s broken a hip, he’s done their surgery. He’s busy, but he’s very kind. Very nice.”
For St. John, receiving expert orthopedic care close to home meant healing faster—and staying connected to the family and community she loves, right here in Sheridan.
When injuries interrupt your life, Sheridan Orthopedics is here to help you get back on your feet. Learn more at sheridanortho.com.

At Sheridan Memorial Hospital, serving the community with excellent, patient-centered care often goes far beyond medications, appointments and surgeries. It’s made possible through mentorship, teamwork and generations of shared experience among staff.
Within the Wyoming Rehab team, four “generations” of therapists—Lisa Mohatt, MS, PT, CWS, CLT; Tiffany Sutton, DPT, PT; Justin Bridger, DPT, PT, CSCS; and Dawson Eppe, PTA—represent more than two decades of learning, teaching and passing the torch.
All four are Sheridan natives. Each left to pursue their education and, in time, returned home—bringing with them not only skills and knowledge, but also a commitment to mentorship that continues to shape the culture and expertise of Sheridan Memorial Hospital’s outpatient and inpatient rehabilitation teams.
“We’ve been teachers for each other, and now we’re colleagues,” said Sutton, who has been a physical therapist on the hospital’s Transitional Care Unit (TCU) for the past eight years. “It’s kind of a weird coincidence.”
The mentorship story begins with Mohatt, a physical therapist at Wyoming Rehab’s outpatient clinic, who mentored Sutton when she was a student therapist. Years later, Sutton mentored Bridger, helping him log observation hours and writing a recommendation letter for his application to physical therapy school. Bridger then stepped into that same role for Eppe, mentoring him through his final clinical rotation as he earned his physical therapist assistant license from Laramie County Community College.
Today, Sutton and Eppe work side by side on the TCU floor, while Bridger and Mohatt support patients in Wyoming Rehab’s outpatient clinic—sometimes even treating those who have graduated from Sutton and Eppe’s care.
“It’s been super fun to connect with Tiffany as a colleague and have conversations with her as an equal,” shared Bridger, who has been with Wyoming Rehab since July 2024. “It’s pretty much unheard of to have four generations of therapists in the same organization. I can see how Lisa influenced Tiffany, how Tiffany influenced me and now how I’ve influenced Dawson.”
Each mentor shaped their successor in different ways. Mohatt exposed Sutton to every corner of the field—from outpatient rehabilitation to home health, wound care, and even aquatics. Bridger recalled how Sutton taught him to maintain high standards and recognize that patients are capable of far more than they often realize. When Bridger mentored Eppe, he emphasized adaptability and compassion.
“One of the things Justin hammered into me was that you have to be able to go from rehabbing a hip to, within 30 seconds, switching to a neurological mindset to rehab a stroke,” reflected Eppe, a physical therapist assistant on the TCU floor for the past three years. “His other big lesson was to lead with compassion. You can go from working with a patient having the best day of their life to another having the worst day of their life, and you have to be able to regulate your emotions and meet each patient where they’re at.”
Bridger remembered his time mentoring Eppe fondly, explaining that his goal was to help Eppe see every patient as a unique individual.
“Dawson was able to capture that lesson and make it his own,” Bridger said. “I’m sure he doesn’t treat every patient exactly the way I do—but that’s the point. Take a lesson and make it your own.”
That culture of sharing knowledge and making it one’s own goes both ways. When Eppe joked that he’s still waiting for the day Sutton or Bridger tell him they’ve used one of his exercises, Sutton laughed.
“Are you kidding?” she replied. “I use your hip hinge trick all the time!”
Bridger added that he’s learned something from every student, and that many times, it isn’t clinical knowledge he takes away from mentoring, but insight into different ways to approach and solve problems.
Mohatt agreed, noting that mentorship benefits both teacher and student.
“Mentoring has shown me that each generation has so much to offer, and how important it is to encourage that continued growth so physical therapists can keep helping people more effectively,” Mohatt explained.
The culture of mentorship extends beyond the workplace. Eppe is currently helping Sutton’s daughter recover following hip surgery—a full-circle moment for them both.
And as Eppe begins mentoring his own students, the legacy continues.
“It’s very humbling when you’re asked to teach the next generation,” he said. “When I’m teaching someone, that’s when I feel like I’m at the top of my game, because I have to keep up with the new things students are learning in school, while also showing them what the standard is. It also reminds you how awesome your job is.”
Sutton agreed, adding that growth and curiosity are key to lasting success in the field.
“The moment you think you know it all is when it’s time to hang up your hat,” she said.
Mohatt added that physical therapists play a vital role in a patient’s overall healthcare journey.
“It’s important for physical therapists to truly care about people and their health,” she said. “We need to understand our role in helping patients get better—not just physically, but mentally, as well.”
Together, this multi-generational approach to mentorship and healthcare creates more than professional growth. It fosters a positive, collaborative work environment and strengthens patient care. When knowledge, philosophy and compassion are intentionally passed from one therapist to the next, patients benefit from consistent, thoughtful care throughout their healthcare journey.
“Through community and mentorship, we become more than individuals,” Bridger said. “Through mentorship, we learn our own biases and reframe our thinking, which not only helps the next generation, but also improves care for our patients.”
Learn more about the exceptional care provided through Wyoming Rehab and the TCU at sheridanhospital.org/medical-services/rehabilitation-services/ and sheridanhospital.org/medical-services/transitional-care/.
Are you ready to take the next step in your career and join a workplace that values mentorship, growth and community? Visit sheridanhospital.org/about-us/careers/ to explore current job opportunities and apply today.
Kim DeGraw is the activities director at Sheridan Green House, a long-term care facility operated by Sheridan Memorial Hospital.
Before beginning work as an activities director at Sheridan Green House, I held the same assumptions many people do. Growing older means fewer choices and less freedom. Our bodies protest and our minds tire, so aging must mean a gradual stepping back from the life you once knew. What the elders I work with have taught me, though, is that none of that has to be true.
Aging is about redefining your purpose, not abandoning it.
The elders I see day in and day out want to contribute. They want to set the table, rinse a dish, fold laundry, share a story, teach a card game or offer advice. These may seem like small tasks, but they matter. Purpose doesn’t disappear with age — it just looks a little different.
Elders have also shown me independence is a spectrum. Freedom maybe used to feel like driving on back roads with the windows down, but now it centers around decisions like when to wake up, what to eat, where to sit or how to spend the afternoon. Often elders have more freedom to spend their time how they choose than younger generations in the throes of raising families and working.
While I often remind elders that movement matters, nobody is expecting a marathon. Activity can mean walking, hallway bowling or simply getting up to join a conversation. Staying active, it turns out, is less about the activity itself and more about engagement with the world around you.
This is why mental stimulation is just as important. One of my favorite discoveries has been how powerful curiosity remains later in life. When we explore other cultures, listen to unfamiliar music or talk about places someone has never been, something sparks. Learning doesn’t have an expiration date.
Social connection may be the most powerful lesson of all. Nearly every day, I see meals transform as conversations help bridge the past and present. A single story recalls memories in others and creates a sense of belonging among friends. While so many of us eat meals while scrolling our phones or working at our desks, elders take the time to connect.
There is no denying, though, that aging brings change and often loss. Loss of mobility, loss of memory, loss of loved ones. But elders have taught me about resilience, and shown how much better they adapt when supported. Humor helps, too.
Perhaps the most surprising lesson has come from watching generations connect. Children sitting with elders, reading books, listening to stories, asking questions — these moments matter more than most. Children remind elders that their lives, their memories and their voices carry weight. And elders teach younger generations empathy, patience and perspective.
While these are all important lessons – about independence, activity, social connection, resilience and relevance – the primary thing elders have taught me is that life doesn’t narrow with age unless we let it. Connection, curiosity and joy are available at every stage of life — if we choose to make space for them.
That’s a lesson worth carrying with us, no matter our age.
Hear more from the team at Sheridan Green House. The team appeared on Sheridan Media’s Public Pulse in December. Listen here:

In November 2020, as the world reeled from the effects of the COVID-19 pandemic, Laura Holsinger’s life changed in a far more personal way. Just days after discovering a small, rapidly growing lump in her breast, she underwent a mammogram, ultrasound and biopsy at Sheridan Memorial Hospital. Soon after, Holsinger’s care team confirmed her worst fear: stage two breast cancer.
Up until that point, Holsinger had never faced any major health concerns.
“I’d never spent a night in the hospital or broken a bone, and my family had no history of breast cancer,” she said. “And then boom — all this craziness happened.”
Holsinger had a lumpectomy with Dr. Sara Maguire, MD, FACS, to remove the lump. After surgery, part of the tissue was sent to a lab for an Oncotype DX test — a genomic test that examines the activity of specific genes within cancer cells to estimate how aggressive the cancer might be and how likely it is to spread. Based on the test results, patients receive a score that helps determine whether the potential benefits of chemotherapy outweigh its side effects. For women younger than 50, a score of 25 or lower suggests a low risk of recurrence, meaning chemotherapy is unlikely to provide significant benefit. For women older than 50, a score of 20 or lower indicates the same.
Holsinger’s score was 67.
“Dr. Maguire said it was the highest score she’d seen since joining the hospital,” she recalled.
Holsinger started chemotherapy at the Welch Cancer Center on Feb. 1, 2021. Due to COVID-19 restrictions at the time, patients were not allowed to have visitors or loved ones accompany them to appointments.
“I drove myself to and from appointments,” Holsinger explained. “I was grateful I could get treatment here in town, so then I didn’t have to drive out of town by myself while I wasn’t feeling well.”
Although Holsinger felt grateful to receive care close to home, the experience proved far from easy.
“The only appointment I could bring my husband to was the one where we decided my course of treatment,” Holsinger said. “I can’t tell you how terrified I was the first time I went in for chemo, being surrounded by nurses in what looked like hazmat suits because the medicine was so strong, and realizing they were about to put it in my body.”
Compassionate care team
Despite her initial fear, behind those layers of protective equipment were compassionate caregivers ready to comfort and reassure her every step of the way.
“I appreciate the nurses at the Welch Cancer Center so much,” Holsinger reflected, tears welling in her eyes. “I can’t even describe how comfortable they made me feel, especially knowing I was there alone. They knew I was going through probably the most awful period of my life up to that point, and they were focused on making it the best experience they could despite everything. And they did a really, really good job at that.”
Providing comfort during a patient’s most vulnerable moments is something the nurses at the Welch Cancer Center understand deeply. One nurse reflected on how meaningful it is to support patients through those first, often overwhelming days of treatment.
“I’ve always enjoyed being a patient’s nurse on their first infusion day, so I can give them a sense of security and genuine compassion,” said Lori Karajanis, RN, Oncology Nurse Navigator at the Welch Cancer Center. “It’s what we would all want if it were us in that chair. That is the best part of nursing, in my opinion.”
That compassion made a lasting impression on Holsinger. One of Holsinger’s favorite memories happened on her very first day of treatment. A nurse asked what her favorite colors were, and Holsinger said she preferred “true” colors—more natural, earthy tones.
The nurse disappeared for a few minutes and returned with several other nurses, each holding a handmade quilt donated by a local quilting club. Holsinger chose the quilt that matched the earthy colors she described earlier, and the nurses laughed. It turned out that the nurse who asked about her favorite colors had a knack for picking patients’ favorite blankets—and, as the others joked, she always “won.”
Smiling at the memory, Holsinger added, “That was really nice. Really fun. I didn’t tattle on her. I let her have her glory.”
Her appreciation extended well beyond that single moment and beyond the nursing staff. Holsinger spoke highly of the entire Welch Cancer Center team and the way each person contributed to her care.
“The physicians were always reasonable,” she said. “You’re not just a number to them. You can express your concerns to the providers at the Welch Cancer Center and they listen to you. They talk it out with you and reason on it. Dr. Megan Ratterman, DO, was very good at that. Even over the phone, her voice is so caring and concerned. It’s like talking with a family member.”
That sense of compassion is no accident. It’s woven into the culture of the Welch Cancer Center—something in which the team takes immense pride. Welch Cancer Center Manager Megan Ripley, RN, OCN, explained how deeply teamwork and empathy shape the patient experience.
“Our team demonstrates exceptional compassion for patient-centered care, and teamwork is at the heart of everything we do,” she said. “Patients can truly feel the positive impact of a cohesive and positive work environment when they receive care in our facility.”
Treatment & path forward
Holsinger received chemotherapy from early February through the end of April 2021, followed by 20 rounds of radiation throughout May. Through it all, she worked hard to stay positive.
“My family was terrified,” she admitted. “I was terrified, but I tried really, really hard the whole time to stay positive, because I truly believe the mind can help the body heal.”
Now, five years after her diagnosis and recovery, Holsinger still faces moments of uncertainty. A recent blood test and mammogram have raised concerns that she and her care team continue to monitor closely. Yet even as she faces these challenges, Holsinger does so with remarkable resilience.
“I’m not trying to be paranoid, just proactive,” she said. “And if I have to go through it again, I’m glad I’m here and can go back to the Welch Cancer Center, because I trust them completely. It’s convenient that they’re right here in town, and they’re the best people I know for the job.”
Today, Holsinger is part of Sheridan Memorial Hospital’s Environmental Services and Laundry teams. Recently, she had the opportunity to clean the Welch Cancer Center for the first time since her treatment.
Inspired by the compassion she experienced firsthand at the Welch Cancer Center, Holsinger now gives back by donating a portion of her paycheck to support care there as an Employee Partner of the Sheridan Memorial Hospital Foundation.
“It’s my little way of giving back,” she said.
For Holsinger, being a cancer survivor means more than overcoming an illness. It means gaining a new perspective on life.
“This experience gave me so much empathy,” she explained. “And things aren’t as earth-shattering as they used to be, because you’ve already been through the earth-shattering part. You know you can handle everything else.”
Holsinger has also found purpose in supporting others going through similar experiences.
“I’ve sat with a friend during her first day of chemo because I know how scary it is,” she said. “I was able to encourage her and tell her, ‘You’re going to be OK. I’ve been through this, and I’m still here.’”
For those currently fighting cancer, Holsinger offered simple but powerful advice:
“Just fight, stay positive and kick cancer’s butt.”
For more information about the Welch Cancer Center, visit welchcancercenter.org or call 307.674.6022.

With over 20 years of nursing experience, Kate Winn, MSN, RN, brings expertise, a passion for elder care and a vision for creating a truly home-like environment where residents and caregivers feel supported in her new role as Director of Nursing at Sheridan Memorial Hospital’s long-term care facility, Sheridan Green House.
Over her 23-year nursing career, Winn has cared for patients in settings ranging from emergency departments to refugee health clinics and public health epidemiology. Her work has taken her across the country and around the world, from Oklahoma and Texas to Idaho and Washington state, where she served as an administrator for a dementia and geriatric psychology facility. Most recently, Winn worked as an account manager in long-term care pharmaceuticals before moving to Wyoming, where all six of her children live.
It was during her time working in infection prevention at a nursing home in Gillette that Winn discovered her passion for long-term care.
“I started working infection prevention as a nursing home, and that’s when I really began to fall in love with it,” she said. “You’re literally meeting people where they are. This is their home. And everything you do has an impact.”
To Winn, elder care is both underserved and underappreciated.
“These are the people who made us who we are,” she reflected. “We’ve done such a good job in modern medicine keeping people alive, but we don’t quite know what to do with people when they get old. We’ve gotten people into their 80s, 90s and 100s, but we don’t have a culture that really knows how to embrace that.”
For Winn, one of the most meaningful parts of her work is watching younger staff members interact with residents.
“To see the community of elders and staff interact — to see child-rearing advice, recipes and encouragement shared — is so special,” she said. “The elders have been through it before, so they’re able to offer life advice to the staff that work around them. Seeing generations intermingle is so healthy, and you don’t see that in many areas of healthcare or even in our society.”
Winn was drawn to work at Sheridan Green House because of its unique, cottage-style setting and its use of the Green House Model — an innovative approach to long-term care where elders live in home-like cottages and caregivers provide personalized support, home-cooked meals and meaningful daily routines and activities.
Winn credits Sheridan Green House’s Executive Director Tonya Carlson, BSN, RN, NHA, and former Director of Nursing Dawn Morgan, RN, for laying a strong foundation she’s eager to build upon.
“Because Tonya and Dawn rolled up their sleeves and really got after it, the pieces are all here now to build something that will work well for the elders, the staff and for the community,” Winn praised.
Winn’s main goal as Sheridan Green House’s director of nursing is simple:
“We should be a great place to work and a great place to live.”
Having lived in many rural communities, Winn understands the challenges of sustaining quality healthcare in small towns.
“I’ve seen rural hospitals fail and families drive hours just to see a doctor,” she explained. “For a hospital and nursing home to work together, it’s more than smart business. It’s touching. It means saying to our community, ‘We’ll be your home now.’ That matters.”
When she’s not at work, Winn enjoys spending time outside, collecting and polishing rocks, drawing, painting, writing, knitting and making her own collage paper. She’s also an avid reader, with favorites including “The Odyssey” and “A Tree Grows in Brooklyn”.
Winn describes herself as “approachable and a good listener” and someone who values honesty and trust.
“I can’t solve every problem,” she said. “But I’ll always try to at least bring us to an understanding.”
Sheridan Green House is comprised of four cottages, each with 12 rooms available for residents. If you or a loved one is considering long-term care, reach out to Sheridan Green House at 307.672.0600. For additional information, see sheridangreenhouse.org.
Personalized, confidential care for every stage of life
At the Sheridan Memorial Hospital Women’s Clinic, sexual health is an essential part of your overall wellness. We provide a compassionate, judgment-free space where you can ask questions, seek guidance and receive the care you deserve. Whether you are navigating adolescence, pregnancy, postpartum changes, menopause or anything in between, our team is here to support you with expertise and understanding.
Sexual health concerns can sometimes feel sensitive — but you are not alone. We care for women with these questions every day, and we are committed to listening and providing answers with dignity and respect.
Conditions we evaluate and treat
We offer specialized care for a wide range of sexual health concerns that affect women of all ages.
• Low Libido & Hypoactive Sexual Desire Disorder (HSDD)
Many women experience a decrease in sexual desire at some point in life. If low libido is distressing or affects your relationships, it may be HSDD. Our providers offer:
-
Comprehensive evaluation
-
Hormonal assessments when appropriate
-
Medication options
-
Counseling on contributing factors such as stress, sleep, or relationship changes
-
Personalized treatment plans
• Female Orgasmic Disorder
Difficulties achieving orgasm can be distressing and may stem from physical, hormonal, or psychological factors. We help identify the underlying cause and offer treatment options, education, and referrals when helpful.
• Painful Sex (Dyspareunia)
Pain during intercourse is common — but not something you have to live with. We diagnose and treat many causes, including:
-
Vaginal dryness
-
Hormonal changes
-
Pelvic floor dysfunction
-
Vulvar skin conditions
-
Postpartum or menopause-related changes
-
Infections or inflammation
Treatment may include medications, topical therapies, pelvic floor physical therapy, or changes in routine and habits.
• Vaginal or Vulvar Symptoms
We evaluate and treat:
-
Itching, burning, or irritation
-
Abnormal discharge
-
Recurrent yeast infections
-
Bacterial vaginosis
-
Non-healing lesions
• STI Screening & Treatment
Confidential testing and treatment for:
-
Chlamydia
-
Gonorrhea
-
Trichomoniasis
-
Syphilis
-
HIV
-
Herpes
-
Hepatitis B & C
We provide clear education about safer sex practices, prevention options, and follow-up care.
Additional Sexual Wellness Services
• Contraception & Family Planning
Including birth control pills, patch, ring, injections, IUDs, implants, emergency contraception, pregnancy testing, and preconception planning.
• Menopause & Hormonal Health
Support for changes affecting sexual function, comfort, and well-being—including vaginal dryness, discomfort, and decreased libido.
What to Expect at Your Visit
Your provider will take time to understand your symptoms, concerns, and goals. A typical visit may include:
-
A conversation about your history and experiences
-
A physical exam if needed
-
Testing to help determine the cause of symptoms
-
A personalized treatment plan
-
Follow-up support to help you feel your best
We want you to feel heard, supported, and empowered.
Your Privacy Matters
Sexual health concerns are deeply personal. All appointments, tests, and results are handled with complete confidentiality. You can feel confident seeking care within our small, close-knit community.
Schedule an Appointment
If you’re experiencing low libido, pain, difficulty with orgasm, unusual symptoms, or want STI testing, our Women’s Clinic is here to support your health and wellness.
Call 307.672.2522 today to schedule a visit and take the next step in your sexual well-being.
Specialized care close to home
At Sheridan Memorial Hospital Women’s Clinic, we understand vulvovaginal symptoms can be uncomfortable, disruptive and sometimes difficult to discuss. You deserve care that is private, respectful and focused on getting you answers. Our Women’s Clinic team provides expert evaluation and treatment for a wide range of vulvovaginal conditions — right here in our rural community, close to the people you know and trust.
Conditions we diagnose & treat
Our providers offer comprehensive care for many vulvovaginal conditions, including:
-
Recurrent yeast infections (candidiasis)
-
Bacterial vaginosis (BV)
-
Lichen sclerosus and lichen planus
-
Vulvodynia (chronic vulvar pain)
-
Pelvic floor–related pain
-
Dermatitis or skin irritation
-
Genitourinary Syndrome of Menopause (GSM)
-
Sexually transmitted infections (STIs)
-
Vaginal dryness, itching, or discomfort
-
Painful intercourse (dyspareunia)
-
Abnormal vaginal discharge or odor
-
Non-healing or suspicious lesions
Early evaluation helps us treat symptoms more effectively and rule out more serious concerns.
What to expect at your visit
We work to make every appointment as comfortable as possible. During your visit, your provider may:
-
Discuss your symptoms, medical history and any previous treatments
-
Perform an exam
-
Collect swabs or samples if needed for accurate diagnosis
-
Offer treatment options tailored to your needs, lifestyle and future plans
-
Provide education and guidance on preventing flare-ups or managing chronic conditions
Our goal is to help you understand what’s happening — and to partner with you in creating a personalized care plan that brings relief.
Advanced treatment options
Even in a small community, you have access to treatments often found in larger medical centers, including:
-
Prescription topical and oral medications
-
Hormone and non-hormone therapy
-
Targeted treatments for inflammatory skin conditions
-
Pelvic floor therapy referrals
-
Long-term management plans for chronic vulvar conditions
-
Coordination with dermatology or gynecology specialists when necessary
We believe comprehensive care should be available close to home, without unnecessary travel.
When to seek care
You should schedule an appointment if you experience:
-
Itching, burning or persistent discomfort
-
Pain with sexual activity
-
Changes in vulvar skin color or texture
-
Recurring infections
-
A lump, sore or lesion that does not heal
-
New symptoms after starting a medication or product
-
Symptoms that interfere with daily activities
If you have concerns that feel embarrassing or difficult to talk about, please know we care for these conditions every day—and our team is here to listen without judgment.
Compassionate, confidential care
Your health and comfort matter. Our team at the Women’s Clinic takes the time to answer your questions, explain your options and make sure you feel supported throughout your care.
If you’re experiencing vulvovaginal symptoms, you are not alone—and help is close by.
Call the Sheridan Memorial Hospital Women’s Clinic at 307.672.2522 to schedule your appointment.

When Megan Crocker and her husband, Jeff, moved to Sheridan in 2019, Megan quickly established care at Sheridan Memorial Hospital’s Women’s Clinic. She had been struggling with painful menstrual cycles, unexplained weight gain and other frustrating symptoms.
Unlike past experiences where she was told to simply “diet and exercise,” the Women’s Clinic team listened carefully and worked with Crocker to uncover the true cause: polycystic ovary syndrome (PCOS).
“The providers at the Women’s Clinic were the first to actually listen to me and help diagnose my PCOS,” Megan Crocker said. “Once we decided we were ready to have kids, I tried for over a year with no success.”
Navigating infertility and loss
PCOS made conceiving difficult because Crocker did not have a regular cycle, making ovulation rare and very hard to track. For a months, the Women’s Clinic providers had Crocker try a variety of options to help with ovulation.
“The team always explained the options and helped me know what to expect,” Crocker said. “I am a very plan-oriented person so knowing they had a plan helped me feel comfortable. Getting pregnant with PCOS is a gamble – some get pregnant really easily and some, like me, it just takes time.”
After more than a year of trying, Crocker finally became pregnant — only to experience a heartbreaking miscarriage.
“In that instant my hopes and dreams were shattered,” Crocker said. “The team prepped me for what to expect physically but also made sure to check in on my mental health. They encouraged me to seek counseling, which was one of the most impactful decisions I made for my healing.”
With compassionate care, ongoing support and a clear plan, Crocker found the strength to keep moving forward.
Welcoming Cade
In January 2022, Crocker learned she was pregnant again. The pregnancy itself went smoothly, though anxiety about miscarriage remained a constant challenge.
“The Women’s Clinic team was amazing,” Crocker said. “They would answer any questions I had or when I called with concerns, they would listen. Preparing to be a first-time parent is overwhelming but they ensured we felt prepared.”
Outside the anxiety Crocker felt around another potential miscarriage, this pregnancy progressed without complications.
But at 36 weeks, the baby’s arrival was dramatic. Crocker arrived at the hospital already 8 centimeters dilated, with the baby in breech position. Within 45 minutes, the Sheridan Memorial Hospital team had her in surgery for an emergency C-section.
“I remember having five nurses rapidly working around us to prep me for surgery,” Crocker said. “Even though it was a whirlwind, the team explained everything and kept us calm. We knew we were in good hands.”
After delivery, the Crockers’ son, Cade, faced some health struggles, including unstable glucose levels, but physicians and nurses worked closely to stabilize him, while also supporting Crocker in her postpartum recovery.
Every pregnancy is different
Two years later, the Crockers felt ready to grow their family again. This time, conception was nearly effortless compared to the first journey.
Pregnancy with their daughter, Colbi, brought new challenges, though, including nausea in the first trimester and gestational diabetes. With education, support and close monitoring, Crocker made it through the first trimester and rebounded for the remainder of the pregnancy.
“My biggest concern was whether I would know I was in labor,” Crocker recalled. “With Cade, I had no idea I was in labor and that put us both at risk. I was incredibly stressed that would happen again, but the Women’s Clinic staff and Women’s Health team were incredible with this concern.
“Whenever I thought I was possibly in labor they would either see me in office or in the unit for observation,” Crocker said. “They always said it is not a hassle at all and is always better to be safe. Each time I left the Women’s Health unit I felt confident and at ease Colbi and I were OK.”
While the pregnancy with Cade was easy, his birth was dramatic. For Colbi, the opposite was true. A harder pregnancy challenged Crocker, but the delivery went smoothly.
And, following this scheduled C-section, Crocker was able to stay with her new baby girl and her husband post-surgery, while with her first child — she stayed in recovery with her son while her husband waited in another room. Staying together as a family meant Crocker had her husband by her side the entire time.
Postpartum care
Following the birth of the Crockers’ first child, the Women’s Health team at Sheridan Memorial Hospital ensured Crocker’s pain was managed and helped the couple learn what to expect as new parents.
“You learn so much the first handful of days you have a baby,” Crocker said. “They helped with learning to breastfeed, bathe a baby and even teach you to swaddle, which they all make look so easy. Having nurses you can rely on during these big life changes is key to having an amazing experience.”
Following the birth of the Crockers’ second child in 2025, the Women’s Health team was similarly attentive, but also provided the family with space as needed.
In addition, after her second C-section, an occupational therapist met with Crocker in the hospital to help provide care. They provided tips regarding the best ways to get in and out of bed, support for when the family returned home and more.
“This wasn’t something that was offered after my first child, and it was incredibly helpful, and therefore I had a more successful recovery,” Crocker said.
Gratitude and Trust
Today, Cade — now 2 years old — adores his little sister, Colbi, and the family is thriving. Reflecting on their journey, Crocker credits the Women’s Clinic and Women’s Health teams at Sheridan Memorial Hospital for their expertise, compassion and unwavering support.
“We honestly would not have had our second baby at Sheridan Memorial Hospital if we didn’t trust these teams. They listened, reassured and celebrated every milestone with us,” Crocker said. “Pregnancy is both terrifying and exciting, and having such a well-trained, compassionate team made all the difference.”

Shelley Meier, BSN, RN, CWOCN, is a nurse in the Sheridan Memorial Hospital Wound Care Clinic.
Our skin does a lot of heavy lifting. It protects us from infection, helps regulate temperature and acts as the body’s first line of defense against the world around us. But like the rest of our body, skin changes with age. It becomes thinner, less elastic and often drier. These changes make older adults more vulnerable to wounds, infections and a condition that can have serious health consequences: pressure ulcers.
Pressure ulcers develop when constant pressure reduces blood flow to the skin and underlying tissues. This lack of circulation can damage the skin, leading to painful sores that range from mild redness to deep wounds. The most common places they appear are over bony areas — such as heels, hips, tailbone and elbows.
Prevention is key
The single most important factor in managing pressure ulcers is prevention. Small, daily habits can make all the difference and actions like regular repositioning, skin care and nutrition play a role.
Caring for existing ulcers
Caring for a pressure ulcer requires both local wound management and attention to overall health.
• Relieve pressure: Healing cannot occur if pressure continues on the sore. Use pillows, foam wedges or specialized cushions to keep weight off the affected area. Frequent repositioning — at least every two hours in bed — is vital.
• Clean the wound: Gentle cleansing is the foundation of care. Most ulcers can be cleaned with saline or mild wound cleansers. Harsh antiseptics like hydrogen peroxide or iodine should be avoided unless directed by a healthcare provider, as they can damage healthy tissue.
• Dressings: A clean, moist environment encourages faster healing. Dressings vary depending on the ulcer’s depth and drainage. A nurse or wound specialist can recommend the right choice and help set a schedule for changing them.
• Infection control: Signs of infection include increased redness, swelling, warmth, pus or foul odor. Fever can also be a warning. If infection is suspected, contact a healthcare provider immediately — oral or topical antibiotics may be needed.
• Pain management: Pressure ulcers can be painful, especially during dressing changes. Over-the-counter pain relievers, prescribed medications or topical anesthetics may help improve comfort and tolerance of care.
Support healing from within
The body needs extra support when fighting a wound. Adequate protein, vitamins and hydration strengthen the skin and immune system. For older adults with poor appetite, supplements or dietitian guidance may be beneficial. Good diabetes control and circulation health are also crucial factors.
While prevention is key, if a pressure ulcer does develop, consulting a wound care expert can help ensure a steady path to healing.
To learn more about the Sheridan Memorial Hospital Wound Care Clinic and how we can help you care for and prevent wounds, see sheridanhospital.org/medical-services/wound-care/.

For her 99th birthday, Sheridan Green House resident Vera Montgomery had just one wish: to ride a horse again.
Born in Sheridan in 1926, Vera grew up on a small farm outside of Sundance and has spent nearly a century in the saddle.
“I wasn’t born on a horse, but close to it,” Vera said. “I started riding when I was about 3 years old. I was probably sitting on the saddle horn in front of somebody, but I was riding.”
From riding 2.5 miles to school as a child to working cattle on a ranch in central Montana, horses have always been part of Vera’s life. For 14 years, she and her husband ran a 1,000-head cattle ranch along Currant Creek.
“I was a hired hand, I guess you could say,” Vera recalled. “People tried to put me down and say I was just a housewife, but I told them, ‘I am not a housewife. I am a rancher.’”
After her husband passed away, Vera sold the ranch and returned to Sheridan in 1984 to be closer to her mother. In January 2024, she moved into Sheridan Green House.
That ranching spirit never left her. So, when Sheridan Green House’s Activities Director Kim DeGraw asked what she wanted for her birthday, Vera didn’t ask for cake or decorations. She wanted to get back in the saddle.
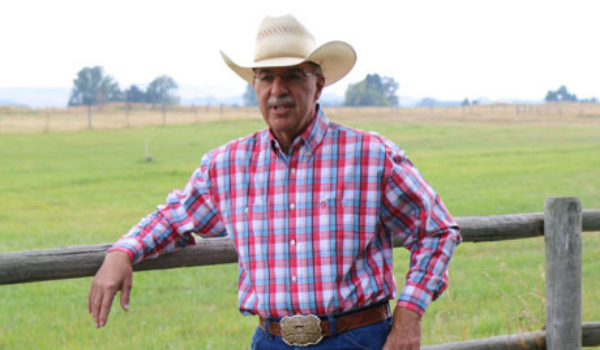
Thanks to the generosity of local rancher and musician Dave Munsick, his wife Trudy and their horse Uno, Vera’s birthday wish came true.
 Dave, Trudy and Uno arrived at Sheridan Green House on a bright June morning. With a little help from licensed practical nurse Kayla Larsen and certified nursing assistant Jennifer Broadwater, Vera climbed into Uno’s saddle. Smiling proudly, she rode Uno around the block while Dave led the way and a crowd of supporters walked beside her.
Dave, Trudy and Uno arrived at Sheridan Green House on a bright June morning. With a little help from licensed practical nurse Kayla Larsen and certified nursing assistant Jennifer Broadwater, Vera climbed into Uno’s saddle. Smiling proudly, she rode Uno around the block while Dave led the way and a crowd of supporters walked beside her.
“It was great,” Vera said afterward. “Once you know how to do it, you never forget.”
Vera’s love for ranch life goes beyond horsemanship. She’s written cowboy poetry since she was 10 year old, inspired by the land and lifestyle she cherishes.
“I put poems under pictures of what I write about,” she said. “I even sold one once for about $20.”

Vera Montgomery holding a photo of herself when she was 13 on horseback at her family’s farm.
After her ride, Vera relaxed on the cottage patio, sharing a photo of herself at 13 on horseback at her family’s farm and reflecting with staff about her childhood and the simpler, tougher times she lived through.
“I wish kids today could understand the kind of life people lived back in the ’20s, ’30s, and ’40s,” she said. “Not necessarily to live it, but just to know what people had to go through.”
She spoke of a time when electricity and telephones were luxuries. A loaf of bread cost eight cents, and a gallon of gas just ten. Children were expected to work in the fields as soon as they were old enough. Boys cut wood to sell in town, and clothing was handed down from neighbors and patched by parents doing their best.
“We didn’t know we were poor,” Vera said. “Everybody was in the same boat. There was no making fun of each other — just neighbors doing what they had to do. It was a hard life, but it was a good life.”
As Dave and Trudy loaded Uno back into the trailer, Vera sat with staff, enjoying the shade and conversation. Kim leaned over and gave her a hug.
“I’m so glad we could make this happen for you,” Kim said. “It was the only thing you wanted for your birthday!”
“And I got it!” Vera beamed.
“You did! You’re 99 years old — you should get what you want! What are we going to do for your 100th birthday next year?”
Without missing a beat, Vera grinned and replied, “Ride a mule.”
At Sheridan Green House, we believe in honoring the lives, passions and independence of every resident—just like Vera. If you’re looking for a place where your loved one can feel truly supported and celebrated, we invite you to connect with us. Call 307.672.0600 or visit sheridangreenhouse.org to learn more.


After years of chronic ankle pain, Judy Merriott, DVM, reached a point where everyday tasks—and even walking—became unbearable. Working as an equine veterinarian felt impossible, and the activities she once loved were now out of reach. Determined to get back in the saddle, both literally and figuratively, Judy turned to Sheridan Orthopedics, where she found the care and support she needed to reclaim her mobility and joy.
Judy has called Sheridan home for the past year, returning to Wyoming after spending 12 years practicing veterinary medicine in Australia. Her ankle pain began about five years ago, following an injury she sustained while working abroad.
“I was doing chiropractic work on a horse and standing on a stepladder,” Judy recalled. “I was up above this mare’s neck, and the person holding her wasn’t paying much attention. The mare jumped sideways, knocked me off the ladder and stepped on my ankle.”
Although initial X-rays showed no broken bones, the damage worsened over time. The pain gradually began to affect every part of her life.
“I was a solo practitioner, so I didn’t get much time off,” she explained. “I soldiered on, but every year it got a little worse. Eventually, I was walking with my foot turned out like a duck because that was the only position that felt comfortable. When I moved to Sheridan, I knew that if I still wanted to work as an equine vet, I needed my mobility back. I have to be able to get out of the way quickly if my patient—the horse—isn’t happy with me.”
Judy’s pain didn’t just affect her work. It also kept her from enjoying her favorite pastimes.
“I like to hike, and I love to ride horses,” she shared. “I tried to ride last summer, but I ended up getting of the horse in tears because my ankle hurt so much.”
Eager for a solution, Judy researched providers in Sheridan, Billings and Denver. She eventually met with Dr. Daniel Peterson, DPM, FACFAS, at Sheridan Orthopedics, who introduced the possibility of a total ankle replacement.
After speaking with others in the community and hearing consistent praise for Dr. Peterson’s expertise and kindness, combined with the convenience of receiving care close to home, Judy felt confident moving forward with the procedure.
From her first visit to her final follow-up, Judy felt heard, respected and supported throughout the process.
“The front desk staff were very friendly and efficient,” Judy said. “And the scheduler was great, even when I had to postpone my surgery twice. Any time I had a concern, I could call the office, and Dr. Peterson would personally call me back.”
Her experience stood in stark contrast to a previous major surgery.
“I had both knees replaced in 2008 in Colorado. The surgeon was well-known, but I felt like I was just a blip on their screen,” she said. “Dr. Peterson never made me feel that way. I felt very well taken care of.”
In December 2024, Sheridan Orthopedics became part of the Sheridan Memorial Hospital team, enhancing the hospital’s ability to deliver expert, coordinated orthopedic care close to home. This integration ensures patients like Judy receive a smooth, supportive experience—from initial consultation through surgery and recovery—guided by a team that puts people first.
Judy’s surgery went smoothly, and she spent one night at Sheridan Memorial Hospital—a stay that left a lasting impression.
“The nurses were wonderful,” she reflected. “When you’re a patient, someone else has to help you do everything—and they were kind, respectful and never made me feel awkward.”
Now, several weeks into her recovery, Judy has made remarkable progress—enough to impress even Dr. Peterson.
“At my two-week check-up, my incisions had already healed really well,” she said. “By four weeks, Dr. Peterson looked at my X-rays and range of motion and said, ‘I’m really surprised. I’ve never seen an ankle heal this quickly.’”
Judy chuckled. “And I said to him, “I told you I was a good healer!”
She continues physical therapy and is eager to walk again without a boot or crutch, but she’s also learning to listen to her body.
“I have a tendency to push through things,” Judy admitted. “A few days ago, I felt strong enough to go for a walk with my neighbor, but on the way back, it started to hurt. I’m learning to listen to my ankle and know when it’s had enough. I’m trying to do everything I can to make it heal quickly, but at the same time, I don’t want to overextend myself.”
When asked what advice she would give others considering ankle replacement, Judy answered, “Number one, go to Dr. Peterson. Number two, trust your doctor. Make a list of your questions and concerns, and just go have a conversation.”
In just a few more weeks, Judy hopes to be hiking the Bighorns with her Border Collie and, eventually, riding horses again.
“I’ll be thrilled the first time I get back on a horse,” she said with a smile. “I’ll be thrilled, because that was my life for many, many years.”
If bone, joint or muscle pain is keeping you from the things you love, you don’t have to go through it alone. Visit sheridanortho.org to learn how Sheridan Orthopedics can help you get back in the saddle and back to doing what you love.
When you don’t know what “normal” should look like, you learn to cope with the hand you’ve been dealt. For 35-year-old Danielle Law, that meant years of painful cramps, difficult menstrual cycles and hormones that fluctuated through extremes.
After giving birth to three boys, though, Danielle sought help figuring out what “normal” could mean for her. She worked with a functional healthcare provider who started her on supplemental hormones, but a year into that treatment Danielle knew something still wasn’t right.
“I did a lot of research,” Danielle said of that timeframe, adding that she adjusted her diet and implemented healthier habits. “I felt the best that I’ve felt in my entire life.”
About five months ago, though, her menstrual cycles returned more regularly and they were just as frustrating as they had been before she had children.
“My mom had a hysterectomy after years of dealing with endometriosis,” Danielle said. “After everything I had tried and how good I had felt, the return to that cycle of pain – I knew something was wrong. So, I called the Women’s Clinic and let them know I wanted to be checked for endometriosis.”
 Danielle said she was scheduled quickly, and sat down with Dr. Lindsay Capron to discuss her symptoms.
Danielle said she was scheduled quickly, and sat down with Dr. Lindsay Capron to discuss her symptoms.
“In all of my research, I had read horror stories about women spending years advocating for themselves and arguing with doctors about their symptoms,” Danielle said. “I didn’t have that experience at all. Dr. Capron listened to me, believed me and got to work trying to help me figure it out.”
Dr. Capron said many women are suffering with severe pain and heavy bleeding, thinking it’s normal, or worse, feeling like they are just complaining and unable to cope.
Danielle was diagnosed with adenomyosis, a condition where the tissue that normally lines the uterus grows into the muscular wall of the uterus, causing heavy menstrual bleeding and pelvic pain. It can get progressively worse with each menstrual cycle and each pregnancy.
Dr. Capron provided Danielle with several options for treatment, including ablation, hormonal treatment and hysterectomy. The hospital’s use of robotics also allows surgeons like Dr. Capron to offer excision of endometriosis as an option for treatment.
Dr. Capron noted that whether a woman is 20 or 90, the decision to pursue hysterectomy is very individualized. She and the other providers at SMH’s Women’s Clinic are available to discuss all options with patients to help find a solution that meets their needs and desires.
 “It sounded terrifying at first,” Danielle said of hysterectomy. “Dr. Capron reassured me that I didn’t have to decide right away. So I did more research – I mean these days you can research to your heart’s content.”
“It sounded terrifying at first,” Danielle said of hysterectomy. “Dr. Capron reassured me that I didn’t have to decide right away. So I did more research – I mean these days you can research to your heart’s content.”
She noted that her initial concerns centered around hormones, which she had spent so many years trying to regulate and control. Ultimately, though, Danielle opted for the hysterectomy, keeping her ovaries, knowing she was at her healthiest and excited to see an end to the pain she had endured for decades.
She was scheduled for the surgery and within two weeks Dr. Capron had utilized robotic technology at SMH to complete the procedure, leaving just four small incisions on Danielle’s abdomen and shortening the recovery time.
To celebrate the surgery, Danielle even recorded a short video of herself dancing in her hospital gown after surgery.“I wanted to show everyone that I was OK,” Danielle said.
Little did she know that one short post celebrating her choice would go viral, as women across the country empathized with her situation and celebrated that more and more options are becoming available to help women manage their menstrual cycles, pain and hormones.
“So many women were looking for information,” Danielle said of the post that went viral. “I had comments that included everything from ‘thank you’ to questions about the process, horror stories about doctors that wouldn’t listen and women saying they had done the same and never regretted it. It was wild.”
Since then, Danielle has continued sharing her story on social media, giving updates on how she’s feeling, helping women understand her journey and the options available.
A couple weeks post-surgery, Danielle had a follow-up appointment with Dr. Capron, where the WOMC provider confirmed the adenomyosis diagnosis along with endometriosis and fibroids.
“It was reassuring that I felt like I made the right decision,” Danielle said. “I feel great, almost so good that I wonder what I’m missing.”
While Danielle is still only about eight weeks post-surgery, she said she’s excited to settle into what her new “normal” will look and feel like – with less pain and an increased appreciation for her health heading into her 40s.
If you’re struggling with pain or symptoms that don’t feel “normal,” you don’t have to face it alone. The experienced team at Sheridan Memorial Hospital’s Women’s Clinic is here to listen, support, and help you find real answers. Your health matters—and so does your story. If you would like to make an appointment call or text 307.672.2522.

At Sheridan Memorial Hospital Women’s Clinic, our OB/GYN team partners with you throughout your pregnancy — offering compassionate prenatal care, personalized delivery support and follow-up to give you and your baby the healthiest possible start.
From your first prenatal visit to the moment you meet your baby, our goal is to ensure a safe, supportive and positive birth experience.
Why prenatal care matters
Prenatal care is the ongoing medical support you receive during pregnancy. Regular visits allow your provider to:
- Monitor your health and your baby’s development
- Detect and address potential complications early
- Provide education, resources, and emotional support
- Help you prepare for delivery with confidence
Every pregnancy is unique, and consistent care gives your baby the best possible beginning—whether it’s your first pregnancy or your fifth.
When to schedule prenatal care
It’s best to schedule your first prenatal appointment as soon as you suspect you’re pregnant—usually around 8 weeks (four weeks after a missed period).
A typical prenatal care schedule includes:
- Weeks 4–28: one visit per month
- Weeks 28–36: two visits per month
- Week 36 until delivery: one visit per week
If your pregnancy is considered high-risk, you may need more frequent visits for closer monitoring.
What to expect during prenatal visits
At your first visit, your provider will:
- Review your health history and check vital signs
- Estimate your due date
- Perform a physical exam, including a pelvic exam
- Listen for the baby’s heartbeat
- Order early blood tests and screenings
In later visits, you may have:
- Ultrasounds to monitor growth and development
- STD screenings
- Glucose tolerance testing for gestational diabetes
- Urinalysis to screen for preeclampsia
- Genetic testing, amniocentesis, or chorionic villus sampling (as needed)
- Group B strep culture in the third trimester
- Fetal monitoring
Delivery support and birth planning
As your due date approaches, your provider will work with you to create a birth plan that aligns with your preferences, health needs, and baby’s well-being.
Our team is committed to supporting your vision for labor and delivery—while being fully prepared to respond quickly and safely if unexpected complications arise.
Call today to schedule your first prenatal visit and begin your personalized pregnancy care plan.

An ultrasound screening is a safe, noninvasive way for your provider to evaluate your reproductive organs or monitor a developing pregnancy. At Sheridan Memorial Hospital Women’s Clinic, we offer convenient, in-office ultrasound services so you don’t have to travel elsewhere for diagnostic imaging.
Call Sheridan Memorial Hospital Women’s Clinic today to schedule your ultrasound.
What is an ultrasound?
An ultrasound uses high-frequency sound waves to create detailed images of the tissues and organs inside your body. It does not use radiation, making it a safe option for reproductive and prenatal care.
During the test:
- A technician glides a handheld wand (transducer) over your abdomen.
- Sound waves bounce off your internal structures.
- These echoes create real-time images on a computer screen.
Sometimes, your provider may perform a transvaginal ultrasound by placing a sterile wand inside the vagina. This approach provides clearer images of the uterus and surrounding structures when needed for diagnosis.
What does an ultrasound detect?
Ultrasound imaging helps your provider examine reproductive organs such as the uterus, ovaries, cervix, and fallopian tubes. It can also be used to evaluate the bladder or assess fetal growth during pregnancy.
Common reasons you may need an ultrasound include:
- Detecting ovarian cysts
- Measuring and locating uterine fibroids
- Evaluating causes of pelvic pain or irregular bleeding
- Monitoring a pregnancy and assessing fetal development
What types of ultrasounds are offered?
Your provider recommends the most appropriate type of ultrasound based on your health needs. Options include:
- Transabdominal ultrasound – The standard exam, where the wand is moved across your lower abdomen.
- Transvaginal ultrasound – The wand is placed inside the vagina to capture a more detailed view of the uterus and ovaries.
- Transperineal or translabial ultrasound – Performed externally on the genital area to evaluate urinary or pelvic conditions.
Some women may undergo both abdominal and vaginal ultrasounds for a more complete picture of the pelvic region.
What are the benefits of an ultrasound?
Ultrasounds provide several advantages for both patients and providers:
- Safe, noninvasive, and radiation-free
- Real-time images of your internal organs or developing baby
- In-office availability at Sheridan Memorial Hospital Women’s Clinic—no need to travel to another facility
- Immediate interpretation by your provider so you can receive results and treatment quickly
In-office women’s ultrasound care in Sheridan
At Sheridan Memorial Hospital Women’s Clinic, our team provides high-quality, compassionate care for women’s health needs, including advanced imaging. Whether you need a diagnostic pelvic ultrasound or a prenatal checkup, you can trust our providers to deliver expert care close to home.
Call today to schedule your ultrasound and learn more about women’s imaging services.

Endometriosis is a common women’s health condition, especially for women in their 30s and 40s. It occurs when the lining of the uterus (endometrial tissue) grows outside the womb in places like the ovaries, rectum or bladder. This misplaced tissue can cause painful periods, irregular bleeding and fertility challenges.
At Sheridan Memorial Hospital Women’s Clinic, our experienced providers offer expert diagnosis and treatment options to help you find relief and protect your long-term reproductive health.
Call our office today to schedule an evaluation if you suspect you may have endometriosis.
What are the symptoms of endometriosis?
Endometrial tissue that grows outside the uterus still responds to monthly hormonal changes—thickening, breaking down, and bleeding. Because this tissue has no way to leave the body, it can lead to inflammation, pain, and scarring. Common symptoms include:
- Painful, heavy, or irregular periods
- Cramps that last longer than normal (sometimes weeks)
- Chronic pelvic, abdominal, or lower back pain
- Pain during sex or bowel movements
- Difficulty getting pregnant (30–40% of women with endometriosis experience infertility)
Endometriosis is most often diagnosed in women between ages 25 and 35, but symptoms may begin earlier.
Who is at risk of developing endometriosis?
Any woman of childbearing age can develop endometriosis, but your risk is higher if you:
- Have a first-degree relative (mother, sister) with endometriosis
- Began menstruating at a young age
- Have never been pregnant
- Have short or frequent menstrual cycles
- Experience periods that last more than seven days
- Have an immune system condition
If you have these risk factors and symptoms, the team at Sheridan Memorial Hospital Women’s Clinic encourages you to schedule an evaluation for accurate diagnosis and personalized care.
What are the treatment options for endometriosis?
While there is no permanent cure for endometriosis, treatments can effectively manage symptoms and improve quality of life. Your provider will create a customized treatment plan based on your age, family plans, overall health, and the severity of your symptoms. Options may include:
- Over-the-counter or prescription pain medications
- Relaxation and stress-reduction techniques
- Hormone therapy (birth control pills, progesterone therapy, or hormone injections)
- Fertility treatments if you are trying to conceive
- Minimally invasive surgery to diagnose and remove abnormal tissue
- Hysterectomy (in severe cases when other treatments aren’t effective and pregnancy is not desired)
Early diagnosis and treatment can help prevent complications, improve fertility outcomes, and provide much-needed relief.
Expert endometriosis care in Sheridan
You don’t have to suffer in silence. At Sheridan Memorial Hospital Women’s Clinic, our caring providers are here to listen, support, and guide you through effective treatment options for endometriosis.
Call today to schedule your endometriosis evaluation and start your path to relief.

Well-woman exams are an essential part of preventive health care for women at every stage of life. At Sheridan Memorial Hospital Women’s Clinic, our compassionate providers make your annual exam as comfortable and straightforward as possible. These visits offer an overall assessment of your health with an extra focus on breast and gynecologic health.
Call Sheridan Memorial Hospital Women’s Clinic today to schedule your well-woman.
What is a well-woman exam?
Depending on your age, health history and risk factors, your provider may:
- Screen for breast, cervical, vulvar, vaginal, colon, lung, skin cancers, etc.
- Screen or provide guidance to prevent infectious disease such as hepatitis, HIV, tuberculosis and STDs
- Conduct a bone health assessment, and prevention of osteoporosis
- Screen for heart health sand provide referrals as needed
- Provide mental health screenings and referrals when needed
- Evaluate and help manage of urinary incontinence
- Help prevent pregnancy
- Assist with fertility
- Provide pre-pregnancy counseling
- Provide menopause and perimenopausal care
- Provide a breast cancer risk assessment and discussion on breast cancer prevention options
- Discuss genetic testing for genes associated with breast or ovarian cancer
- Offer screening and referrals for substance and tobacco use disorders,
- Assess and help manage infertility
- Discuss and address menstrual irregularities
- Update immunizations
- Assess issues of intimate partner violence
The team at Sheridan Memorial Hospital’s Women’s Clinic are your full partners in healthcare. We are here to connect you with any additional resources you made need in your healthcare journey. Well-woman exams offer a thorough health evaluation and assessment.
How should I prepare for my annual exam?
Before your visit, be ready to share your:
- Personal medical history (pregnancies, surgeries, health conditions)
- Family medical history
- Current medications and dosages
Your provider may also ask questions such as:
- When was your last menstrual period?
- How long do your periods typically last?
- At what age did you start menstruating?
- Are you currently sexually active?
Having this information helps your doctor provide the most personalized care.
What happens during a well-woman exam?
Our providers will explain each step so you know what to expect.
- Breast exam – To check for lumps or changes that may indicate breast cancer.
- Pelvic exam – Speculum and bimanual exam as well as an external examination.
- Pap smear – A swab of cervical cells to test for cancerous or precancerous changes.
- Bimanual exam – Your provider checks your uterus, ovaries, and fallopian tubes.
This exam provides a complete picture of your gynecologic health and is a key step in preventive women’s health care.
What conditions can a well-woman exam detect?
Most patients leave with no concerns. However, well-woman exams sometimes detect early signs of conditions such as:
- Urinary incontinence
- Breast, colon, cervical, vulvar, vaginal, uterine, skin, lung and other cancers
- Vulvar and vaginal conditions
- Sexual health conditions such as hypoactive sexual desire disorder, female orgasmic disorder or painful sex
- PCOS
- Pelvic floor dysfunction
- Menstrual problems including endometriosis, adenomyosis, ovarian cysts, uterine fibroids
- Pelvic infections
Early detection means earlier treatment and better outcomes.
Expert women’s health care in Sheridan
At Sheridan Memorial Hospital Women’s Clinic, our experienced team combines advanced technology with personalized, compassionate care. Whether you need routine screenings, family planning, or treatment for a health concern, you can trust us to support your long-term well-being.
If you’re due for your annual well-woman exam, call Sheridan Memorial Hospital Women’s Clinic today to schedule an appointment.

Cancer screenings are an important part of women’s preventive health care. At Sheridan Memorial Hospital Women’s Clinic, our providers offer routine cervical and breast cancer screenings — including Pap smears and mammograms—as well as screenings for lung, colon, cervical and other types of cancer. We also offer advanced genetic testing for women with higher risk due to family history.
Early detection saves lives. Regular screenings can help identify cancer at its most treatable stages, giving you the best chance for a healthy future.
What is cancer screening?
Cancer develops when abnormal cells grow uncontrollably. Screenings are preventive tests designed to detect these changes before symptoms appear.
Since cancer is the second leading cause of death worldwide, routine screenings play a critical role in early detection and treatment.
Types of cancer screenings for women
Our clinic provides comprehensive cancer screening services, including:
Cervical cancer screening
- Pap smear: During a pelvic exam, your provider collects cervical cells to check for abnormalities and early signs of cancer. Women should begin Pap smears at age 21.
- HPV test: Human papillomavirus (HPV) is a common sexually transmitted infection that can increase the risk of cervical cancer. Screening for HPV usually starts at age 30. If both Pap smear and HPV tests are negative, you may only need screening every five years.
Breast cancer screening
- Clinical breast exam: At your annual well-woman visit, your provider checks breast tissue for lumps or abnormalities. You’ll also be encouraged to perform monthly self-breast exams at home.
- Mammogram: Starting around age 40, mammograms are recommended to detect breast changes not felt during an exam. This low-dose X-ray can detect breast cancer in its earliest stages.
Genetic (hereditary) cancer screening
Some women may be at higher risk of breast or cervical cancer due to family history or genetic mutations. Our clinic offers heritage cancer screening to identify inherited risk factors such as the BRCA1 and BRCA2 “breast cancer genes.”
If genetic testing shows you have a higher risk, your provider will create a personalized screening and prevention plan tailored to your needs.
Take the next step
Routine cancer screenings are one of the best tools for prevention and early detection. Whether you need a Pap smear, mammogram, or genetic cancer risk evaluation, our team at Sheridan Memorial Hospital Women’s Clinic provides the expert, compassionate care you deserve.
Call today to schedule your cancer screening appointment.

An abnormal Pap smear doesn’t necessarily mean you have cervical cancer. To better understand your results, your provider may recommend a colposcopy — a simple, in-office procedure that allows for a closer look at the cervix.
At Sheridan Memorial Hospital Women’s Clinic, our OB/GYN specialists perform colposcopy exams to detect cervical changes early, provide answers, and guide you to the right next steps.
What is a colposcopy?
A colposcopy is a gynecological procedure used to examine the vulva, vagina, and cervix for abnormalities.
Your provider uses a colposcope — a magnifying instrument with a light — to detect changes in cervical tissue that are not visible to the naked eye. If needed, a small biopsy (tissue sample) can be taken during the procedure for lab testing.
Why might I need a colposcopy?
The most common reason for a colposcopy is to follow up on abnormal Pap smear results. However, your provider may also recommend the procedure to evaluate:
- Cervical inflammation (cervicitis)
- Genital warts
- Suspicious or precancerous cervical tissue changes
Colposcopy helps confirm or rule out more serious conditions, including cervical cancer, at an early and treatable stage.
What happens during a colposcopy?
A colposcopy is performed in-office and typically takes about 15–20 minutes. Here’s what to expect:
- You’ll lie on the exam table in the same position as a pelvic exam.
- A speculum is inserted to gently open the vaginal walls.
- The colposcope is positioned just outside the vagina to magnify the cervical tissue.
- A mild solution is applied to highlight any abnormal cells.
- If needed, a biopsy of suspicious tissue is taken.
Most women feel no pain, though a biopsy may cause a brief pinch or cramping sensation.
What to expect after a colposcopy
- If no biopsy is taken, you can resume normal activities right away.
- If you had a biopsy, you may experience light bleeding, spotting, or mild cramping for a few days. Your provider may recommend avoiding tampons and sexual activity for about a week.
Take the next step
A colposcopy is a safe and effective way to better understand abnormal Pap smear results and protect your long-term health.
For expert, compassionate women’s care, call Sheridan Memorial Hospital Women’s Clinic today to schedule your appointment.

Sometimes surgery is the best option to treat gynecological issues such as irregular uterine bleeding, pelvic pain, fibroids, or endometriosis. At Sheridan Memorial Hospital Women’s Clinic, our experienced surgeons specialize in minimally invasive and robotic-assisted surgery to deliver precise results with faster recovery times.
What is minimally invasive surgery?
Minimally invasive surgery uses small incisions, specialized instruments, and advanced technology to treat gynecological conditions while reducing trauma to the body.
Compared to traditional open surgery, which requires a large abdominal incision, minimally invasive techniques such as laparoscopy and robotic surgery (da Vinci platform) offer:
- Smaller incisions with less scarring
- Reduced blood loss
- Lower risk of infection
- Shorter (or no) hospital stays
- Faster recovery and return to normal activities
- Greater surgical precision and control
Whenever possible, our surgeons use minimally invasive techniques—but in certain complex cases, open surgery may still provide the safest outcome.
Types of minimally invasive surgery we offer
Our clinic provides a wide range of advanced gynecologic procedures, including:
Laparoscopic surgery
A laparoscope (a thin tube with a light and camera) is inserted through small incisions to project images of your reproductive organs onto a screen. This allows surgeons to diagnose and treat conditions such as:
- Endometriosis
- Ovarian cysts or masses
- Fibroids
- Hysterectomy procedures
Hysterectomy
Our surgeons have more than 50 years of combined experience performing minimally invasive hysterectomies for conditions such as chronic pelvic pain, uterine prolapse, cancer, and abnormal bleeding. Options include:
- Laparoscopic-assisted vaginal hysterectomy (LAVH): Removes the uterus, and possibly fallopian tubes/ovaries
- Total laparoscopic hysterectomy (TLH): Removes the uterus and cervix
- Vaginal hysterectomy: Removes the uterus through the vagina, avoiding abdominal incisions
Because a hysterectomy triggers menopause, our team also provides ongoing support and treatment for symptom management.
Endometrial ablation
A quick, minimally invasive procedure that destroys the uterine lining to stop or reduce heavy menstrual bleeding.
Fibroid and polyp removal
A specialized hysteroscope is used to remove abnormal tissue causing pain or heavy bleeding—typically completed in about 30 minutes.
Myomectomy
A surgical procedure to remove fibroids while preserving the uterus, ideal for women who want to maintain fertility. This can be performed laparoscopically or with robotic assistance.
Take the next step
If you need gynecologic surgery, you deserve the most effective care with the least disruption to your life. At Sheridan Memorial Hospital Women’s Clinic, our minimally invasive and robotic-assisted procedures are designed to provide safe, precise treatment with a quicker recovery.
Call today to schedule a consultation with our surgical team and explore your options.

If you’re experiencing abnormal uterine bleeding or other gynecological concerns, your provider may recommend a hysteroscopy. This minimally invasive procedure allows your OB/GYN to look inside your uterus, diagnose problems, and in some cases, perform treatment during the same visit.
At Sheridan Memorial Hospital Women’s Clinic, our women’s health experts use hysteroscopy to provide accurate diagnoses and effective treatment with minimal downtime.
What is a hysteroscopy?
A hysteroscopy is a gynecological procedure that uses a thin, flexible tube called a hysteroscope. The device has a light and camera that transmit images to a screen, allowing your provider to clearly evaluate the uterus.
There are two main types of hysteroscopy:
- Diagnostic hysteroscopy – Used to examine the uterus and identify causes of abnormal bleeding, infertility, or other issues.
- Operative hysteroscopy – Combines diagnosis and treatment. Your provider may remove fibroids or polyps, perform an endometrial ablation, or locate an intrauterine device (IUD).
Why might I need a hysteroscopy?
Your provider may recommend a hysteroscopy to:
- Identify the cause of abnormal or heavy bleeding
- Evaluate recurrent miscarriages during an infertility workup
- Locate or remove an intrauterine device (IUD)
- Treat fibroids, polyps, or other uterine abnormalities
What happens during a hysteroscopy?
The details of your procedure depend on whether it is diagnostic or operative. In general, you can expect:
- Sedation or anesthesia to help you relax
- Cervical dilation using medication or a device
- Insertion of a speculum and then the hysteroscope
- Filling the uterus with fluid to improve visibility
- Examination and, if planned, treatment of any abnormalities
Recovery after a hysteroscopy
Most patients go home the same day. You may experience:
- Mild cramping
- Bloating
- Light spotting
Your provider may recommend avoiding sexual activity or strenuous exercise for up to two weeks while you heal.
Take the next step
A hysteroscopy is a safe, effective procedure that can both diagnose and treat common gynecological conditions with minimal downtime.
Call Sheridan Memorial Hospital Women’s Clinic today to schedule an appointment and learn whether hysteroscopy is right for you.

When it comes to birth control, women have more choices than ever. At Sheridan Memorial Hospital Women’s Clinic, our OB/GYN specialists provide personalized contraception counseling to help you select the method that best fits your health, lifestyle, and family planning goals.
What is birth control?
Birth control — also called contraception — refers to any method, device, or medication used to prevent pregnancy. Beyond pregnancy prevention, some birth control methods can also help regulate periods, reduce menstrual cramps, or treat conditions like endometriosis.
Types of birth control
We offer a wide range of options, including:
- Birth control pills – Daily oral medication containing estrogen and/or progestins to prevent ovulation, and just like the patch can be used to help regulate cycles and treat other gynecologic conditions
- Intrauterine devices (IUDs): Long-acting, reversible contraception placed in the uterus. Options include hormonal and non-hormonal (copper) IUDs, effective for up to 10 years.
- Nexplanon® implant: A small, hormone-releasing device inserted under the skin of the arm, effective for up to 3 years.
- Birth control patch: Worn on the skin, releases hormones to prevent ovulation. Also used to help regulate cycles and reduce painful periods.
- Vaginal ring: A flexible, hormone-releasing device placed in the vagina and replaced monthly.
- Diaphragm: A dome-shaped barrier device placed over the cervix to block sperm. Our providers offer professional fittings to ensure proper placement.
- Condoms: A barrier method that prevents pregnancy and also protects against sexually transmitted infections (STIs), including HIV.
- Tubal ligation: A permanent surgical option in which the fallopian tubes are blocked to prevent pregnancy.
Choosing the right method
The best birth control method depends on factors such as your age, health history, lifestyle, and whether you plan to have children in the future. During your visit, our providers will:
- Review your medical history and preferences
- Discuss the pros and cons of each method
- Provide prescriptions or perform in-office procedures as needed
- Offer STD testing and prevention counseling when appropriate
Take the next step
Whether you’re looking for short-term contraception, a long-lasting reversible option, or permanent birth control, our women’s health experts are here to guide you.
Call Sheridan Memorial Hospital Women’s Clinic today to schedule a consultation and explore your birth control options.

Polycystic ovary syndrome (PCOS) is one of the most common hormonal disorders, affecting 5–10% of women of childbearing age. PCOS impacts ovulation, fertility, and overall health—but with the right care, symptoms can be managed effectively.
At Sheridan Memorial Hospital Women’s Clinic, our women’s health specialists diagnose and provide personalized treatment plans to help you take control of PCOS and improve your quality of life.
What is PCOS?
PCOS is a hormonal imbalance that affects how the ovaries function. Women with PCOS often produce higher-than-normal levels of androgens (male hormones), which can disrupt ovulation and cause a wide range of symptoms.
Symptoms of PCOS
PCOS symptoms vary, but common signs include:
- Irregular or absent periods
- Excess hair growth on the face, chin, or body (hirsutism)
- Weight gain and difficulty losing weight
- Acne or oily skin
- Hair thinning or male-pattern baldness
Importantly, PCOS is a leading cause of infertility due to irregular ovulation.
How PCOS is diagnosed
Diagnosis begins with a full medical history, physical exam, and pelvic exam. Your provider may also:
- Order blood tests to check hormone levels
- Perform a pelvic ultrasound
- Discuss menstrual history
- Review family history, since PCOS often has a genetic link
PCOS treatment options
There is no cure for PCOS, but symptoms can be managed and fertility often restored with the right care. Treatment is customized based on your goals, such as improving symptoms, regulating cycles, or achieving pregnancy.
Lifestyle support
- Weight management through healthy diet and regular exercise
- Blood sugar management to reduce insulin resistance
Medications
- Birth control pills to regulate menstrual cycles and improve acne
- Fertility medications to stimulate ovulation
- Metformin to improve insulin sensitivity
Fertility support
If pregnancy is your goal and medications aren’t effective, advanced options like in vitro fertilization (IVF) may be recommended.
Cycle regulation with hormones
Management of hair growth, hair loss and acne
PCOS also affects metabolism, increasing the risk of:
- Weight gain or difficulty losing weight
- Insulin resistance
- Type 2 diabetes
Take the next step
PCOS is a common condition—but it doesn’t have to control your health or your future. With early diagnosis and a personalized treatment plan, many women successfully manage symptoms and achieve healthy pregnancies.
If you’re struggling with PCOS symptoms or infertility, call Sheridan Memorial Hospital Women’s Clinic today to schedule an appointment.
Menopause is a natural life stage that marks the end of a woman’s fertility. While it is normal, the hormonal changes that occur during perimenopause and menopause can cause disruptive symptoms that affect quality of life.
At Sheridan Memorial Hospital Women’s Clinic, our women’s health specialists provide compassionate, patient-centered care to help you manage symptoms and protect your long-term health.
What is menopause?
Menopause occurs when your ovaries reduce production of estrogen and progesterone—the hormones that regulate your menstrual cycle—and you have gone 12 consecutive months without a period.
Most women naturally reach menopause between ages 45 and 55. However, the transition happens gradually, beginning with a stage called perimenopause.
What is perimenopause?
Perimenopause can last months or even years before menopause. During this time, hormone levels fluctuate, often causing:
- Worsening PMS (most common first symptom)
- Brain fog
- Irregular or skipped periods
- Heavier or lighter bleeding than usual
- Symptoms associated with menopause, such as hot flashes or sleep disturbances
A gap of 60 days or more between periods may signal that you are approaching menopause.
Symptoms of menopause and perimenopause
Symptoms vary in severity and duration, but common ones include:
- Hot flashes and night sweats
- Difficulty sleeping or insomnia
- Memory issues or forgetfulness
- Mood swings or irritability
- Vaginal dryness
- Low libido
- Joint and muscle aches and pains
- Dysuria (painful urination)
After reaching postmenopause, many symptoms gradually improve, but low estrogen levels increase the risk of conditions such as osteoporosis.
Treatment options for menopause
Our team develops personalized treatment plans based on your symptoms, health history, and preferences. Options may include:
- Menopause hormone therapy or hormone replacement therapy
- Vaginal hormonal therapy
- Non-hormonal medications
- Low-dose antidepressants
- Lifestyle support
We carefully monitor your health before, during, and after menopause, adjusting treatment as your needs change.
Take the next step
Menopause is a natural transition, but you don’t have to navigate it alone. At Sheridan Memorial Hospital Women’s Clinic, we provide expert care and support to help you feel your best through every stage of this journey.
Call today to schedule an appointment and discuss your menopause treatment options.

Uterine fibroids are one of the most common gynecological conditions. While these growths are usually non-cancerous, they can cause a wide range of disruptive symptoms for many women.
At Sheridan Memorial Hospital Women’s Clinic, our women’s health specialists provide expert diagnosis and treatment for fibroids—helping you find relief and improve your quality of life.
What are fibroids?
Fibroids are benign (non-cancerous) tumors that grow in the uterus. They can vary widely in size, number and location.
Risk factors for fibroids include:
- Family history of fibroids
- Age (more common after 40)
- Obesity
- High blood pressure
- Never having been pregnant
- Being a woman of color (higher likelihood of developing multiple or more severe fibroids)
Symptoms of fibroids
Many women with fibroids experience no symptoms and may only learn about them during a routine well-woman exam.
When symptoms do occur, they may include:
- Heavy or prolonged menstrual bleeding
- Pelvic pain or cramping
- Pelvic pressure or fullness
- Urinary frequency or incontinence
Symptoms often worsen during menstrual cycles due to hormonal fluctuations. If fibroids interfere with your daily activities, it’s important to seek evaluation.
Diagnosing fibroids
Your provider may suspect fibroids after a pelvic exam. To confirm the diagnosis and better understand their size and location, additional imaging tests may include:
- Ultrasound
- MRI
These tests help guide the most effective treatment plan for your needs.
Treatment options for fibroids
Treatment depends on the severity of your symptoms, your health, and your family planning goals. Options may include:
Medications
- Hormonal birth control – helps regulate cycles and control bleeding
- GnRH agonists – shrink fibroids and ease symptoms
Minimally invasive & surgical treatments
- MyoSure® – a minimally invasive procedure that removes fibroids while preserving the uterus
- Myomectomy – surgical removal of fibroids while keeping the uterus intact
- Hysterectomy – removal of the uterus, typically recommended for women with severe fibroid complications who do not wish to have future pregnancies
Take the next step
Fibroids are common—but you don’t have to live with the discomfort they cause. The women’s health team at Sheridan Memorial Hospital Women’s Clinic offers personalized treatment options to help you take control of your health and restore comfort.
Call today to schedule your fibroid consultation.

Urinary incontinence — the involuntary loss of bladder control—affects up to 45% of women at some point in their lives. For some, it’s a mild inconvenience; for others, it can be deeply disruptive and limit daily activities.
At Sheridan Memorial Hospital Women’s Clinic, our team offers compassionate, effective treatments to help you regain confidence and improve your quality of life.
What is urinary incontinence?
Urinary incontinence occurs when your bladder muscles or nerves don’t work together properly, leading to urine leakage. The condition can range from occasional drips during activity to sudden, strong urges that make it difficult to reach the bathroom in time.
Types of urinary incontinence in women
Understanding your type of incontinence helps guide treatment:
- Stress incontinence – Leakage occurs with physical activity that puts pressure on the bladder, such as coughing, laughing, sneezing, exercising, or lifting heavy objects.
- Urgency incontinence (overactive bladder) – A sudden, overwhelming urge to urinate followed by involuntary leakage.
- Mixed incontinence – A combination of stress and urgency incontinence.
- Overflow incontinence – The bladder doesn’t empty completely, causing leakage or dribbling.
- Transient incontinence – Short-term incontinence caused by medications, infections, or temporary health conditions.
When to see a doctor
Even small amounts of leakage are worth discussing with your provider. Urinary incontinence is not an inevitable part of aging — and treatments are available. Schedule an appointment if you:
- Leak urine during exercise, laughing, or sneezing
- Frequently feel a strong urge to urinate
- Avoid activities or social events due to fear of accidents
- Wake up multiple times at night to urinate
Treatment options for urinary incontinence
Your provider will create a personalized treatment plan based on the type of incontinence, its severity, and your overall health. Options may include:
Lifestyle and behavioral therapies
- Bladder training and timed bathroom breaks
- Limiting caffeine, alcohol, or evening fluid intake
- Pelvic floor strengthening exercises (Kegels)
Medical treatments
- Prescription medications to calm overactive bladder
- Vaginal devices (pessaries) for support
Surgical options
If conservative care doesn’t provide enough relief, procedures may be recommended:
- Sling procedure: A strip of tissue or synthetic mesh supports the urethra to prevent leaks.
- Bulking agents: Injections near the urinary sphincter help thicken tissue and reduce leakage.
Take back control
You don’t have to live with bladder leakage. Our women’s health specialists at Sheridan Memorial Hospital Women’s Clinic provide discreet, effective care for urinary incontinence.
Call today to schedule your appointment and take the first step toward lasting relief.

About 1 in 10 women of childbearing age experience infertility. Struggling to conceive can feel overwhelming, but infertility does not mean you cannot become pregnant. With the right diagnosis and treatment, many women are able to achieve their dream of starting or growing their family.
At Sheridan Memorial Hospital Women’s Clinic, our compassionate team specializes in identifying the causes of infertility and providing effective treatment options tailored to your needs.
What is infertility?
Infertility is defined as:
- Inability to get pregnant after one year of trying (if under 35)
- Inability to get pregnant after six months of trying (if 35 or older)
Infertility can affect either partner. While many women assume infertility is solely a female issue, male factors account for nearly half of all cases. That’s why a thorough evaluation is important for both partners.
Causes of infertility in women
Infertility may result from a variety of conditions, including:
- Ovulation disorders – The most common cause of infertility. Conditions such as polycystic ovary syndrome (PCOS), hypothalamic dysfunction, or premature ovarian insufficiency (POI) can disrupt ovulation.
- Fallopian tube damage or blockage – Caused by pelvic inflammatory disease (PID), scar tissue from endometriosis, or prior pelvic surgery. This prevents the egg from traveling to the uterus.
- Uterine dysfunction – Fibroids or endometriosis may alter the structure of the uterus, interfering with implantation or pregnancy.
- Age-related infertility/menopause – Natural decline in ovarian function, which can happen at any age, ends fertility permanently.
What to expect during an infertility evaluation
Your fertility evaluation at Sheridan Memorial Hospital Women’s Clinic includes a thorough history, physical exam, and diagnostic testing to determine the cause. Depending on your symptoms and needs, tests may include:
- Ovulation assessment – Blood tests, ultrasound, or at-home ovulation kits
- Hysterosalpingogram (HSG): An X-ray test that evaluates whether your fallopian tubes are open
- Laparoscopy: A minimally invasive procedure to look for pelvic scarring, endometriosis, or blockages
- Ultrasound
This comprehensive approach helps your provider identify whether infertility is related to ovulation, fallopian tubes, uterine structure, or other factors.
Infertility treatment options
Once the cause is identified, our team develops a personalized treatment plan that may include:
- Medication – To stimulate ovulation and regulate cycles
- Surgery – To repair blocked fallopian tubes, remove fibroids, or treat endometriosis
- Reproductive assistance – Options such as intrauterine insemination (IUI) or referral for advanced fertility treatments (like IVF) when appropriate
Compassionate support on your fertility journey
We understand that infertility can be emotionally challenging. Our team is here to provide medical expertise, emotional support and personalized care every step of the way.
If you’re struggling to conceive, call Sheridan Memorial Hospital Women’s Clinic today to schedule your fertility evaluation.

Sexually transmitted diseases (STDs), also called sexually transmitted infections (STIs), are very common. The Centers for Disease Control and Prevention (CDC) estimates there are over 20 million new cases every year in the U.S.
At Sheridan Memorial Hospital Women’s Clinic, our team provides confidential, accurate STD testing and treatment. We help you protect your health, reduce the risk of spreading infections, and get relief from uncomfortable symptoms.
Why STD testing matters
Many STDs cause few or no symptoms at first, which means you may not know you have one. Untreated infections can lead to:
- Fertility problems
- Pelvic inflammatory disease (PID)
- Chronic pelvic pain
- Increased risk of HIV transmission
Regular STD screening is one of the best steps you can take to protect your long-term health.
Common STDs we test for
We offer comprehensive testing for a wide range of infections, including:
- Chlamydia
- Gonorrhea
- Herpes (genital or oral)
- Human papillomavirus (HPV) / Genital warts
- Syphilis
- Trichomoniasis
- Hepatitis B
- HIV (recommended at least every 6–12 months if you are sexually active or at higher risk)
STD testing may also be included as part of your annual well-woman exam, but more frequent testing is recommended if you have new or multiple partners, or believe you’ve been exposed.
How STD testing works
Testing methods depend on the infection being checked. Common tests include:
- Blood test (finger prick or blood draw)
- Urine sample
- Swab of the mouth, cervix, urethra, anus, or any discharge/sores
Your provider will explain which tests are appropriate based on your symptoms, medical history, and risk factors.
STD treatment options
Treatment depends on the type of infection:
- Bacterial STDs (like chlamydia, gonorrhea, or syphilis) – usually treated with antibiotics
- Viral STDs (like herpes or hepatitis B) – managed with antiviral medications and symptom control
- HIV – while there is no cure, modern treatments can help you live a long, healthy life
If you test positive, your provider will create a personalized care plan and discuss next steps. We will also guide you in talking with sexual partners so they can be tested and treated if necessary.
Protecting your health
The best way to protect yourself is through regular testing, safer sex practices, and open communication with partners. If you experience symptoms—or think you may have been exposed — don’t wait.
Call Sheridan Memorial Hospital Women’s Clinic today to schedule confidential STD testing and take charge of your sexual health.

Pelvic pain that happens regularly can disrupt your daily life and may signal an underlying gynecological condition. Whether the pain is constant, comes and goes, or appears only during certain activities — such as sexual intercourse, exercise or using the bathroom — it deserves evaluation.
Our women’s health team provides thorough evaluation, diagnosis, and treatment to help you find relief and protect your long-term health.
What is pelvic pain?
Pelvic pain is discomfort felt in the lower abdomen — below the belly button — where muscles, connective tissue and nerves support key organs, including:
- Female reproductive organs (uterus, ovaries, fallopian tubes)
- Urinary organs (bladder, urethra)
- Parts of the digestive tract (large intestine, rectum)
Depending on the cause, pelvic pain may feel:
- Dull or achy
- Sharp or stabbing
- Constant or intermittent
- Radiating to the back, buttocks, or thighs
It can also be accompanied by other symptoms such as:
- Heavy or irregular vaginal bleeding
- Bloating, constipation, or diarrhea
- Pain during sex
- Fever or signs of infection
Causes of pelvic pain
Pelvic pain may occur with ovulation or menstruation, but it can also indicate an underlying condition affecting the reproductive or urinary system. Common gynecologic causes include:
- Endometriosis
- Pelvic inflammatory disease (PID)
- Ovarian cysts
- Uterine fibroids
- Sexually transmitted infections (STIs)
- Ectopic pregnancy or miscarriage
Other non-gynecological causes may include kidney stones, irritable bowel syndrome (IBS), or appendicitis.
If pelvic pain starts suddenly and is severe, seek medical care immediately.
Treatment options for pelvic pain
Treatment depends on the cause of your symptoms. Options may include:
- Medications – such as antibiotics for infections, hormonal therapies (e.g., birth control pills), or pain management
- Minimally invasive surgery – to treat ovarian cysts, fibroids, or endometriosis
- Pelvic floor therapy – exercises and rehabilitation to strengthen muscles and relieve discomfort
- Lifestyle support – stress management, dietary adjustments, and exercise recommendations
Take the next step
You don’t need to live with ongoing pelvic pain. Our women’s health specialists can help find the cause and recommend effective treatment options tailored to your needs.
If you’re experiencing pelvic pain that interferes with your life, schedule an appointment today.

Bleeding after menopause
Menopause is officially confirmed 12 months after your last menstrual period. Any vaginal bleeding or spotting that happens after this point is called postmenopausal bleeding (PMB) — and it’s not considered normal.
While the cause is often minor and treatable, postmenopausal bleeding can sometimes be an early sign of a more serious condition. That’s why it’s important to have it checked by a healthcare provider right away.
What causes bleeding after menopause?
In most cases, postmenopausal bleeding is linked to non-cancerous or easily treatable conditions. Common causes include:
- Vaginal atrophy (atrophic vaginitis): thinning and inflammation of the vaginal lining after menopause
- Endometrial atrophy: thinning of the uterine lining
- Polyps: small, usually benign growths in the uterus or cervix
- Endometrial hyperplasia: thickening of the uterine lining
- Cervical or uterine changes: abnormalities that may require further evaluation
Most of these conditions are not serious. However, in about 10% of cases, postmenopausal bleeding can be linked to uterine or cervical cancer. Early detection greatly improves treatment outcomes, so evaluation is essential.
How doctors diagnose postmenopausal bleeding
If you experience bleeding after menopause, your doctor may refer you to a gynecologist for further evaluation. Depending on your history and symptoms, your provider may recommend:
- Pelvic exam and cervical screening (Pap test): to check for abnormalities in the cervix or uterus
- Blood tests: to check hormone levels, anemia, or other conditions
- Pelvic ultrasound (transabdominal or transvaginal): to view the uterus, cervix, endometrium, and ovaries
- Endometrial biopsy (pipelle test): a thin tube is inserted into the uterus to collect a small sample of tissue
- Hysteroscopy: a thin, lighted scope is used to look inside the uterus; biopsies may be taken during this procedure
- Dilation and curettage (D&C): scraping of the uterine lining under anesthesia to collect tissue samples
These tests help determine the exact cause of bleeding and guide treatment.
Treatment for postmenopausal bleeding
Treatment depends on the underlying cause:
- Vaginal or endometrial atrophy: often treated with estrogen therapy (pills, creams, patches, vaginal rings, or gels)
- Polyps: surgically removed, sometimes in a same-day procedure
- Endometrial hyperplasia: treated with progesterone medications and/or surgical procedures
- Cancerous or precancerous changes: may require surgery or other specialized treatments, which are most effective when detected early
Your gynecologist will explain each option, ensuring you understand why a particular treatment or test is recommended.
Don’t ignore bleeding after menopause
Even though most cases of postmenopausal bleeding are not serious, it’s always important to get evaluated. Prompt care can rule out cancer, give you peace of mind, and ensure that if there is a serious condition, it is treated early and effectively.
If you notice bleeding after menopause, schedule an appointment with your doctor right away.

If you are experiencing heavy periods, bleeding between periods, or menstrual cycles that feel irregular, you may have a condition called abnormal uterine bleeding (AUB). This is a common concern—and one our women’s health specialists are here to help you manage.
What is abnormal uterine bleeding?
Abnormal uterine bleeding refers to changes in the frequency, duration, regularity or flow of your menstrual cycle outside of pregnancy.
A normal menstrual cycle typically lasts 24–38 days, with bleeding lasting up to seven days. If your period is significantly heavier, lasts longer or comes too often — or too infrequently — you may be experiencing AUB.
How common is irregular menstrual bleeding?
About 1 in 3 people with periods experience irregular bleeding at some point, most often at the start of menstruation (menarche) or near menopause.
Causes of abnormal uterine bleeding
AUB can be linked to hormone imbalances, uterine growths, or other medical conditions. Doctors often use the PALM-COEIN system to describe causes:
- P: Polyps – Noncancerous growths in the uterine lining, often causing bleeding between periods.
- A: Adenomyosis – Endometrial tissue growing into the uterine muscle, causing pain and heavy bleeding.
- L: Leiomyomas (Fibroids) – Benign uterine tumors that can cause heavy or prolonged periods.
- M: Malignancy/Hyperplasia – Abnormal or cancerous growths in the uterus.
- C: Coagulopathy – Blood-clotting disorders, affecting about 20% of women with heavy bleeding.
- O: Ovulatory Dysfunction – Irregular or absent ovulation, often linked with polycystic ovary syndrome (PCOS).
- E: Endometrial Causes – Inflammation, infection, or overgrowth of the uterine lining.
- I: Iatrogenic – Medication side effects, including birth control or hormone therapy.
- N: Not Classified – Rare causes such as post-surgical complications.
Symptoms of abnormal uterine bleeding
You may have AUB if:
- Your period lasts longer than 7 days
- Your cycles come closer than 21 days or farther apart than 35 days
- You bleed heavily enough to pass large clots or soak through a pad or tampon every hour for more than 2 hours
- You experience bleeding between periods or after sex
If you notice these symptoms, it’s important to schedule an appointment with your healthcare provider.
Diagnosis: How doctors evaluate AUB
Your provider will begin with a pregnancy test to rule out complications such as miscarriage or ectopic pregnancy. Additional steps may include:
- Medical history & menstrual tracking
- Physical exam – including thyroid and hormone checks
- Pelvic exam & Pap smear – to check for infections, cervical changes, or polyps
- Blood tests – to evaluate hormone levels and check for anemia
- Ultrasound – to detect fibroids, polyps, or abnormal uterine lining
- Hysteroscopy – to look directly inside the uterus and remove growths if needed
- Endometrial biopsy – especially for women over 45 or with PCOS, to rule out endometrial cancer
Treatment options for abnormal uterine bleeding
Treatment depends on your age, overall health, and whether you want future pregnancies. Options may include:
Medications
- Hormonal birth control (pills, patch, IUD) – regulate cycles, reduce bleeding, prevent pregnancy
- NSAIDs (e.g., ibuprofen) – reduce bleeding and relieve cramps
- Tranexamic acid – helps slow blood loss during heavy periods
Procedures & Surgery
- Endometrial ablation – removes the uterine lining (not for women planning future pregnancies)
- Myomectomy – removes fibroids while preserving fertility
- Hysterectomy – removes the uterus; often a last resort when other treatments fail
Lifestyle Support
- Weight management, diet changes, and exercise can improve symptoms—especially for women with PCOS.
Why it matters: Complications of untreated AUB
Chronic or severe abnormal bleeding can lead to:
- Anemia (low red blood cells)
- Infertility
- Endometrial cancer (in some cases)
In rare cases, acute heavy bleeding may cause severe anemia, shock, or other life-threatening complications. If you experience very heavy bleeding, seek immediate medical care.
Take the next step
If you have irregular or heavy menstrual bleeding, don’t wait — abnormal uterine bleeding is treatable. Our women’s health specialists can provide the right diagnosis and treatment to help you feel better and protect your long-term health.

Pelvic organ prolapse (POP) is more common than many people realize — but it often goes undiscussed. Many women feel uncertain or even embarrassed about the condition, yet POP affects millions of women across all ages. If you’re experiencing symptoms, know that you are not alone and that help is available. Call Sheridan Memorial Hospital Women’s Clinic to schedule your appointment today.
What Is POP?
POP occurs when one or more pelvic organs — such as the bladder, uterus, rectum or vagina — shift downward due to a weakened pelvic floor. The pelvic floor is a network of muscles, ligaments and connective tissue that normally supports these organs. When it weakens, organs may press into or even bulge outside the vagina, causing a variety of symptoms.
Symptoms
Symptoms can vary but often include:
-
Leaking urine or difficulty emptying the bladder
-
Bowel problems, including constipation or needing to press inside the vagina to pass stool
-
Vaginal bulging or pressure, sometimes described as the feeling of a tampon “half in and half out”
-
Pain or pressure in the lower back or pelvis
-
Discomfort or pain with sex
-
Vaginal noises during exercise or intimacy
Symptoms usually develop gradually, though they can occasionally appear suddenly (for example, during strenuous exercise).
Who Is at Risk?
POP can affect women at any stage of life. Risk factors include:
-
Pregnancy and childbirth
-
Aging and menopause
-
Family history of POP or connective-tissue disorders
-
Obesity
-
Previous pelvic surgery, such as hysterectomy
-
Chronic constipation or straining
-
Long-term coughing from smoking or lung disease
-
Heavy lifting or high-impact activities
By age 80, nearly half of all women experience some degree of POP.
Treatment Options
The good news: effective treatments are available, and not every woman needs medical intervention. Together with your OB/GYN, you can decide what’s best for you. Options may include:
Lifestyle and self-care
-
Increase dietary fiber and hydration to ease bowel movements
-
Maintain a healthy weight
-
Strengthen your core with low-impact activities like yoga or Pilates
Medical therapies
-
Pessaries: Simple devices placed in the vagina to support pelvic organs, relieving bulging or leaking.
-
Pelvic floor therapy: Guided exercises (such as Kegels) taught by a physical therapist to strengthen the pelvic floor correctly and safely.
Surgical treatment
If POP significantly affects your quality of life, surgery may be considered to restore support and relieve symptoms.
Postpartum Care and Prevention
The postpartum period, often called the “fourth trimester,” is an ideal time to check in on your pelvic floor health. Preventive steps — such as pelvic floor therapy, diet changes, or the use of a pessary—can help reduce future risk of POP.
When it comes to running, efficient movement and injury prevention matter just as much as wearing a good pair of sneakers. Common running mistakes—like excessive pelvic drop and overstriding—when they occur too frequently, place extra stress on the muscles and joints of the lower back, hips and knees. Over time, this added strain increases a runner’s risk for injury.
 Wyoming Rehab’s C-Mill—an advanced piece of equipment resembling a treadmill available at only a few locations nationwide—integrates virtual reality to add variety to exercises, features a force plate to measure gait and adaptability and includes frontal and side cameras for in-depth analysis of walking or running patterns.
Wyoming Rehab’s C-Mill—an advanced piece of equipment resembling a treadmill available at only a few locations nationwide—integrates virtual reality to add variety to exercises, features a force plate to measure gait and adaptability and includes frontal and side cameras for in-depth analysis of walking or running patterns.
The C-Mill is a powerful tool for improving movement efficiency and reducing injury risk. While commonly used in stroke and traumatic brain injury rehabilitation, it also plays a vital role in performance training for athletes at all levels.
“It’s super cool equipment,” said Wyoming Rehab’s Lindsay Kinney, PT, DPT, COMT. “You record a 30-second video, and the C-Mill picks up on all of the weight-bearing, loading and any asymmetry that you can see with somebody’s strike or step length. It’s truly a one-of-a-kind device, and I feel lucky to have access to it.”
One person benefiting from the C-Mill’s technology is Daniel Katz, an avid runner and EMT with Wyoming Regional EMS. Daniel recently underwent a gait analysis with Wyoming Rehab using the C-Mill, and his experience highlights how understanding your body’s movement and making small adjustments can lead to significant long-term benefits.
Daniel, who has completed marathons, half-marathons and ultra-races, discovered his love for long-distance running during the COVID-19 pandemic. What started as a short-term challenge when his friend invited him to run a virtual marathon quickly became a lifelong passion.
“Until I was 25, I swore I would never be a distance runner,” Daniel said. “But halfway through the virtual race, I ended up loving it and haven’t stopped running since.”
Daniel now trains for the 2025 Bighorn Trail Run, scheduled for June 20–21, 2025. The course, which traverses the Little Bighorn and Tongue River areas of Bighorn National Forest, challenges even the most seasoned ultra-runners, with over 20,500 feet of ascent and 20,750 feet of descent. Daniel completed the 52-mile course last year, and this year, he and his wife plan to tackle the 32-mile course together.
Over time, Daniel’s training has evolved, focusing on building weekly mileage to match or surpass race distances, stacking long runs and following a nutrition plan that supports his endurance. He now incorporates the C-Mill into his training to elevate his performance.
A typical running gait analysis at Wyoming Rehab begins with a discussion about the runner’s injury history and current issues. Lindsay then conducts a full mobility and strength assessment in a treatment room, followed by a run on the C-Mill. Using insights from both the assessment and the C-Mill, she creates a personalized treatment plan that may include targeted strength training and gait re-training to improve running mechanics.
 Daniel’s gait analysis revealed key insights into his running form. Video footage showed a pelvic drop of more than six degrees, suggesting reduced lateral hip strength. This kind of asymmetry commonly contributes to running injuries. To address this, Lindsay recommended exercises to strengthen the gluteus medius and hip rotators, as well as targeted training to help Daniel maintain a level pelvis while running.
Daniel’s gait analysis revealed key insights into his running form. Video footage showed a pelvic drop of more than six degrees, suggesting reduced lateral hip strength. This kind of asymmetry commonly contributes to running injuries. To address this, Lindsay recommended exercises to strengthen the gluteus medius and hip rotators, as well as targeted training to help Daniel maintain a level pelvis while running.
Additionally, the distance between Daniel’s foot and center of mass indicated overstriding. To improve efficiency and reduce injury risk, Lindsay suggested cadence adjustments to bring his foot strike closer to his body.
“Catching these discrepancies now is powerful, as we can address them before they become problems in the future, especially when Daniel is packing in the miles during a training cycle for a race,” Lindsay said. “If he doesn’t fix these issues, somewhere else in the body must pick up the slack, overloading an area that might not be equipped to handle it.”
Daniel appreciated both the depth of insight and Lindsay’s passion for helping runners.
“What’s great about Lindsay is that you can find a lot of people who know their stuff, but she loves this stuff,” he said. “And she’s a runner, too.”
“Runners are unique—all we want to do is run,” Lindsay added. “Sustaining an injury that prevents us from being able to do that is demoralizing, especially if it we have to miss a race because of it. A personalized analysis is a helpful way in keeping us out running on the roads or trails and reducing one’s chances for overload injuries.”
Using the information gathered from Daniel’s running gait analysis, he and Lindsay now have a clear roadmap to improve his running mechanics and stay healthy for the long haul.
“I’m not setting out to be a top-of-the-world runner,” Daniel said. “But I do want to keep running for the next three to four decades. If I can be one of those old guys who still run marathons at 72 that would be awesome. This analysis will help me stay on track.”
Lindsay emphasized that the goal of gait analysis isn’t necessarily to change a runner’s stride, but to optimize their natural movement patterns.
“Everyone has their ‘signature’ moves,” she explained. “Everyone is so individualized. Using the C-Mill, we can identify factors that may predispose someone to injury and provide exercises to strengthen those areas, making their running gait as efficient as possible.”
For Daniel, the experience reinforced the importance of periodic assessments, even for healthy athletes.
“Any work you do when you’re healthy helps prevent injuries and accelerates your training,” Daniel said. “It’s like mental health—when you connect with a therapist while you’re healthy and not in crisis mode, the good work can actually be done.”
He also noted how the C-Mill helped him better understand his body’s needs.
“This will help people develop intuition about their bodies,” Daniel said. “People should listen to their bodies, and they can come in to do these assessments to learn how.”
Looking to enhance your performance and stay injury-free? Call Wyoming Rehab today at 307.674.1632 to schedule your free screening and receive personalized treatment recommendations for non-emergent impairments and injuries. Visit wyomingrehab.org to explore Wyoming Rehab’s full range of services.

Longtime SMH volunteer on finding resilience and community through service
For Judy Hayworth, Sheridan Memorial Hospital represents more than just a place for treatment—it provides strength, healing and community. Recovering from her fifth bout with cancer, Judy continues to approach life with resilience and gratitude, not only for the care she has received but also for the opportunity to give back to the very institution and community that supported her throughout her journey.
Judy was first diagnosed with stage 4 colon cancer in 2008, followed by stage 1 colon cancer in 2018, and then faced recurring tongue cancer three times in 2023 and 2024. Throughout those years, she received various treatments at Sheridan Memorial Hospital, and she speaks highly of the compassionate, wraparound care she received.
From surgery performed by Dr. Barry Mangus at Big Horn Surgical to remove part of her colon to Ear, Nose & Throat specialist Dr. Cheryl Varner discovering her tongue cancer, chemotherapy and radiation at the Welch Cancer Center to speech therapy with Wyoming Rehab, Judy is well-versed in Sheridan Memorial Hospital and its services.
“I think it’s wonderful that people come from Gillette, Buffalo and other communities to receive care here,” Judy said. “Sheridan Memorial Hospital has a wonderful reputation, and people know they’ll receive good care. We are very fortunate to have the quality of care that we do here. I had a mammogram last Sunday at SameDay Health & Imaging, and when I left, I told somebody, ‘I would go there any time!’ Everyone there is so nice and efficient.”
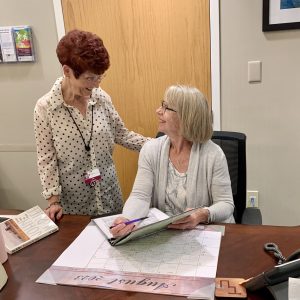 Despite her health challenges, Judy found a meaningful way to channel her gratitude—through volunteer work at Sheridan Memorial Hospital and in the broader Sheridan community.
Despite her health challenges, Judy found a meaningful way to channel her gratitude—through volunteer work at Sheridan Memorial Hospital and in the broader Sheridan community.
Judy joined Sheridan Memorial Hospital as a volunteer shortly after overcoming colon cancer in 2009, providing companionship and comfort to those waiting in the surgical waiting room for their loved ones undergoing surgery.
“Many times, especially with younger people who haven’t experienced having a loved one in the hospital before, they can be very upset,” Judy explained. “I always try to comfort them because it can feel overwhelming. I like that I can help them, even just a little bit, during those times.”
 In addition to her work in the surgical waiting room, Judy also serves as a member of the Sheridan Memorial Hospital Auxiliary, a group of individuals who come together to support the hospital’s mission, staff and patients. The Auxiliary’s efforts include fundraising and volunteering their time through initiatives such as Trees of Love and the annual 5-Year-Old Birthday Party. They also help spread holiday cheer by decorating Christmas trees throughout the hospital and its clinics each holiday season and assist with mailings for the hospital, among other important initiatives.
In addition to her work in the surgical waiting room, Judy also serves as a member of the Sheridan Memorial Hospital Auxiliary, a group of individuals who come together to support the hospital’s mission, staff and patients. The Auxiliary’s efforts include fundraising and volunteering their time through initiatives such as Trees of Love and the annual 5-Year-Old Birthday Party. They also help spread holiday cheer by decorating Christmas trees throughout the hospital and its clinics each holiday season and assist with mailings for the hospital, among other important initiatives.
“The Auxiliary is a wonderful organization,” Judy praised. “They tune into what’s important and where there’s a need, and I love that.”
Judy and her daughter, Heidi, also enjoy participating in the Sheridan Memorial Hospital Foundation’s Link – Partners in Pink annual run/walk each year.
Outside of Sheridan Memorial Hospital, Judy stays just as busy, volunteering as a Court Appointed Special Advocate, a meal room attendant at The Hub on Smith and an usher and ticket taker at the WYO Performing Arts & Education Center. In recognition of her dedication, Judy received the 2023 AARP Wyoming Andrus Award, which honors the state’s top volunteer over age 50, and was named the 2024 Sheridan College Distinguished Alum.
 Judy looks forward to volunteering again after taking a break from December 2023 to March 2024 to recover from tongue cancer. When asked what she would say to someone considering volunteering at Sheridan Memorial Hospital, Judy encouraged them to do it.
Judy looks forward to volunteering again after taking a break from December 2023 to March 2024 to recover from tongue cancer. When asked what she would say to someone considering volunteering at Sheridan Memorial Hospital, Judy encouraged them to do it.
“It doesn’t have to be in the surgical waiting room,” she said. “It could be in the gift shop or taking newspapers around. You feel that your time is rewarded for being here. I just love it, the way everyone treats each other. I would say you’ll find it very enjoyable.”
April is National Volunteer Month. If you would like to learn more about Sheridan Memorial Hospital’s volunteer program or share an experience you have had as or with one of our volunteers, please contact Jasmine Slater at jasmineslater@sheridanhospital.org or 307.675.2620.

A Sheridan couple’s journey through Sheridan Memorial Hospital’s continuum of care
At Sheridan Memorial Hospital, orthopedic care, rehabilitation and interdepartmental collaboration come together to deliver exceptional patient outcomes. Dan and Rosemary Rieder are living examples of the hospital’s commitment to ensuring patient care across the organization is a seamless experience.
Dan struggled with joint pain and arthritis, which significantly impacted his daily life, making even routine tasks like grocery shopping difficult and preventing him from getting restful sleep.
“I could barely get in the car after grocery shopping, my knee was so stiff,” Dan shared. “And my shoulder was grinding, losing flexibility and causing pain. In both cases, they got so uncomfortable that the only real solution was to replace both joints.”
Dan’s wife, Rosemary, encouraged him to seek treatment at Sheridan Orthopaedic Associates after her own positive experience with Dr. Brian Laman, who performed a minor arthroscopic procedure for her. Her trust in the team’s expertise gave Dan confidence in their care, leading him to undergo a reverse total shoulder replacement with Dr. Justin Steinert in November 2023, followed by a knee replacement with Dr. Brian Laman in November 2024.
When Dan’s medical history—specifically his use of blood thinners for an artificial heart valve—led to complications during and after his shoulder surgery, the staff at Sheridan Memorial Hospital collaborated to provide comprehensive care. This included managing excessive bleeding and the need for a blood transfusion following an emergency room visit due to dangerously low hemoglobin levels. These coordinated efforts ensured Dan’s safety and supported Rosemary as his caregiver, while preventing similar complications in future procedures.
Dan and Rosemary were deeply appreciative of the care he received.
“When I was admitted to the hospital following my shoulder surgery, Dr. Steinert was there right away to check on my situation. He didn’t have a responsibility for my care, but he still came in to see how I was doing. I was also impressed because the CNAs and other nurses. The CNAs were kind and caring and the nurses would come in and do things that nurse don’t have to do. They would clean up my dishes, take out the trash and straighten my sheets. They just generally cared about my comfort,” Dan said.
Following Dan’s hospital stay after his shoulder surgery and in preparation for his upcoming knee surgery with Dr. Laman, his care team collaborated to develop a proactive plan to prevent similar complications. Dr. Laman worked closely with Jason Otto, PA-C and Registered Nurse Barb Shumaker from Sheridan Memorial Hospital’s Internal Medicine clinic to implement a strategy known as “bridging.” This approach involved transitioning Dan from blood thinners to anticoagulants through a series of twice-daily injections for 10 days before surgery. By carefully managing his medication in this way, the team aimed to reduce the risk of complications and ensure a smoother recovery after Dan’s knee replacement.
As Dan’s caretaker following his previous surgery and in anticipation for the upcoming one, Rosemary said she was thankful for being included in the process.
“They always gave me the information I needed,” Rosemary said. “Many times, when you’re the one receiving care, doctors will only talk to you. I found that, in Dan’s case, when a doctor came in, they not only talked to him, but also to me, and I found that comforting.”
This proactive strategy proved successful, and Dan’s knee replacement surgery was completed without additional complications. He is now pleased with the results of both surgeries and demonstrates the progress he has made, easily stretching and bending his arm over his head.
“With my shoulder, I had difficulty maneuvering in certain ways, but now, being able to do this…” Dan said, demonstrating his ability to stretch and bend his arm over his head. “Being able to reach behind my back to put on my belt is great. The cooperation between departments, the surgeons and everyone involved worked really well.”
Post-surgical rehabilitation was essential to Dan’s recovery, and Sheridan Memorial Hospital’s Wyoming Rehab provided the physical therapy necessary to restore strength and function to his knee. Physical therapist Lindsay Kinney worked with Dan to achieve his goal of straightening his knee to 0 degrees and flexing it to at least 120 degrees.
“They take you from where you begin, knowing where you want to end up, and walk you through the stages of gaining more flexibility and strength,” Dan explained.
In the end, Dan was able to flex his knee to between 124 and 126 degrees.
Dan is not the only one who has benefited from Wyoming Rehab’s care. Rosemary had previously received treatment for vertigo at Wyoming Rehab, and she is currently undergoing physical therapy for nerve pain in her neck and arms. She echoed her husband’s appreciation for the team, particularly physical therapist Lindsay Kinney.
“I’m no sooner home from my appointment, and there’s a notice that my notes have been updated in the patient portal,” Rosemary shared. “And I think Lindsay is amazing. She has so much knowledge about nerves, and she explains everything so I understand why she’s doing what she’s doing. When she’s pulling on my head, I know there’s a reason for it. I may walk in with pain, but after Lindsay does some of the exercises with me, she’ll ask, ‘How’s your pain?’ and I’ll say, ‘I don’t have any.’”
For Rosemary and Dan, the key takeaways from their experiences with both the surgeries and rehabilitation were the importance of staying on top of health concerns and consistently working on improvement.
“I think the challenge for anyone who has an issue is accepting that issue for what it is and getting the help you need,” Rosemary said. “Don’t wait, because then the problem becomes larger. We have great people at the hospital, so I think not letting something get the best of you is probably more important than anything. Get the help you need. I feel like I’m getting the help I need because some of my pain is already starting to ease up.”
“My knee still gets grouchy at times, especially because of the weather, but I know that I am also continuing to work on it,” Dan shared. “It’s a long, slow process, and when I went into Wyoming Rehab in the beginning, they made it pretty clear that it was going to be challenging, but that’s necessary in order to get to the end. They let me know that right away. I felt the challenge was pushing beyond the pain a little bit, but the reward came when they’d measure my progress, so you were constantly encouraged that you were getting somewhere. So, yeah, it’s hard, but you’ll be glad you didn’t let it go.”
“Except your other shoulder and other knee,” Rosemary joked, amidst her husband’s mock shushing. “But we don’t talk about that. I told him to just give me a couple more months before he decides to do all this again.”
For more information about Sheridan Orthopaedics and Wyoming Rehab, please visit sheridanortho.com and wyomingrehab.org.

High school student touts SameDay Health & Imaging care
When Brett Oetken slipped and fell on the ice at school, he knew he had injured himself beyond a couple bumps or bruises.
“I was at school and slipped on the ice on my way in,” Brett said recently. “At that point I was really worried about it because I wasn’t able to put any pressure on it or bend it at all.”
Following the fall, Brett went to the school nurse’s office and then called his mother and asked about getting his knee checked out that day. Brett’s mom, Erin Oetken, called ahead as they made their way across town to SameDay Health & Imaging, a Sheridan Memorial Hospital clinic located between Walmart and WyoVision. The clinic offers urgent care, imaging and laboratory services seven days a week.
Within a few minutes of arriving, the medical staff were examining Brett’s knee.
“I thought it was really fast and convenient, because within an hour of me falling on the ice and hurting my knee, I was getting seen by a doctor and about to get an X-ray,” Brett said. “This injury happened in the middle of my track season, so I was really concerned about it.”
Brett saw Dr. Christopher Prior, one of two physicians at SameDay Health & Imaging who work alongside a team of advanced practitioners, nurses, phlebotomists, imaging technicians and others who ensure each patient receives excellent, patient-centered care. During his visit, he received an X-ray to check for more serious injuries, an option available right there in the clinic.
Brett and his family had opted to see the team at SameDay Health & Imaging due to a prior experience at the clinic. Brett’s sister, Sheridan High School athlete Becca Oetken, had also utilized the clinic’s services for injuries and had been happy with the experience.
“Dr. Prior did a really good job explaining my treatment options,” Brett shared. “He told me that it would heal on its own and there’s no surgery required, which I was kind of worried about. Then he was looking at the X-rays with me so I could assess it with him. He made me feel very involved in the whole process.”
Dr. Prior had advised Brett that his knee would likely take nine or 10 days to heal, and right around that timeframe, Brett said he started feeling more confident in his injured leg. He eased back into his athletic activities and noted that within 15 days he felt back to lifting weights and running.
“I’m so grateful to the team at SameDay Health & Imaging because they were quick to see me and provided me with the care I needed to get back to sports,” Brett said.
SameDay Health & Imaging is open seven days a week, Monday through Friday from 6:30 a.m. to 6 p.m. and Saturdays and Sundays from 9 a.m. to 6 p.m. For additional information about the clinic, see sheridansameday.org.

Up until she was 98 years old, Annie Belish lived by herself. She always had help with cooking, cleaning and other household tasks, but she lived independently in her Sheridan home.
When one day a family member stopped by to check on Annie and discovered her on the floor, dehydrated and suffering from COVID, they quickly had her transported to Sheridan Memorial Hospital. Shortly after the illness, Annie experienced another setback – a fall resulting in a broken hip and subsequent surgery.
Following the surgery, Annie lived in a senior rehabilitation facility in Sheridan, but her family had heard good things about another long-term care option.
“Sheridan Green House had a much less institutional feel,” said Sue Belish, Annie’s daughter-in-law. “It felt homier. While she shared a room at the other facility, at the Green House she has a private room, and the cottage has a more pleasant atmosphere.”
At Sheridan Green House, there are cozy areas near the fireplace, in the kitchen or, during warmer months, outside on the patio surrounded by flowers. Annie’s private room also allows family to visit without feeling out of place or in the way of other residents.
In the spring of 2024, Sheridan Memorial Hospital took on operations at Sheridan Green House to ensure the asset remained available to community members and their families. Sheridan Green House got its start nearly 20 years ago, when a dedicated group of citizens, along with many philanthropic organizations, gathered with the purpose of providing a different model of care for loved ones as they age. That mission centered around providing long-term care in loving homes where every person could live a dignified, fulfilling life.
Annie has lived at Sheridan Green House for approximately three years now, and her family has shared that the experience remains positive under the hospital’s leadership. Communication is key to the family. They are encouraged by the efforts of the Green House staff who are keeping them in the loop about changes and processes.
Sue and her husband, Elbert, are reassured by the care Annie receives at Sheridan Green House. They noted Annie is clean and cared for, and the staff routinely tells the family about things Annie has said or done, providing reassurance that Annie is not just a patient, but part of a community.
On Christmas Eve, Sue and Annie’s daughter, Pennie Vance, joined Annie and her cottage companions in a cookie decorating and caroling event organized by the staff.
“It was a really nice activity for them,” Sue Belish said. “It made me feel good to walk into the cottage, see all the decorations and feel at home.”
The mission of Sheridan Green House is to provide long-term care in loving homes where every person lives a dignified fulfilling life. Recently, the Belishes have noticed improvements in Annie’s health, despite her advancing age. For example, when they stopped in to have lunch with Annie, they noticed she was feeding herself.
“She hasn’t done that for a long time,” Elbert said, noting that Sheridan Green House staff had been working with Annie on the task.
Sue added. “She’s thriving, as much as you could want a loved one to thrive.”
Sheridan Green House is comprised of four cottages, each with 12 rooms available for residents. If you or a loved one is considering long-term care, reach out to Sheridan Green House at 307.672.0600. For additional information, see sheridangreenhouse.org.
Addiction Medicine patient overcomes challenges to serve as peer specialist
Brent Weaver always wanted to experience things. After leaving a private parochial school and entering public school, he had a tendency to rebel and experiment with limits – both his own and testing the limits of authority figures around him.
“This set me up to make a lot of bad decisions,” Weaver said. “I made them, I made those choices, but those really started me down a specific path.”
Weaver said he began gravitating toward the people who accepted him, including a group of individuals who partied and used controlled substances. He stopped prioritizing extracurricular activities like sports and agricultural organizations and started using alcohol and marijuana around the age of 15. Through high school, he experimented with hallucinogens, various street drugs and pharmaceuticals. By his early 20s, Weaver had become dependent on prescription pain medications, both due to his addictive thinking and a serious back injury that resulted in prescriptions for pain medications. Weaver said it was at that time he crossed the line in how he abused substances.
“In my own mind, when I started doing that, I saw myself as a junkie,” Weaver said. “I had always looked at people who did that as powerless, helpless.”
Weaver added that his opinion of himself shattered shortly after that.
“I wasn’t functioning as a person anymore,” he said. “Looking back at how fast it all happened, it hurts. I lost a lot of people. People were going to prison, overdosing or just disappearing. Interpersonal connections were fading away. I wasn’t spending holidays with my family. It was a dark, dark place for me.”
Weaver said he would have thought rock bottom was the day he had to serve time for a possession charge and found a good friend dead of an overdose, but it was actually six months later. He had what he described as a lightbulb moment – when he realized his life was not going to change only with his best intentions or will power. He needed help.
“I knew if I didn’t take some drastic action and get out of my existing situation, nothing was going to change,” Weaver said. “I knew it as clear as anything in my life – that the path I was on was destructive and I was going to either be dead soon or on a bus to prison.”
Weaver had heard about a local rehabilitation program and relocated to Sheridan to seek treatment. He went through about three months of inpatient treatment followed by three months in transitional housing focused on recovery. From ages 25-28, Weaver made it about 11 months at a time without using controlled substances, but found himself relapsing. He later found a medication assisted treatment program, but when that healthcare provider closed his office, Weaver again found himself struggling.
About 10 years ago, though, Weaver began working with Dr. Jason Ackerman in the Sheridan Memorial Hospital Internal Medicine and Addiction Medicine Clinic. Weaver said the clinic is different from others with which he had worked. It treats patients with compassion and empathy while providing structure and accountability. It also offers support for patients who have a setback rather than being punitive, Weaver said. The MAT program through SMH has helped Weaver remain sober and he began working to help others suffering with addiction or at-risk for substance abuse.
He earned a job at a court-ordered youth school where he discovered the key to his sobriety – paying it forward and helping others.
“I have to be active in my recovery,” Weaver said. “I have to be actively helping people find what works for them and advocating for others to find recovery.”
When a peer specialist he had leaned on asked if he’d ever considered taking on a similar role, Weaver jumped at the chance and earned the credentialing needed to work in the facilities he had first come to as a patient. He has worked as a certified peer specialist since 2021 and prior to that, beginning in 2014, he worked with at-risk youth doing similar work, helping others with empathy and understanding.
“When you first come into recovery, you’re a shattered person, he said. “There is so much guilt and shame that you carry into the doors when you first want help. If you’re sitting across from someone who has been in a similar position, who isn’t judging you, who understands, you have more belief in yourself that you can make a change. You don’t feel alone.”
Weaver now spends two days per week in the SMH Internal and Addiction Medicine Clinic, working with others receiving treatment for addiction. The clinic on average sees 292 patients per month, and peer specialists work with nearly all of them. While healthcare providers may have difficulty building relationships with patients undergoing treatment for addiction, peer specialists have the ability to create an empathetic bond through personal experience and knowledge of addiction and recovery.
The team in the SMH Internal and Addiction Medicine Clinic have noted that patients who connect with peer specialists are more likely to stick with their treatment, have fewer or less intense relapses and follow through with their recovery process.
While Weaver has lived experiences that some would struggle to understand, his journey now provides hope and encouragement for those who continue to struggle with addiction.
To learn more about the Sheridan Memorial Hospital Internal and Addiction Medicine Clinic, see https://www.sheridanhospital.org/medical-services/clinics/addiction-medicine/

Charlie Gibson’s Journey at Sheridan Memorial Hospital Transitional Care: A Story of Resilience and Triumph
At 91, Charlie Gibson faced some of the toughest challenges of his life all at once. A prostate cancer diagnosis led to the discovery of a malignant kidney, which was promptly removed, leaving him with healing stitches. To make matters worse, Gibson was hit with a severe urinary tract infection that left him bedridden and drained of energy.
But Gibson’s story doesn’t end there — it’s just the beginning of his remarkable recovery at Sheridan Memorial Hospital’s Transitional Care Unit. Gibson affectionately refers to his time in TCU as “the resurrection of Charlie Gibson,” and the team of physical therapists worked with him, pushing him to regain his strength and balance. But, they didn’t just put him through the paces — they made it fun.
Gibson said the highlight of his stay was undoubtedly the decathlon the physical therapists organized for him. Inspired by the Olympic Games that were on TV during his first two weeks at the hospital, Gibson joked that in his next life, he’d come back as a decathlete. The staff took him at his word and set up a series of challenges that included boxing, throwing a javelin (made from a pool noodle), bowling and more. For Gibson, this event wasn’t just a series of exercises; it was a testament to his resilience and spirit.
“I developed the decathlon for Mr. Gibson after being inspired by the fact that even at 91 years old he displayed an unwavering work ethic and determination to overcome any challenge life put in front of him,” said Dawson Eppe, a physical therapy assistant, who worked with Gibson. “I am a firm believer that everyone is an athlete no matter their mobility or age, and the therapy and exercises we choose for treatment should scale with the patient and reflect that.”
The decathlon wasn’t easy. With his recent surgeries and infections, Gibson found the challenges both taxing and exhilarating, but he didn’t back down. With determination and the encouragement of his therapists, Gibson completed every event, even managing to climb the podium at the end. His efforts were rewarded with a gold medal, a symbol of his triumph over adversity.
Throughout his stay, Gibson found the key to recovery was more than just physical therapy. It was about staying positive, listening to happy music, laughing and accepting challenges — even when they seemed insurmountable. These principles guided him throughout his life, from his career with the U.S. Forest Service to his passion for poetry and art in retirement.
Gibson’s story is one of courage, humor and an indomitable spirit. He’s now looking forward to returning home, where he’ll continue his recovery and resume the active life he’s always enjoyed. He knows it will take time to get back into his routine, but he’s ready for the challenge.
For anyone who might find themselves in a similar situation, Charlie has a simple message: “Don’t just lay around. You don’t get well doing that. You need someone to kick you in the butt every day and get you moving.” And if you’re lucky enough to be at Sheridan Memorial Hospital Transitional Care, you’ll have a team of people ready to do just that — with a smile, a laugh, and maybe even a gold medal to reward your efforts.
If you or a loved one have spent three nights in the hospital and still need additional care before returning home, ask your case worker or physician about Transitional Care at Sheridan Memorial Hospital. Our Transitional Care program offers a supportive environment where you can continue your recovery close to home.
Javelin (made from a pool noodle)
Boxing
Bowling
Receiving the Gold

Sheridan Memorial Hospital Foundation celebrates new and outgoing directors on the SMH Foundation Board
During their annual meeting on July 23, 2024, The Sheridan Memorial Hospital (SMH) Foundation recognized outgoing board directors and welcomed two community members to serve on The Foundation board.
Outgoing Foundation board directors – Vicki Jorgenson and Rob Johnson
With much gratitude for sharing their time, talents and passion, The Foundation announces the departure of two valued board members, Vicki Jorgenson and Rob Johnson. Both served six years and were instrumental in the growth and success of the SMH Foundation during their tenure on the board. Their dedication to The Foundation’s mission has been a driving force behind our fundraising efforts and community outreach initiatives. The Foundation leadership thanked them for their service and wished them all the best in their future endeavors during the annual meeting.
“Vicki’s been an incredible supporter of our community hospital for decades. She is a quiet connector who cares deeply for our community. Vicki’s legacy of kindness and support will always be a part of SMH,” shares hospital and Foundation Chief Development Officer, Cody Sinclair. “Rob Johnson is a pillar of professionalism and thoughtful leadership. It was an absolute pleasure to witness the Foundation’s success under Rob’s calm and steady leadership as Board President over the last two years,” Sinclair expressed.
New board directors – Mikole Bede Soto & Gary Campbell
The Sheridan Memorial Hospital Foundation is excited to announce the addition of two new Foundation board members – Mikole Bede Soto and Gary Campbell.
Mikole was raised in Sheridan and then attended the University of Wyoming, where she received a B.A. in History and Political Science and a Master’s in History. After receiving her Juris Doctorate degree from the University of Wyoming in 2017, Mikole Bede Soto joined Chapman Valdez & Lansing in 2018 in the Sheridan office.
Mikole finds it important to be engaged in the Sheridan community. Currently, she serves on the Sheridan Chamber of Commerce Board, KidsLife Board, and Museum of the Bighorns Board. Mikole is also a graduate of the 2020-2021 Sheridan County Leadership class. “The hospital is such a pillar of our community. Having excellent healthcare in our community is part of what makes Sheridan so special,” shared Mikole. “I look forward to helping contribute to this asset in our community and ensuring it is here for everyone.”
When able to adventure, Mikole enjoys spending time outdoors with her husband, Austin, daughter, Marley, and their dogs and horses. Occasionally, Mikole teaches cooking classes at her family’s business, Verdello.
On behalf of the entire Foundation Board & staff, Sinclair highlighted, “The Foundation Board is thrilled to have Mikole join our team. She has a wonderful perspective being engaged in the community around her. Her skills, talents and dedication to serving our community excites our entire team and we look forward to working alongside her.”
Gary Campbell grew up in Sheridan and earned a bachelor’s degree in civil engineering at the University of Wyoming. His career included working with the U.S. Forest Service across National Forests throughout the country as well as leadership positions in Washington D.C. Gary ended his career with the Bureau of Reclamation and oversaw many large water projects across nine states in the Western United States. Gary brings a wealth of knowledge and experience. “Coming back to Sheridan brought out a desire to serve the community that gave so much to me. Having family members who have experienced a lot in healthcare systems, I feel that I can truly help to support and make a difference for others, to ensure that they all have the excellent care they deserve,” says Campbell. “Serving on The Foundation Board is the exact opportunity I was looking for to give back and really connect.”
After a decorated and extensive career, Gary is now retried back in Sheridan, the community he has always called home. Gary is an avid outdoorsman and likes to hunt and fish. You can often find Gary with his family: wife – Cindy, his son Justin and wife Katie also of Sheridan, and visiting daughter Ronni in Reno, Nevada.
“When you meet Gary, he exudes professionalism and kindness. His passion and thoughtfulness are always apparent and just what we look for in a board member. He has so much to offer our hospital and Foundation. Our team is looking forward to sharing and learning from him,” expressed Sinclair.
Looking ahead
The Foundation team is inspired by the leadership, passion, and community spirit of our board. The Foundation welcomes Mikole Bede Soto and Gary Campbell and express gratitude for the involvement and contributions of the other Foundation board members: President Sue Belish, Vice President Wendy Smith, Secretary Yvonne Gatley, Treasurer Chuck Burgess and at-large directors Dr. Bill Doughty, Richard Garber, Ryan Franklin, Rosemary Rieder and Dr. Joshua Scott. Their diverse backgrounds and dedication to service will strengthen efforts to support Sheridan Memorial Hospital in providing exceptional healthcare to our community.
To get the most up-to-date Foundation information and learn more about The Board of Directors, visit sheridanhospital.org/foundation or call our Foundation Team at 307.673.2418.
While commercials often highlight allergy season by depicting an array of green grasses, flowers and pollen floating through the air, the timing of allergy season depends heavily on an individual’s specific sensitivity and can take place throughout the year.
For Sheridan resident, teacher and photographer Tim Doolin, allergy season centers primarily around the fall archery elk season.
“Starting in my mid-30s, I began to develop quite a number of seasonal allergies,” Doolin said. “As time elapsed, those allergies began to disrupt my way of life, causing me to wake up at all hours of the night, with my nose just streaming.”
Doolin said he realized his respiratory health was being affected by the allergies and decided to seek treatment.
He began his initial appointments in Billings, as he was unaware Sheridan Memorial Hospital offered allergy testing and treatments. Dr. Cheryl Varner’s team at SMH’s Ear, Nose and Throat Clinic administered the treatments regularly to allow Doolin to stay closer to home for his care. Eventually, Doolin opted to switch, putting the direction of his allergy treatments under Varner’s team at SMH.
“The relationship that I had developed with the office, Dr. Varner, and all of the nurses in Dr. Varner’s office was something that I didn’t want to disrupt or change,” Doolin said, adding that with the help of the SMH Ear, Nose and Throat Clinic, he petitioned Blue Cross Blue Shield to cover additional allergy testing. “I had that testing done recently with Dr. Varner‘s office and was quite impressed with how thorough and comprehensive the testing was. The tests done here at Sheridan Memorial Hospital were far more thorough and extensive than those I received initially through my treatment in Billings.”
“I have high hopes that this continued treatment with a more comprehensive and refined approach to the serums I will be receiving will actually improve my allergy response even more than the benefits I have already experienced,” Doolin added.
According to SMH’s Ear, Nose and Throat Clinic, an allergy is a condition in which the immune system reacts to something eaten or in the environment that doesn’t affect most other people. People often think of allergy symptoms as sneezing, runny nose, nasal stuffiness and itchy, watery eyes.
However, allergies can also cause symptoms such as postnasal drip, head congestion, frequent “colds,” recurring ear infections, hearing loss, dizziness, chronic cough and asthma. Even stomach and intestinal problems, skin rashes, chronic headaches and fatigue can be symptoms of an allergy.
Various treatments exist for those suffering from an allergy or multiple allergies. Avoiding the allergen is often a first step when possible, followed at times by medications and immunotherapy. Sheridan Memorial Hospital’s Ear, Nose and Throat Clinic works with each individual patient to develop an allergy testing and treatment plan.
Doolin said the staff at Sheridan Memorial Hospital treats patients with care and like an extended family.
“Every week throughout the year, there are quite a number of us who receive this allergy shot therapy, and without fail, the conversations revolve around grandchildren, children, holiday and summer plans, and life in general,” Doolin said. “It really is like a small knit little family and the community is quite positive and something I appreciate.”
To schedule an appointment with the Ear, Nose and Throat Clinic at Sheridan Memorial Hospital call 307.675.4646 or to learn more see sheridanhospital.org/medical-services/clinics/ear-nose-throat.
Bonnie Brester had a rough year. Her husband, Mark, died in July 2022, and about six months later, Brester received a breast cancer diagnosis that would change not only her outlook on life but where she would call home.
Brester began treatment for the cancer in January, but about three days after one of her chemotherapy treatments her condition quickly declined.
“I had developed neuropathy and I was going to have to learn to walk all over again,” Brester said. “I needed emotional support. I needed physical therapy. I needed a place that could care for me throughout the day.”
While she had lived in Billings, Montana, with her husband prior to his passing, Brester knew her new situation wouldn’t allow for that independence. She moved to Sheridan and began receiving care in Sheridan Memorial Hospital’s Transitional Care Unit, which provides a recuperative and supportive place to heal following injury, surgery or serious illness. For Brester, Sheridan Memorial Hospital’s TCU meant she could be closer to family because her son, Dusty, and his wife, Jamie, live in Sheridan.
“I can’t say enough about all the great people at Sheridan’s TCU unit,” Jamie Brester said. “My mother has been in TCU twice for short amounts of time and just recently, my mother-in-law spent approximately 90 days there.”
“…Having her in Montana and us down here was not an option,” Jamie Brester said of her mother-in-law. “Bonnie was released to the TCU in July after Billings providers had told us to start looking at hospice options.
“When she got to Sheridan, chemotherapy had taken so much out of her she could not walk or eat and was not comprehensive most of the time. We thought we were going to lose her,” Jamie Brester added. “Once she got to Sheridan, everything changed. Bonnie started to feed herself, started physical therapy and really started to live again.”
The new TCU space at Sheridan Memorial Hospital opened in the fall of 2022, after several years of planning and construction. The new space, located on the second and third floors of the original 1954 hospital, includes 20 private suites for those needing time, space and help in healing.
“The first year has been full of celebrations, lessons, growth and achievements,” said Ashlee Winne, TCU manager. “I really enjoy seeing the progress the patients make. They come in sometimes at the hardest times of their lives and by the time they leave are often in better condition and spirits than before whatever illness or injury brought them to TCU. It really is a blessing to watch each patient’s individual journey.”
Now open for more than one year, TCU has served more than 188 individuals.
Bonnie Brester spent 100 days in TCU, relearning the skills she would need to live at home. She relearned how to walk. She practiced balance that would allow her to reach for a glass out of the cupboard and conduct daily personal hygiene. She worked hard to build the strength needed to get in and out of vehicles and step over and onto curbs.
“Everybody was so enthusiastic and so patient with me,” Brester said. “One of the first times I was able to walk with my walker, there were several nurses there cheering me on. It was a whole cheering section just for me.”
Patients on the TCU have an entire team of healthcare professionals available to help in the healing process. The team includes nurses, nurses’ aides, physical therapists, occupational therapists, speech therapists, nurse practitioners, doctors, case managers and more.
Thanks to that team, Bonnie Brester said she feels ready to live with Dusty, Jamie and their family in Sheridan.
“The people here at TCU have really given me a lot of support and a lot of good therapy,” Brester said. “The biggest thing I had to learn was to believe in myself, that I could do this. It was hard for me, but everyone was so encouraging. They wouldn’t let me go home if they weren’t sure I was ready.”
Jamie Brester said their family owes Bonnie Brester’s progress to the staff at SMH.
“Bonnie has been back home for a few weeks now, but misses her connections from the hospital,” she said. “She made friends with just about everyone there. I really believe the environment allowed her to thrive and she became determined to win at this game called life.”
Jade Stanley, a local Sheridan resident, is the first Sheridan Memorial Hospital (SMH) patient to undergo hysterectomy surgery using state-of-the-art da Vinci® robotics. Stanley underwent the hysterectomy at the hospital in December and has been sharing of her positive experience since.
When asked why she chose SMH to perform her hysterectomy, Stanley said, “Our local hospital has great services, and I feel very comfortable there. The staff are all friendly, and the doctors are very knowledgeable. The SMH Women’s Clinic also delivered my child, so I wanted to stick with the people that knew my history.”
Rebecca Krzyminski, DO, one of the physicians at the Women’s Clinic who is specially trained in robotic-assisted surgery, performed the operation. Stanley had previously worked with Dr. Krzyminski, having glowing words for the staff and doctor, calling them “very knowledgeable,” “professional,” and “down to earth.” Stanley continued to share that the team at SMH “are all friendly and eager to assist. Dr. Krzyminski’s confidence is contagious.”
Stanley also spoke positively of her recovery, saying, “It’s been great.” She was able to walk out of the hospital the same day as her surgery and has been going ever since.
When asked if she would recommend SMH and robotic surgery to potential patients, Stanley said, “If you’ve got a hospital as great as this one in your neck of the woods, why go anywhere else? I would tell them not to be afraid. My recovery was virtually painless. It’s definitely the way to go.”
SMH is committed to providing excellent, patient-centered care with an outstanding healthcare team and state-of-the-art technology right here at home. Robotic-assisted surgeries are now available for anyone needing procedures such as hysterectomies, hernia repair, endometriosis, gall bladder removal, ovary removal, and prostate biopsy/removal.
To learn more about Sheridan Memorial Hospital’s minimally invasive robotic-assisted surgery, visit SheridanRoboticSurgery.com and Robotic-Assisted Surgery FAQs.

Each year in February, we celebrate National Cardiac Rehabilitation Week to draw attention to the role of cardiac rehab in reducing the potentially devastating effects of heart disease. In Sheridan, we are lucky to have many exceptional services to support heart health, from the cardiology team at the Heart Center, to our Cardiac Catheterization Lab and state-of-the-art ICU at Sheridan Memorial Hospital. After having a heart attack, being diagnosed with heart failure, or after a heart procedure like a coronary artery bypass, coronary stent placement, or valve replacement, Sheridan Memorial Hospital’s nationally accredited Cardiopulmonary Rehab program provides support to help you recover.
Checking in on Tom McClain, Cardiopulmonary Rehab patient
 Just over a year ago, we told you about Tom McClain, who has been in the SMH Cardiopulmonary Rehab program since 2019. We thought we would check in on him and learned that he continues to participate in the maintenance program, now logging over 320 sessions over the last three years!
Just over a year ago, we told you about Tom McClain, who has been in the SMH Cardiopulmonary Rehab program since 2019. We thought we would check in on him and learned that he continues to participate in the maintenance program, now logging over 320 sessions over the last three years!
Tom says that since we last talked to him, he had cardiac ablation, a procedure to block his heart from producing irregular or abnormal rhythms, and also had his pacemaker replaced.
He is very grateful to have the program and the beautiful space to work out in. “This is a safe place for cardiac and pulmonary patients, and that’s why I come here. It makes me feel better, and it’s not hard to make myself come because there are people here who are expecting me. Coming to exercise here is just part of my weekly routine.”
He still considers himself one of our “regulars,” saying: “I come twice a week. Socialization is really important to me – there are three of us who come at the same time, and it makes exercising fun. We have a lot in common and encourage each other to do our best. I live alone and really look forward to spending time here.”
“What I particularly like about the hospital program is that there is always a nurse or staff member who monitors me – taking my blood pressure and checking my oxygen levels as I go about my workout. It’s comforting to have a professional on hand, observing me and making sure I’m doing ok. Besides that, I’m on oxygen, and it is so convenient that I can just plug my oxygen line into the wall as I exercise,” Tom adds.
He has also participated in the educational classes offered to patients in the Pulmonary Rehab program.
According to Cassie Mullins, RN, SMH Cardiopulmonary Rehab Supervisor, “Because our patients come so often, the Cardiopulmonary staff really gets to know each individual. A typical program runs from 18-36 sessions, so we learn a lot about our patients: their likes and dislikes, what they care about, and the goals they have. This also helps us develop a plan together with the patient, to reduce their risk of developing worsening heart disease. It can also help us provide continued encouragement for the individual to accomplish a health goal like quitting smoking. If our patients don’t show up, we call to check on them and encourage them to continue their workouts.”
More about the program
Our Cardiac Rehab program has two phases. The first phase of cardiac rehab is the monitored exercise phase. During this time, your doctor can order up to 36 closely monitored exercise sessions for you to complete. We encourage our patients to work up to exercising 3 times a week with us. After graduating from the monitored exercise program, we encourage our patients to continue to exercise! During the maintenance phase, we provide the opportunity for our patients to continue exercising in our gym with less monitoring. The ultimate goal is for our patients to feel safe and confident participating in whatever kind of exercise they enjoy, whether in a cardiac rehab setting, at home, or in the community.
If you have had a heart attack, heart failure, or a heart procedure, ask your doctor if you could be eligible to be enrolled in cardiac rehab. For more information, call Cardiopulmonary Rehab at Sheridan Memorial Hospital at 307.672.1062.

Anne Hinman was kind enough to leave this 5 star google review about Sheridan Memorial Hospital’s Wyoming Rehab: “I could not have been happier with the treatment and personal care of this team! I messed up my back and was in a lot of pain. Jeanne was able to squeeze me in for a consultation and really took the time to figure out where my pain was coming from and how to treat it. Highly recommend this clinic.”
Anne said a friend of hers recommended Wyoming Rehab – so she went to the hospital’s website and learned about the Free Screenings for non-emergent issues.
“I am a bit embarrassed to say that I had begun lifting weights and was experiencing “very much” pain – I’m 27 and was scared that I had really done something bad to my back and I hoped that physical therapy might help. It was awesome that Jeanne Brooks could fit me in the same day as I called Wyoming Rehab.
Jeanne checked out my back and walked me through some activities and motions that helped loosen up my back. It was a lot more help than I was expecting on a screening visit. Jeanne also gave me a list of things that I could do on my own to help alleviate the pain and relax my back.
Jeanne also said that I was welcome to come back for more help if need be, but I am doing fine on my own now. If I ever have an injury, I know I would go back to Wyoming Rehab.”
If you have nagging aches or pains, give Wyoming Rehab a call today to schedule a non-emergent free screening – 307.674.1632.

For most people, Sheridan, WY is a place to come when you want to get away from the crowds yet still crave the comforts of a small town. For Sig Palm, the deciding factor to come to Sheridan was having local access to exceptional healthcare.
 Sig’s first introduction to Sheridan came in 1967, while on a trip to meet with the forest supervisor and his primary staff. Sig was a newlywed, freshly off active duty in the Army, and brand new to the Forest Service. That day kicked off a pivotal Forest Service career spanning fifty-eight years and numerous states. While the bulk of his working years took him far away from Sheridan, he never forgot how at home he felt there. Unforeseen to him at the time, Sheridan would become the place he relied on to manage numerous health concerns ranging from minor to extensive.
Sig’s first introduction to Sheridan came in 1967, while on a trip to meet with the forest supervisor and his primary staff. Sig was a newlywed, freshly off active duty in the Army, and brand new to the Forest Service. That day kicked off a pivotal Forest Service career spanning fifty-eight years and numerous states. While the bulk of his working years took him far away from Sheridan, he never forgot how at home he felt there. Unforeseen to him at the time, Sheridan would become the place he relied on to manage numerous health concerns ranging from minor to extensive.
Sig is no stranger to heart problems – both his maternal grandfather and his mother died of congestive heart failure. Around the age of 11, Sig realized he had inherited the same heart trouble. “I knew about it because I didn’t have the stamina that other kids did, like in PE.” So, it was of little shock to Sig when in 2012, on a Boy Scout trip to Yellowstone with his grandson, he went into congestive heart failure.
At that time, Sig and his wife Judi were living in Colorado Springs but contemplating a return move to Sheridan. “Sheridan is where we felt most at home. Our kids were born around here, and we kept in touch with our friends.” But for Sig and Judi, they couldn’t base their decision to move back solely on feelings – the scare on that Yellowstone Boy Scout trip made proximity to specialized healthcare the number one determinant in where they would live. Armed with a list of Sheridan doctors suggested by his physician in Colorado Springs, Sig set to work researching. “The most important thing to me at the time was the heart center and what it offered. I told them what I had going on, and Dr. Brennan came highly recommended.” What he found in researching Sheridan Memorial Hospital Heart Center sealed the deal – after decades away, they were coming home to Sheridan.
Since their move back to Sheridan, Sig has run the gamut with hospital specialties. From Cardiology, Orthopedics, and Wyoming Rehab to Internal Medicine and The Welch Cancer Center – he has been a patient of each. Sig recalls a conversation he had with Dr. Megan Ratterman, Oncologist at the Welch Cancer Center, when he was diagnosed with Multiple Myeloma. She said, “I won’t feel offended if you want a second opinion.” Sig thought about it and decided, “Nah. You know, I want to stick with the Sheridan team. I trust their counsel.”
Sig understands he has options for care. He has chosen to stay here at SMH. For Sig, the ability to receive the care he needs locally made all the difference. “Everyone I have ever came in contact with at the hospital has been just beyond wonderful.”
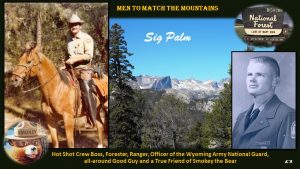 For more information about the many exceptional services offered at Sheridan Memorial Hospital, visit our website at www.SheridanHospital.org.
For more information about the many exceptional services offered at Sheridan Memorial Hospital, visit our website at www.SheridanHospital.org.
Robert Kessler has led a full life for sure. He has lived in Buffalo, WY, since 1964. He has been in the Navy, run his own business in Buffalo, and then went back to school for a teaching degree and taught school in Ranchester and Buffalo for 20 years. To say he is always on the move is an understatement.
But in 1972, Robert “broke his knee” and a little lump developed behind his knee that never went away. Then, recently while traveling in Australia, his knee became very painful. Once home, he went to the VA Hospital in Sheridan and in May of 2019 received a diagnosis of soft tissue sarcoma (cancer) in that lump.
After radiation and surgery, additional cancer was found in the lymph nodes of his thigh . That’s when the chemotherapy started.
“It was a pretty tough regimen and I know now why people hate chemo,” Robert stated. “You get to a point where you wonder if it’s worth it.”
After receiving the first round of chemo in Salt Lake City, Robert was able to transition his care to the Welch Cancer Center (Welch) in Sheridan for the next round.
“It’s 30 minutes away instead of eight hours,” Robert said, “and it meant a lot.”
Robert started the second regimen at the Welch in 2020 after a PET scan revealed the first round had not done its job. Having his treatment close to home made it much more palatable.
“This time, I was able to be home and that was very helpful and comforting,” he said.
However, after the second round of chemo, he was told by his doctors in Salt Lake that the cancer was still progressing and the prognosis was dim.
“I asked them how long I had, and they told me 12 months. So I started to get my affairs in order, as they say, to make sure my family was taken care of. I even bought a stone and put my name on it. I cried all the way home from Salt Lake,” Robert said.
Lucky for Robert, shortly after that hard-to-swallow conversation, a new drug hit the market. Robert and his cancer care teams agreed it would be good to try.
“And after visiting with Dr. Ratterman, it was determined I could get the treatment at the Welch,” he added. “The coordination between the team in Salt Lake and the Welch was amazing. Very professional.”
The new treatment began in October of 2020 and the following April, another PET scan revealed a significant improvement, so additional treatment was in order. Another scan after that showed even more improvement.
“We pretty much have it on the run, but cancer is diabolically sneaky,” Robert said. “This coming February, I will have my 17th treatment of the new drug regimen. We will keep going as long as it keeps working and my immune system continues to tolerate it.”
There are a few lingering effects from all the cancer care, but he says things are good now, “I feel good and it isn’t slowing me down. I do everything I used to do, only a little slower. I have no after-effects from the treatments. After my last infusion, we got in the car and drove to Arizona.”
Robert has high praise for the teams that continue to keep him going. He says the coordination of care between all the teams was professional and the level of respect was very evident. He adds that he felt the knowledge base of the Welch team was great and he never had to wait for an answer.
“The level of care at the Welch was fantastic and I would encourage anyone needing cancer care to visit with the team at the Welch,” he said emphatically.
With a little chuckle, he adds, “They have done a great job of keeping me alive two years after my expiration date. But in all seriousness, I have nothing but glowing respect and admiration for Dr. Ratterman and Nurse Practitioner Nina Beach and the whole team of nurses at the Welch. I always feel like they are treating one of their own family when I see them. They are very caring people and they never treated me as if I was going to die.”
Anyone wanting to learn more about services provided at The Welch Cancer Center please visit https://www.sheridanhospital.org/medical-services/welch-cancer-center/ or call 307.674.6022.

The challenges that come with a debilitating injury are more than physical. The mental challenges of not being able to do things that came easy prior to the injury can be beyond frustrating. And the baby steps it sometimes takes to get back to “normal” can seem to take forever.
Matt Kemerling’s shoulder injury from a workplace mishap took him through some very challenging times. “I separated my biceps from my shoulder is how the doctor described it to me,” Kemerling stated. “The news that I had to have surgery just shattered me. But the doctor assured me that the surgery followed by a strong physical therapy regimen I could get back to normal.”
Kemerling admits his first thoughts about physical therapy were “that it’s a waste of time. I wasn’t a big believer in it.” But he was willing to give it a try and after the surgery he got to work with Charlotte Walter and Mike Duncan at Wyoming Rehab.
“I don’t think I could have been more fortunate to work with two people who fit my personality better,” Kemerling said. “I was super impressed with them both. They are super motivators and helped drive me to get done what I needed to get done.”
The regimen was three days a week to start and slowed to two days as progress was made.
“As we started doing therapy at the (Wyoming Rehab) facility and I did my homework, I saw improvements and that was a huge factor in my motivation,” Kemerling added. “Just the way Charlotte and Mike listened and talked to me really raised my spirits and helped with the mental aspect of dealing with this injury. That was so important.”
Kemerling was impressed with Walter and Duncan’s approach to therapy, the way they kept his goals in front of him and how they were invested in his success.
“The relationships I developed with the team at Wyoming Rehab were amazing and it was a little sad when I was done with my therapy and had to tell Charlotte and Mike good-bye,” Kemerling said. “It was an awesome experience, with a very professional team and I would recommend them to anyone.”
Learn more about Wyoming Rehab services by following the link sheridanhospital.org/medical-services/rehabilitation-services/ Specific exercises and stretches from a qualified professional at Wyoming Rehab will alleviate and can prevent common health problems. Call Wyoming Rehab today to set up a free screening for non-emergent physical impairments or injuries – 307.674.1632.

Adriane Duff isn’t the type of person to sit down and just tell you about her life and her healthcare history. In her own humble way, she wants to “help others” and in telling her story, she hopes to offer encouragement.
“I don’t want this story to be about me,” she says right up front. “I’m hoping that by telling my story this way, I can help others by encouraging them.”
When you hear her story, it’s doesn’t sound that different from many people you know. Except for the chemo, the radiation and don’t forget that bone marrow transplant in 1990. After being diagnosed with Hodgkin’s Lymphoma in 1989, rounds of chemo and radiation couldn’t eliminate the disease.
“That’s when they decided to try the bone marrow transplant,” she says. “Back then, that was highly experimental for anything other than leukemia.”
It must have worked, because she was healthy, other than a suppressed immune system which they told her would happen and would get worse the longer she lived.
Fast forward to 2014, it’s a Sunday morning, Adriane thought she was having an asthma attack.
“I was coming up the stairs in my home and I could feel my heart beating in my head. I sat down, took my pulse and thought, ummm, 40, that’s not a good pulse,” she says with a chuckle. “I told my husband we need to go to the ER.”
It was there, in the ER on that Sunday that Adriane’s experience with Sheridan Memorial Hospital (SMH) began.
“Dr. Brennan was there to see me in about 30 minutes, on a Sunday no less,” she exclaims. “He is a very sweet man. He has a heart for people and you can see it in how he cares for you.”
The diagnosis? A pacemaker needed to be installed to regulate her heart rate. But complications from radiation treatments years ago made that a struggle. The leads for the pacemaker were not able to be run through her veins which had been severely constricted due to the radiation treatments from years ago. Her chest would have to be opened up to install the device.
Adriane says she has been told by doctors she is a very unique patient.
“I guess they say that because I have survived a bone marrow transplant as long as I have,” she says with a big grin. “All these health issues can be traced back to that. I just keep working through whatever comes up and I’m very thankful to everyone who has helped keep me healthy.”
Adriane hopes she can encourage people by telling her story.
“There are so many people to thank. People from the Heart Center to Wyoming Rehab to the clinic, I can’t even name them all. They have all been just great and worked to find solutions for me.”
“The doctors have always been very good about working with me. If anything happens, I know they’ll take care of me. We have some very, very good health professionals here. They are here for the community and have our best interest at heart.”
Adriane is retired now and spends most of her days at home with her happy little dachshund, Carlin. She still has to be careful to not contract an infection, but says she gets out as much as she can, takes every necessary precaution and absolutely loves living in Sheridan.

9-1-1 HEART ATTACK
After his heart attack, Ron was given a second chance at life. He was determined not to waste it.
Update – Ron Richter – In His Own Words: 4 Years After a Heart Attack
I feel much better today than I did prior to my heart attack on January 17, 2017. I still have bad days, but the good days outnumber the bad ones tenfold. Although I feel much better, I do realize that I will be living with heart disease for the rest of my life.
Changes have been extensive, as a healthy diet and regular exercise have become part of my daily life. I’ve lost a lot of weight, initially around 70 pounds. I’ve gained about 10 of that back from lifting weights and what not, but I know the weight loss has helped my heart immensely and has also helped with my sleep apnea.
I make sure to limit my daily sodium intake and try and stay away from foods high in saturated fat, cholesterol and preservatives. My exercise routine includes a lot of bicycling and playing basketball, as they are both great forms of cardiovascular exercise, which of course is good for the heart and helps with my high blood pressure. Another change I’ve made is I’ve been smoke free since February of 2017. I smoked a pack to two packs of cigarettes a day for over 20 years. During my first visit to the Heart Center at Sheridan Memorial Hospital (SMH) following my attack, I asked Dr. Garcia what was the main reason for me having a heart attack at such a young age, and he said smoking…..that’s all I needed to hear. I haven’t touched a cigarette since.
The hardest thing to change has probably been my diet. It was a little overwhelming at first, as I quickly realized that most, if not all of the food I had been eating had little, if any nutritional value, and was nowhere near heart healthy. Grocery shopping became an experience, as reading the nutritional content became the norm in an effort to limit my daily intake of sodium, cholesterol, and saturated fat. Now I know what to buy and what not to buy, so that part has become much easier.
Aside from my six-month check-ups at the SMH Heart Center, I really haven’t stayed in touch with the people that were responsible for giving me a second chance at life. While I may not keep in touch with any of them, I appreciate every single person that played a role in helping me stay on this planet a little longer. I appreciate them all, everyone from the EMT’s with Rocky Mountain Ambulance and Sheridan Fire-Rescue, to the team at the ER and Cardiac Cath lab, and of course, Dr. Garcia. Because without all of them, I most likely wouldn’t be writing these words today.
As far as advice, if you think you may be a candidate for heart issues, talk with your doctor and make sure to check your blood pressure regularly. Keep an eye on your cholesterol levels and be proactive, not reactive about any and all issues regarding your heart health.
Click below to see the original video from 2017 where Ron talks about the great care he received from the Sheridan Memorial Heart Center after his heart attack.
MEDICAL EXCELLENCE – right here at home
Stacy Windon was a recent patient in Sheridan Memorial Hospital. Below is her experience in her own words.
My fiancé and I both work at VA. When the COVID-19 vaccinations became available, I was adamant he receive the vaccine due to his COPD. I was insistent because I thought it was easier for him to get sick and that he could be extremely sick if he contracted COVID.
At the time, I didn’t get vaccinated, I was hesitant because the vaccine had not been FDA approved, I was leery; plus, I was healthy.
In early August (4th & 5th) we both tested positive for COVID. The difference in our experiences is that he was back to work by the 9th due to being vaccinated; I was in the hospital by the end of the week and had to stay for nine (9) days. I was shaking, I couldn’t breathe, I couldn’t move, I was not always coherent; it was the scariest time in my life.
Everyone at the hospital was wonderful; the kitchen staff, housekeepers, nurses, CNAs and the doctors. They treated me with respect, never like I was in danger, and I learned a lot from all of them about this virus.
Now, based on instructions from my physician, I have to wait 60 days until I can get the vaccine. In the meantime, I have to make sure I don’t get sick again.
I’m sitting here at home, I can’t get a good breath, I’m on oxygen, I can’t really get around my house. I tried cleaning house recently and the next day I paid for it. I’m carrying a 50 foot air hose everywhere I go in my house.
My advice to those who are questioning the vaccine, if you’re scared, research it. Listen to other people who have had it. Please, please ask questions and make an informed decision. This is not minor by any means. Stacy Windon

A first-hand account from recent Urgent Care patient, Janet Dale:
My recent experience at Urgent Care at Sheridan Memorial Hospital was a very positive one.
In early July I noticed a spot on my right shin. At the time I thought it was a bug bite, perhaps an ingrown hair or even a pimple. It did itch a bit, but I thought it would just go away. As time went on, I became concerned because it was not healing but getting worse – it was oozing and getting bigger. I kept it covered most of the time with a band-aid.
Finally, on July 25, I looked for Urgent Care Facilities in Sheridan. I live on the mountain near Burgess Junction so I didn’t want to make a lot of trips to town. I easily discovered Urgent Care at Sheridan Memorial Hospital. The website was great and so easy to use. I scheduled my appointment online at a time that was convenient for me, filled out my paperwork online and had the appointment the following day. I even received confirmation of the appointment online and also received a reminder phone call!
Check-in at Urgent Care was easy. I felt very comfortable and everyone was wearing a mask. I was in with the nurse almost immediately. She was friendly and efficient.
Dr. Nickerson came in and introduced himself and asked why I was in. He looked at my leg and told me the sore was not infected but the spot did need to be removed and a biopsy completed. He told me he could do that today or, if I preferred, I could make an appointment with a dermatologist.
We discussed how he would do the office surgery and making sure that enough was removed to have clear margins. I made the choice of having the spot removed in the office. I did not want to possibly wait weeks to get another appointment and have this spot continue to get worse. Dr. Nickerson was wonderful in making sure the spot was numb and I would not have any pain. He showed me the area that he removed and said it would go to the lab. At that time he asked me to come back in two weeks for stitch removal.
Several days later I called for the lab results. Dr. Nickerson was out of the office, but the nurse practitioner reviewed my results. The biopsy was malignant but thankfully the margins were clear. She carefully reviewed what that meant. I felt very comfortable after talking with her. She reiterated that I needed to come in to get my stitches removed and that was included in the cost of my original visit. There would be no additional charge.
My visit for stitch removal went with no problems. Again, I scheduled my visit online and everything was smooth. I received a reminder message and was immediately taken care of upon my arrival.
I could not be more pleased with the care that I received from Dr. Nickerson and his staff.
Janet Dale
To learn more about Sheridan Memorial Hospital’s Urgent Care or to reserve your spot online visit SheridanUrgentCare.com or call 307.675.5850.

Vera Olson was suffering from more than illness when first admitted into the Transitional Care Unit (TCU) at Sheridan Memorial Hospital in February 2019. On top of experiencing atrial fibrillation and viral sepsis, she was grieving the very recent death of her daughter.
For Vera, looking back today, that first six-week stay in the recuperative wing blurs together. However, one element remains salient: the kindness of the TCU nurses and physical therapists (PT).
“They watched me, they worked with me when I got stronger, they kept the exercises interesting,” Vera remembered. “They made it fun. The TCU [team] seemed to work so well together. It was the highlight of my day.”
“She loved doing therapy with us,” Tiffany Sutton, PT noted. “Even when she was exhausted and sad, she would still come and try to do things with us. We did the therapy, of course, that’s a big part of it — but we also helped her grieve and heal from her daughter’s passing.”
The TCU’s focus on healing patients both physically and mentally was not lost on Vera Olson.
“I will never forget the caring, the support, the lightness of it, and the encouragement that they give you,” she said.
With each day’s dose of exercise, sunshine, and laughter, Vera felt a bit stronger. When she was admitted, she could barely walk for 15 feet and keep her head up, even when assisted. By the time she was discharged, she could walk more than 400 feet independently.

To ease the transition, the TCU team set up home healthcare to visit Vera throughout the week, a service that she deeply appreciated.
“Anytime you can be at home, it’s good,” Vera said.
However, this was not her last trip to the TCU. Due to other health issues, Vera has returned twice more for shorter stays. She would not have returned if it were not such a good experience, she said. “Of all the places I received transitional care, Sheridan Memorial Hospital was by far the best! It was like family caring for me.”
Today, knowing that the TCU team is there for her when she needs them, “Is a very good feeling, very great, very warm,” according to Vera.
To learn more about Transitional Care visit https://www.sheridanhospital.org/medical-services/transitional-care today!

Some of life’s biggest moments are spent with a nurse. National Nurses Week provides the perfect opportunities to celebrate the nurses who care for us, our friends and our families. They have an important job to do, and we are grateful to them for being there for us. We put out a call to our community to share with us how an SMH nurse or nurses have been there for them. Now we share their words with you and the nurses with gratitude. Do you have a great nurse story to tell? Click HERE to tell us about it and recognize the nurse who made a difference in your life.

When Mary Skretteberg severely broke her ankle in September 2019, the prescription of a prolonged hospital stay felt like insult added to injury for the 79-year-old. But when she was discharged two months later, she said goodbye to the staff at Sheridan Memorial Hospital’s Transitional Care Unit (TCU) with tears in her eyes.
Skretteberg was surprised by the level of community she found at the TCU, a recuperative place to heal following an injury, surgery, or serious illness. “It was kind of like a college dormitory,” she explained. “You’re sharing a space: You’re sharing the dining room, you’re sharing the therapy, and you’re sharing your pains and aches and worries.”
By the end of her stay, Skretteberg felt at home in the halls of the TCU.
Today, Skretteberg is thrilled to be home with her husband. She continues to practice physical therapy and is “on the mend.”
And she continues to think fondly of her TCU family. Skretteberg hopes the TCU is able to add more beds “because the community is growing, and once you’re 50, 55, 60 years old, you start to break an ankle here, fall there — you need some time to recover in a hospital that doesn’t feel like a hospital.
“The TCU feels like TLC.”
To learn more about Transitional Care and the current Expansion Project, visit sheridanhospital.org/foundation today!

In early January 2020, Dr. Sy Thickman stepped outside for his usual dog walk. Awaiting him was a thin layer of snow covering thick black ice; he slipped and fell as soon as he reached the street.
“I live with a very dear friend and yelled out to her,” Dr. Thickman remembered. “I was lying in the snow — I couldn’t move at all.”
His friend called for an ambulance, and within 15 minutes, Dr. Thickman arrived at Sheridan Memorial Hospital (SMH). X-rays revealed a fractured hip, and an orthopedic surgeon recommended an operation as soon as possible. The very next day, Thickman underwent a successful surgery and was transferred to the Transitional Care Unit (TCU).
The TCU is a recuperative and supportive place to heal following an injury, surgery, or serious illness. An expert team of nurses, doctors, and physical therapists manages patients’ transitions from daily intensive care to returning home.
“Some people may think that if they lie in bed all day and seem to be doing better medically, they’re ready to go home,” said Tiffany Sutton, a longtime physical therapist and the TCU Rehab Coordinator. “But you need (physical therapy) so you can go safely home — and stay home.”
Sutton and her team frequently have to put on a cheerful show to entice patients to participate in the all-important but often uncomfortable physical therapy. A physician since 1946, Dr. Thickman didn’t need to “drink the Kool Aid,” Sutton said.
And yet, this was his first hospitalization in his then 96 years. Dr. Thickman was admittedly worried, especially when he wasn’t able to move his injured leg at all for many days.
“You begin to think occasionally of potential consequences that would not be uncommon at this age,” he said. “There was a period of hospitalization early on in which I wondered if I was going to be able to return to a normal way of life.”
Enter: the TCU team. The nurses kept Dr. Thickman company, encouraged him to enjoy his meals in the community dining space with his fellow patients, and made him as comfortable as possible. The physical therapists worked on his mobility with their creative methods meant to mimic activities of daily living. The doctors monitored his progress. Everyone lifted his mood.
“I really had such comfort with the staff,” Thickman said. “They came every day, and it was fun to expect them. Never did I have any concern that wasn’t fulfilled. I felt in good hands, and I was able to — if you don’t mind the expression — ‘have fun with it.’”
The feeling was mutual.
“He was very fun — a joy to have,” Sutton said. “He shared his wisdom with us, which was incredibly wonderful of him. He would joke around with us and talk to us about how medicine has progressed. Thirty years ago, this (level of physical therapy) would never have happened.”
After two weeks of progressive improvement, Dr. Thickman could move with a walker with comfort, dress, and care for himself on his own. He was ready to be discharged. The transition home came with more prescribed physical therapy that tapered off over another two months.
Today, at age 98, Dr. Thickman is able to walk without the assistance of a cane or walker. He attributes his complete recovery to the “excellent care” at Sheridan Memorial Hospital.
By Larry Certain February 20, 2021, posted here with his permission.
I feel fortunate to live in Sheridan County, and I am sure I’m not alone. Many of the nicest people live in our county, and a large number of them are employed by Sheridan Memorial Hospital.
We can, I feel, be thankful for the fine hospital and exceptional personnel staff working there. Having never required them in an emergency; I can now tell you they are the best. Having just experienced my first and only (I hope), heart attack, I observed real professionalism at work.
From the minute my wife and I walked up to the emergency window, things happened like clockwork. That was at about 6 a.m., a week ago last Saturday and by Monday morning, I was wheeled out with stents in the ol’ ticker, and a new lease on life.
I can never express the feelings I have for the doctors, nurses and staff members of our fine hospital. But it would start with exceptional. Doctors Selde, Schamber were first on the scene. Then doctors Brennan and Garcia followed. And Dr. Garcia and his fine staff were unbelievable. They were so fast, efficient and so empathic. It was unbelievable. Their knowledge and professionalism, in my opinion, is beyond reproach. Thank you, from the bottom of my indentured heart.
And the nursing staff of the ICU was the best ever, also., and put up with a curmudgeon with no desire to be there, who was always tangled up in tubes. My heartfelt “thank you.” I love you too. And the other members of the support staff in the kitchen, blood draw and house keeping — thanks for making my stay more tolerable.
So any of you, readers, watch for the signs that you should stop shoveling snow and get to the hospital as quick as possible, so you won’t get a side trip like I did. Shortness of breath, like an elephant sitting on your chest, feeling like someone slugged you in the stomach and throwing up. You might not be as lucky as I was.
Larry Certain
Sheridan

Connie Bachel, a longtime employee of Sheridan Memorial Hospital (SMH), contracted COVID-19 in mid-September.
Bachel and six of her co-workers at the SMH Urgent Care tested positive for the coronavirus, each exhibiting different symptoms. For the next two weeks, they recovered, checking in on each other’s progress and offering words of encouragement.
In early October, Bachel was feeling better, if not fully energized. But by mid-October, COVID-19 reasserted itself in full force, even worse than before. Bachel, suffering from gastrointestinal symptoms, did not immediately want to go to the emergency room.
“It was so embarrassing — I didn’t want to do that in my own sandbox,” she said. “But my husband said, ‘No, you’re going to have to be a patient.’”
Bachel was immediately admitted and placed in a COVID-19 isolation wing.
SMH has two dedicated wings for COVID-19 patients: one in the Intensive Care Unit for critically ill patients and the other on the Med Surg floor for those like Bachel who need to be admitted but don’t need ventilators. Experts across SMH departments have worked together to ensure these wings are as safe as possible for patients and staff.
“It’s very scientific,” said Lacey Johnson, the Med Surg Manager at SMH.
Because COVID-19 is an air-borne disease, Johnson explained, one of the most important elements of the isolation wings is the air flow. Partitioned off from the rest of the hospital, the hallways and rooms have negative air pressure. Instead of filtering, cleaning, and recirculating the air like in most buildings, the mechanics of the hospital bring in air and then send it directly back outdoors, without returning to the hospital. All doors and windows must remain closed to maintain the seal.
In addition, the few dedicated staff members who are allowed into the wings must be in full PPE: gown, gloves, booties, N-95 mask, eye cover, and hair bonnet or a capper.
The cleaning staff for the COVID-19 wings uses “terminal cleaning” agents and gear, the same used in Operating Rooms, a lengthier and more involved sterilizing process.
Perhaps most importantly, the medical team must be conscientious of the time spent in the wings.
“If we go in to deliver medications, we get them all at once,” Johnson said. “We bathe patients, change the bed, etcetera, all in that time frame.”
While crucial for safety, the COVID-19 isolation wings can be just that — isolating.
At the time, Bachel’s daughter, Megan Perkins, was a registered nurse at SMH. Due to the strict safety protocols, even she could not enter the room — only the dedicated on-duty nurse could be admitted.
Perkins herself had worked in the COVID-19 wing. She had seen family members’ frustration at being kept apart and knew the importance of lifting patients’ spirits when at their most ill.
“As a nurse, it’s hard to see your patients struggle that way,” Perkins said. “I saw how much it dropped their mood and their affect. It hurts people’s sense of well-being when they’re so isolated. But I knew why we were doing it and that it had to be done. Just from taking care of previous COVID patients, I knew what my mom was going through.”
So, like many of her patients’ family members, Perkins found a safe way to engage with her mom. Bundling up against the October snowstorm, Perkins headed to the window outside of her mom’s room.
“I called her on the phone, and we sat by the window and drank coffee and pretended the window wasn’t there,” Perkins remembered.
Over the next few days, these chats meant the world to Bachel. And the support continued to flow. Friends, family, and co-workers visited — even her daughter’s friends popped by to throw snowballs and wave an encouraging sign out of the window.
“It means more to the people in that hospital bed than you know,” Bachel said, choking up.
After four days of treatment, Bachel showed improvement, tested negative for the contagious antigen, and was released to recuperate at home for another week. She gradually started working again, building up her hours and strength slowly.
Today, Bachel feels “100% completely better.” When she looks back at the fall, she realizes just how ill she was.
“After about a month and a half of being so sick, when you do finally feel good, you realize just how terrible you felt,” she said. “I’m so glad I went in because I don’t know what would have happened. They took great care of me.”
Back at work, Bachel — already a compassionate person — feels even more empathy for patients and family members after her experience. She sees the same change in her co-workers who also recovered from the disease.
“I know how they feel,” Bachel said. “I feel it. It’s real. We all need to wear our mask and practice hygiene. It’s just here. It’s here all the time.”
Her daughter agrees.
“I just hope that people understand what these regulations are for and what the mask mandates mean for certain people,” Perkins said. “Until it becomes personal for you, you don’t really take it to heart. Until you realize one of these patients is a mother or a grandmother — because one was your mother — you just don’t realize the detrimental effects. I think all the people who make a stink about our mask mandates need to take a step back and realize it’s about being a good person.”

Local Journalist, Historian Touts Caring Medical Staff
Cardiology care at Sheridan Memorial Hospital is second to none according to local journalist Pat Blair.
Pat Blair has experienced more than her share of maladies, from suffering a heart attack to getting hit by a car. Luckily for the energetic 73-year-old Sheridan resident, she has had the expertise and support of the health care professionals at Sheridan Memorial Hospital (SMH) to see her through each incident.
How does she sum up her encounters with numerous hospital departments? One word: Caring.
“They’re just a terrific bunch of very caring people,” Blair said. “It really does feel like patient-centered care.”
One evening in January 2016, Blair started feeling pain shooting from the shoulder to the knuckles of her left arm. Imagining she had pulled a muscle, she drove herself to the hospital’s urgent care clinic the next morning.
“A nurse came in and said, ‘You’re having a heart attack,’” Blair remembered. “And my first reaction was, ‘I can’t be having a heart attack. I don’t have time for it.’”
She reluctantly called her team at Sheridan Media, where she has long been a tireless reporter, to let them know she wasn’t “going to be in that day, to say the least.”
Fortunately, the heart attack was minor. Blair’s cardiology team at SMH changed her medications and kindly provided her with information, resources, and support for eating well. She dedicated herself to following their advice and subsequently lost 40 pounds.
This was not Blair’s first foray into heart health. She failed her first stress test in the 1990s and was sent to a hospital in Billings for cardiac catheterization, or a heart cath, in which a thin, hollow tube is inserted into a large blood vessel to examine how well one’s heart is working, a procedure that was not yet available in Sheridan.
While discharging Blair, a nurse told her that the person she lived with should keep careful watch over her, as there were risks in the immediate recovery period. However, but for two dogs and a cat, Blair lived alone.
“The nurse said, ‘Well, just keep an eye on the site, and if you start bleeding, call the ambulance,’ and sent me home,” Blair recalled.
After her employer dropped her off at home, Blair spent an uncomfortable, sleepless night.
“I knew that if anything started happening, I was completely on my own,” she said.
This experience is in stark contrast to Blair’s heart cath at Sheridan Memorial Hospital 20-plus years later. After an inconclusive stress test in January 2020, she was offered the procedure, which has been available at SMH since the Heart Center and Cath Lab opened in 2013.
When SMH cardiologist Dr. Joseph Garcia learned that Blair lived alone, he suggested she stay at the hospital overnight after the procedure, so the on-call doctors and nurses would be able to monitor her in case of any issues.
“Totally different experience,” Blair said. “Everybody here was just very, very attentive, very caring. When I did have to get up in the middle of the night, like to go to the bathroom or something, there was always somebody there.
“I felt much more secure. It was just a greater comfort for me.”
Blair experienced another major incident in October 2019. After reporting on a Sheridan County Commission meeting at the courthouse, she stepped off of the curb by the activated pedestrian crossing button and was struck by a car.
The accident was disorienting.
“I kind of remember the impact, and I remember picking myself up off the street,” Blair said. “…And I remember kind of registering that I was bleeding.”
An ambulance took her to the hospital’s ER, where she was given seven staples on her head and examined for the significant bruising on her left hip and right knee. Testing showed no broken bones or concussion, fortunately.
A few weeks later, however, she awoke to searing pain in her left hip, where she was hit by the car. Back in the ER, Dr. Luke Goddard diagnosed bursitis. At his urging, Blair underwent several weeks of physical therapy.

Beyond the initial visit, each incident has included follow-up appointments and calls, further cementing Blair’s appreciation for her local hospital. From MRIs to ultrasounds, she has experienced a number of medical tests “that I could very happily have gone my entire life without having to deal with. But I’m really glad that if I had to deal with it, you know, this hospital was a good place. I felt very comfortable, very secure, very much taken care of and cared for.”
Today, Blair is feeling well. Her heart is checked every six months, and her injuries from the car have fully healed. For any incidents to come, she is comforted to know that Sheridan Memorial Hospital is steadfastly there for her, with the team’s high standard of care and culture of kindness.

Taylor Wendtland came to Wyoming Rehab after living with moderate to severe low back pain for nearly 10 years. The pain affected his ability to participate in many of the outdoor activities he enjoys. Since coming for treatment, Taylor’s pain has completely resolved, and he is back to doing all the things he loves. Here Taylor is playing Ultimate Frisbee in the park after just a few weeks of treatment at Wyoming Rehab. Congratulations Taylor!!
Call Wyoming Rehab today at 307.674.1632 and ask about our FREE Screens and Treatment Recommendations on Non-Emergent Physical Impairments/Injuries.

Denise Townsend: Fighting Forward

It was pure chance that Denise Townsend’s breast cancer was discovered early. She didn’t have any symptoms, her lump was not detectable through a physical exam and she had not been getting annual mammograms.
Cathy Wilson, a nurse practitioner at the Sheridan Health Center, was treating Denise for giardiasis, an infection in the small intestine.
“As part of my check-up, Cathy asked me when I last had a mammogram,” says Denise. “I told her it had been twelve years.”
Denise’s mammogram detected a suspicious looking mass; but it took an ultrasound test and a breast biopsy to confirm she had a tumor.
“When they ask you to come in to the office to discuss the results of your mammogram, you know that it is not going to be good news,” says Denise. “I was a bit in shock. All I could think was, oh no, it’s really cancer. Oh no, what am I going to do?”
“When I stopped into the Welch Cancer Center, I was amazed by the beautiful building; but the people inside were even more amazing,” says Denise. “I spoke with Kim, the receptionist and Nina Beach, the nurse practitioner. I explained that I had just been diagnosed with cancer and didn’t know what to do. Everything was happening so fast. Then, I began to cry.”
Denise was feeling completely overwhelmed and rightly so. She was told she had cancer on a Thursday and was scheduled for lumpectomy surgery the following Monday. Arrangements were made for Denise to meet with the hospital social worker right away. The two talked for a couple hours about her situation and the resources that were available. While Denise still couldn’t see light at the end of the tunnel, she was feeling somewhat better.
Once treatment started, Denise would go on to face other emotional challenges, like losing her hair, which reached down past her derriere.
“I had been thinking about a new hairdo before my diagnosis,” says Denise. “I just wasn’t planning on going bald!”
Denise’s cancer treatment included surgery, chemotherapy and radiation therapy. Along with treatment, she endured all of the emotional and physical characteristics that go along with it. At one point, she had to fight her way back to health from an inflamed pancreas. It caused her to be admitted to the ICU for a few days and came close to taking her life.
“Throughout my medical care at Sheridan Memorial Hospital, I was never treated like a number,” says Denise. “I am grateful for all of the assistance I was offered and compassionate care that I received from Dr. Greg Marino, Nina Beach and Dr. Shaun Gonda, plus all of the nurses and technicians.”
Another person who played a significant and very supportive role during Denise’s treatment was her daughter, Shara, who moved to Dayton just to help her mother out.
“My daughter is the number one reason that I emotionally survived this journey,” says Denise. “She helped me to stay positive and keep my sense of humor. She taught me how to network on the Internet, so that I could reach out to other cancer victims.”
Fortunately for Denise, her cancer was caught early, so her prognosis is good. Life is back on track for the most part. She has developed new friendships. She has renewed confidence and a stronger, more positive outlook.
“I’m still not certain of what the future has in store for me,” says Denise. “Though, I do know that I want to share my cancer journey in a way that helps others. I also want to encourage women to GET SCREENED! 1 in 8 women will be diagnosed with breast cancer in their lifetime. Those are not good odds. The ONLY way to survive cancer is through early detection.”
Denise goes on to say, “Cancer is scary; but you are NOT alone. There are so many resources out there that you can tap into. Don’t be afraid to reach out. It’s things like having cancer that help you discover what you are really made of. You also realize how many people there are out there that really do care. My motto is Fighting Forward, the rest I leave in God’s hands.”

Jennifer (Jen) Crouse considers herself somewhat of an authority on how healthcare should be delivered. During her 16-year healthcare career, she served in a number of professional capacities, including hospital administration. But a hospitalization in her youth, for a spinal cord injury, that she sustained in a car accident, is what ultimately set her on the path of wanting to help others.
“After being hospitalized for several months with my injury,” Jen recalls “I had good insight of what it was like to be a patient. I knew I wanted to be in a profession where I could assure patient care experiences were the best possible.”
As a hospital administrator, Jen paid close attention to patient care details. Other factors important to her included hospital smells, cleanliness and esthetic looks.
Last year when Jen required urgent medical attention, she naturally scrutinized the medical surroundings and care she received. Sheridan Memorial Hospital’s facilities, services, staff and physicians did not disappoint her.
Within a few weeks of moving to Sheridan, to take over as the new executive director of the Sheridan College Foundation, Jen developed a wound and became ill with a fever.
“So new to the community, I didn’t have a doctor. I didn’t know anything about the hospital or its services,” says Jen. When I called Big Horn Mountain Medicine and explained what was going on, staff got me in to see Autumn Barrett, PA-C immediately. It all happened so quickly and efficiently. I was told, ‘Don’t worry, we’ll take care of you.’”
For the next six weeks, Jen required outpatient services in Wound Care three times a week.
“Every interaction I had throughout my care was amazing,” says Jen. “Everyone was always so kind and friendly. From the moment I arrived in the parking lot, I was assisted. The staff handling the front desk greeted both my son and me by name. Savannah and the wound care team were exceptional. They took good care of me. They also provided me with the special supplies that I needed for home care. Despite the difficult circumstance, it was a great overall experience.”
Jen went on to say that the standard of care is higher here than what she would have imagined for a community this size.
“Compared to other hospitals I have worked in or visited, Sheridan Memorial Hospital is a great hospital,” says Jen. “It’s super impressive.”
Jen says her family’s move to Sheridan in and of itself was a big transition in their lives, without having to contend with additional worry.
“I haven’t required this level of patient care since my car accident,” says Jen. “It’s been over a year since I was treated and yet, I can still feel the emotional aspects of it if I think back. One thing certain, the care I received here was nothing short of a blessing.”


“9-1-1, What Is Your Emergency?”“I need help! I just found my husband face down on the floor! He is blue in the face and not breathing!” These were frantic words spoken by Nancy Naus, on Sunday, April 19, 2015, after she investigated strange sounds coming from the room where her husband, 68 year old Michael Naus, had been working on his computer. When she discovered him lying on the floor, blue in the face and bleeding from the fall, she immediately grabbed her cell phone and dialed 9-1-1.
Though Nancy had never trained in cardio-pulmonary resuscitation (CPR), common sense told her that she had to initiate some form of CPR if Michael were to have any chance of surviving. Nancy began administering a ratio of 30 chest compressions to two breaths on Michael. She also cried out for her mother, who was living in the family home, to take over the 9-1-1 call. Nancy continued CPR until Emergency Medical Services (EMS) personnel arrived on scene.
Controlled frenzy ensued. Within minutes, the EMS crew took over CPR and attached pads to Michael’s chest to analyze his heart rhythm. At two different intervals, paramedics delivered electrical shocks to correct Michael’s abnormal heart rhythm using an automated external defibrillator (AED). Since Michael wasn’t breathing on his own, they inserted a tube to open his airway and improve their ability to manually deliver breaths. CPR continued as the ambulance raced to the hospital, sirens blaring.
Communication between paramedics and Sheridan Memorial Hospital’s Emergency Department readied William Selde, MD and the nursing team for Michael’s arrival. Dr. Selde quickly assessed Michael’s condition. After confirming a pulse and spontaneous circulation, Dr. Selde’s next course of action was to stabilize Michael’s blood pressure and start him on a ventilator to pump more oxygen-rich air into Michael’s lungs. He then ordered an electrocardiogram (EKG) to get a reading on Michael’s heart.
The EKG confirmed Dr. Selde’s suspicions; Michael had suffered a massive heart attack. At that point, cardiologist Joseph Garcia, MD and internal medicine physician David Walker, DO were called to intervene in Michael’s care.
As the clock ticked on, Michael’s life continued to dangle by a thread and Nancy and her family were left keeping a constant vigil of prayers. Nancy was overwhelmed with grief as Michael was given no better than a 20% chance of surviving.
“I prayed to God that He give Michael back to me as he was or take him,” she remarked.
While the heart catheterization team prepped Michael for a coronary intervention procedure, Dr. Walker and Dr. Garcia hastily worked side by side.
Dr. Walker made sure that Michael was adequately oxygenated, a task made more serious and challenging by the broken ribs Michael had sustained during CPR. (Broken ribs are a common consequence of CPR.) He then used a paralyzing medication to keep Michael sedated and motionless during the heart procedure.
Michael’s body temperature was also being deliberately cooled to a hypothermic state using ice packs. (Induced therapeutic hypothermia is necessary in certain cases of cardiac arrest because cooling the body’s temperature for several hours reduces the risk of brain cell damage and tissue injury.)
During the heart procedure, Dr. Garcia used a balloon catheter to inflate the blocked arteries of Michael’s heart and insert stents (tubes that are inserted into the blood vessels to keep them open). Again, Michael’s broken rib cage complicated the procedure and increased the risk involved. Once Dr. Garcia had restored the blood flow to Michael’s heart, he inserted an intra-aortic balloon pump, which is a mechanical device used to assist the heart in pumping blood, to further stabilize him. Still, Michael’s life remained in perilous condition. He was not out of the woods by any means.
If Michael survived, he would definitely need prolonged care on a ventilator and it was still uncertain whether he had suffered any brain damage due to the oxygenation complications of CPR. With those two things in mind, doctors began making arrangements for Michael to be transferred by air ambulance to the Billings Clinic. Nancy followed along, making the journey to Billings by car.
After arriving at the Billings Clinic, doctors there explained the increased odds of Michael having another heart attack and speculated about the possibility of him having lasting neurological side effects. Nancy was encouraged to consider signing a “Do Not Resuscitate” (DNR) order, in case Michael’s heart stopped beating again.
“That was absolutely horrible for me,” Nancy described. Too emotional to make the difficult decision on her own, she sought the advice of her three grown sons and closest friends. It was with a feeling of unsettled reluctance that she ultimately signed the DNR order. Deep down in her heart, Nancy firmly believed she would have the miracle she and her Christian support group were praying for.
As minutes turned into hours and hours turned into days, the odds and hope that Michael would survive gradually grew.
Michael spent the next three weeks hospitalized in the Billings Clinic. Ten of those days were spent in the intensive care unit (ICU). After he regained consciousness, doctors determined that Michael had not suffered any loss of brain function. Nancy’s prayers had been answered.
The recovery process was slow. On top of his hospitalization, Michael was moved to St. Vincent’s New Hope Rehabilitation Center for nine days. Intensive physical therapy treatment was necessary to regain his strength after being bed-ridden for so long.
“The first memories I have of this entire ordeal began during my stay at New Hope,” recalled Michael. However, that might not be all bad considering what he had been through.
Michael returned to Sheridan but that was not the end of his need for medical care. Rehabilitation continued with Sheridan Physical Therapy for another six weeks. Two weeks into physical therapy treatments he was also enrolled in the Cardiac Rehab program at Sheridan Memorial Hospital.
As of late, Nancy and Michael have resumed their prior routine of walking daily. “I am blessed to be alive,” Michael acknowledges.
Looking back, Nancy and Michael admit that signs of a heart attack were present a few weeks before his event. Michael had complained of tightness in his chest, but they attributed it to the vitamins he was taking and ruled out the possibility of it being heart related.
“Also playing a role was that age-old mind set of thinking long and hard before going to the doctor. The high cost of health care and insurance deductibles also make you think twice,” Nancy said. “The lesson we learned has been a painful one,” she added.
“My advice: if you have chest pain get to the emergency department and get it checked out right away!” Michael recommended.
Michael’s survival is nothing short of a miracle. The three Sheridan Memorial Hospital physicians involved in Michael’s care will humbly give Nancy credit for saving Michael’s life. Had Nancy not started CPR, Michael absolutely would have died. (According to the American Heart Association, nearly 400,000 out-of-hospital cardiac arrests occur annually in the United States. Performing Hands-Only CPR can double or even triple a victim’s chance of survival.)
But Michael’s survival also depended on the quick action of local, highly skilled volunteer and paid EMS crews, expertly trained physicians and nurses, and Sheridan Memorial Hospital having the most advanced systems and technical capabilities available.
“The overall medical response to the circumstances surrounding Michael’s case was nothing less than textbook perfect from start to finish,” said Dr. Garcia. “The level of medical personnel and services we have available in a community this size are truly amazing.”
“Michael’s incident serves as an important reminder to the community about the critical value of recognizing and acting on the signs and symptoms of a heart attack and learning CPR,” affirmed Dr. Walker.
Nancy and Michael Naus want to acknowledge and thank everyone involved in Michael’s care. Michael’s medical journey crossed paths with the following entities:
- 9-1-1 Dispatch
- Rocky Mountain Ambulance
- Goose Valley Volunteer Fire & Rescue
- Sheridan County Fire & Rescue
- Sheridan Memorial Hospital:
- Emergency Department
- Cath Lab
- ICU
- Cardiac Rehab
- Guardian Air Ambulance
- Billings Clinic
- St Vincent Healthcare New Hope Rehabilitation Center
- Sheridan Physical Therapy

If anyone can compare cancer services in Sheridan, Wyoming years ago to what is available today, it is Geraldine and Larry Roberts. Geraldine had three occurrences of cancer in her right breast in a span of 15 years. The first diagnosis resulted in chemotherapy and radiation treatment, the second involved a mastectomy and this last time consisted of another round of chemotherapy and radiation.
When they talk about their journey, Larry and Geraldine agree, “We both had cancer.” Geraldine may have been the one diagnosed with breast cancer, but cancer definitely affected both of their lives. So, they tackled Geraldine’s cancer in the same manner they did in 35 years of marriage – as partners.
Geraldine’s job as the patient was to get better, while Larry filled the role of caretaker. Larry worked full time and took care of the housekeeping, cooking, laundry and yard. He helped manage Geraldine’s care by accompanying her to all of her clinic and treatment appointments and keeping a careful account of the treatment details, blood pressure, weight and medications.
“To accomplish the additional work load you have to set priorities, do only those things that are truly important,” Larry said. “The extra work is easy when you love the person you are caring for.”
The caretaker needs to take care of himself, by eating right and getting sufficient rest,” reminded Geraldine. This is something too often neglected. “Yes dear,” Larry surrendered.
During the first bout of cancer, Geraldine had not mentally prepared to be so sick with nausea. Nothing tasted good. “Milk even tasted sour!” Geraldine proclaimed. “Larry tried every food imaginable, including ice cream! The only thing I somewhat enjoyed was fried potatoes. So we ate fried potatoes for six months,” she grinned. When this last cancer was discovered, Geraldine was pleasantly surprised to learn there are now special drugs available to help with nausea. It made her treatment much more bearable.
Out of love, Larry is the one who shaved Geraldine’s head both times radiation and chemotherapy caused her hair to begin falling out in clumps. “It’s best just to get it over with,” says Geraldine. “But, the first time he shaved my head, I cried when I looked in the mirror. I hadn’t known what to expect. It was such a shock. There weren’t wigs available back then like there are today. I didn’t want to go out in public until a neighbor was nice enough to make me a bonnet to wear.” The second time Larry shaved Geraldine’s head she had an assortment of wigs and hats to choose from, including a Harley Davidson do-rag that Larry surprised her with!
When you lose a breast, you feel like you are no longer a whole person. You don’t want to undress in front of your husband. In fact, the first time I looked at myself in the mirror, after the mastectomy, I just screamed.” At the time, Larry went immediately to Geraldine’s side, “I reminded her that I didn’t marry a boob!” Geraldine quipped back, “But, I did!” They both laughed. In reality though, Larry’s reaction made all the difference in the world to Geraldine and getting a fitted bra and breast prosthesis made her feel even better.
“Learning to cope with cancer is a real challenge, it changes how you perceive life,” explained Geraldine. “Life becomes all the more precious when it is at risk. It teaches you to realize what is truly important and to let go of what isn’t. You come to fully appreciate each new day and the happiness it can bring.”
Geraldine’s advice is to “take one day at a time but also identify something you will have to look forward to in the future – after treatment is over. Above all, if you need help, ask for help. Don’t suffer in silence.”
Having her cancer care anywhere but Sheridan Memorial Hospital’s Welch Cancer Center was never a thought for consideration. Geraldine remarked, “I have great faith in our hospital system. I had received good care here in the past and all of the services I needed were available right here. There was no need to look elsewhere.”
Geraldine now marvels at the changes that have taken place throughout her entire cancer journey, from the first cancer treatment she received in a house (the Partridge House) in 2000 compared to her second treatment course which took place at the Welch Cancer Center this past year. “The differences are dramatic,” observes Geraldine. She is in awe of the new facility and the new equipment, and extremely impressed by the exceptionally trained and compassionate nursing staff. She appreciates the way Dr. Fehir and Dr. Marino put her at ease with their personalized care and compassion.
“The one thing that hasn’t changed over the years is how special the staff is,” Geraldine says warmly. “They treat you the same way you would expect to be treated by your family.”