With October often comes the colors changing not only on the grass and trees, but pink is often around every corner you turn. This year marks the 14th Annual Link Partners in Pink for the Sheridan Memorial Hospital Foundation and our community. It was a hugely successful event with hundreds of participants, volunteers and cancer survivors in attendance. This year’s funds raised will go toward the Comfort Care Program at Sheridan Memorial Hospital’s Welch Cancer Center (WCC). These funds are available to cancer patients of all cancer types and providing them with the most comfortable experience during their cancer journey. But what exactly is comfort care and how does it provide needed resources to your neighbors, patients, and family?
Sheridan Memorial Hospital’s Welch Cancer Center Comfort Care Program began with a few gifts to support the journey of cancer patients through their diagnosis and treatment. Now, through thoughtful and generous donations and memorials, Comfort Care provides this needed funding based on criteria set and the patient’s financial needs. These one-time grants enable the WCC team to help our patients and their families on a personal level. Grants may also be used to help with travel expenses associated with unexpected treatments or to aid patients in the region to travel to Sheridan for their necessary treatments. Our patients and staff are grateful for the funds as they cover numerous other resources, support programs, and other comfort-related items, including individual counseling.
Throughout the last year, these funds have provided:
- 20 Wigs, Caps, & Hats for patients on their journey through cancer treatment
- 114 bras & camis were provided for women undergoing mastectomy, lumpectomy or reconstructive surgery, each fitted by a specially trained RN for their individual and specific needs.
- 5 hotel stays have been provided to patients and their families to ensure their safety during winter months, housing for longer periods of treatment, and a home away from home while receiving care at the WCC.
- 76 bus rides have been paid for so our patients don’t have to worry about the logistics or cost of travel before and after their treatments.
- 12 gas cards were given to patients and their families for emergency travel when unexpected trips arose for patients with escalated health care needs at other hospital locations.
It is a gift to be able to support this pivotal part of care and healing for some of the most vulnerable patients in our community.
For more information about the WCC’s Patient Comfort Care please contact the Welch Cancer Center at 307.674.6022.
To make a donation to the WCC Patient Comfort Care Program or other vital healthcare programs, please call The Foundation at 307.673.2418.
































 Sheridan Memorial Hospital’s Audiology team is gearing up for National Audiology Awareness Month this October. This campaign was created to raise awareness of audiology and the importance of hearing protection in preventing noise-induced hearing loss. Noise-induced hearing loss (NIHL) affects many Americans. An estimated 12.5% of children and adolescents aged 6–19 years and 17% of adults aged 20–69 years have permanent damage to their hearing from excessive noise exposure.
Sheridan Memorial Hospital’s Audiology team is gearing up for National Audiology Awareness Month this October. This campaign was created to raise awareness of audiology and the importance of hearing protection in preventing noise-induced hearing loss. Noise-induced hearing loss (NIHL) affects many Americans. An estimated 12.5% of children and adolescents aged 6–19 years and 17% of adults aged 20–69 years have permanent damage to their hearing from excessive noise exposure.












 Dr. Hannah Hall, Dr. Juli Ackerman, Dr. Sierra Gross, Dr. David Walker, Erin Strahan PA-C, and Jason Otto PA-C will remain with SMH Internal Medicine and continue to see patients in their current location in the Outpatient Center.
Dr. Hannah Hall, Dr. Juli Ackerman, Dr. Sierra Gross, Dr. David Walker, Erin Strahan PA-C, and Jason Otto PA-C will remain with SMH Internal Medicine and continue to see patients in their current location in the Outpatient Center.

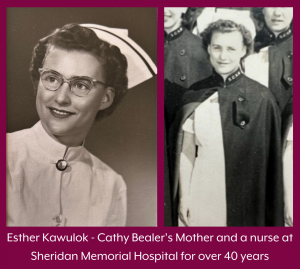 For those of you who might remember Cathy’s mother, Esther Kawulok, she graduated from nursing school in Montana in the early 1950s. Esther was the first and only child in her family to earn a college degree and she did so because she didn’t want her children to struggle as she had: growing up in a two-room home with a dirt floor. After graduating, Esther and two other single nurses moved to Sheridan to work at the hospital. Cathy’s mom married her dad and the couple worked tirelessly to raise Cathy and her 5 siblings. Esther worked for over 40 years at Sheridan Memorial Hospital while her dad worked two jobs. Her parents’ strong work ethic and compassion for others have been driving forces in Cathy’s life.
For those of you who might remember Cathy’s mother, Esther Kawulok, she graduated from nursing school in Montana in the early 1950s. Esther was the first and only child in her family to earn a college degree and she did so because she didn’t want her children to struggle as she had: growing up in a two-room home with a dirt floor. After graduating, Esther and two other single nurses moved to Sheridan to work at the hospital. Cathy’s mom married her dad and the couple worked tirelessly to raise Cathy and her 5 siblings. Esther worked for over 40 years at Sheridan Memorial Hospital while her dad worked two jobs. Her parents’ strong work ethic and compassion for others have been driving forces in Cathy’s life.