Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
SMH Friendly Faces
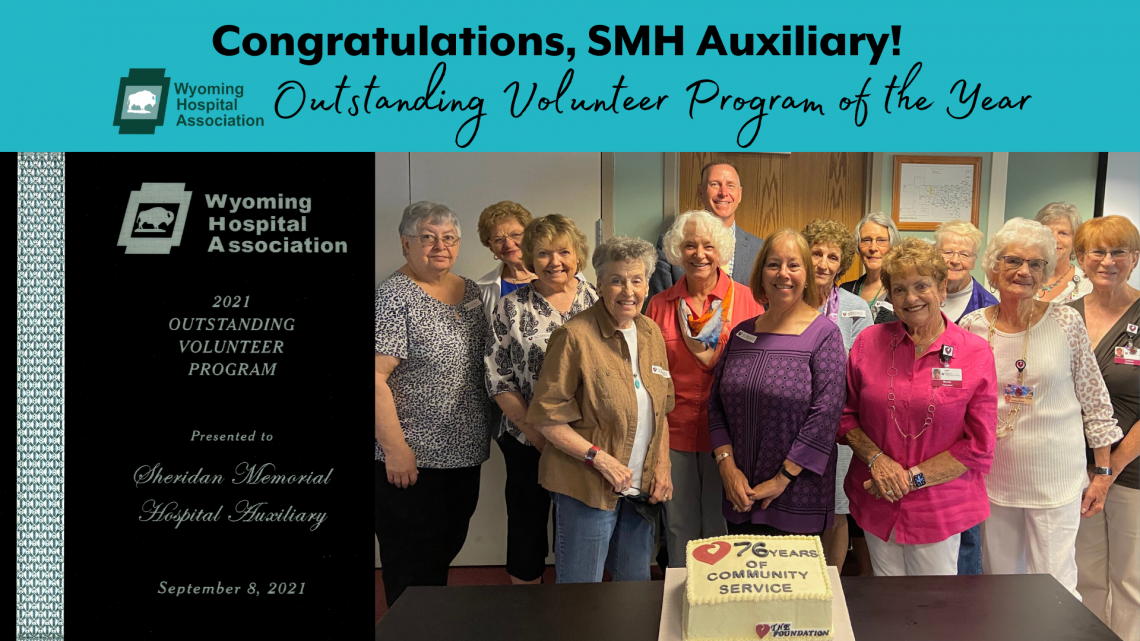
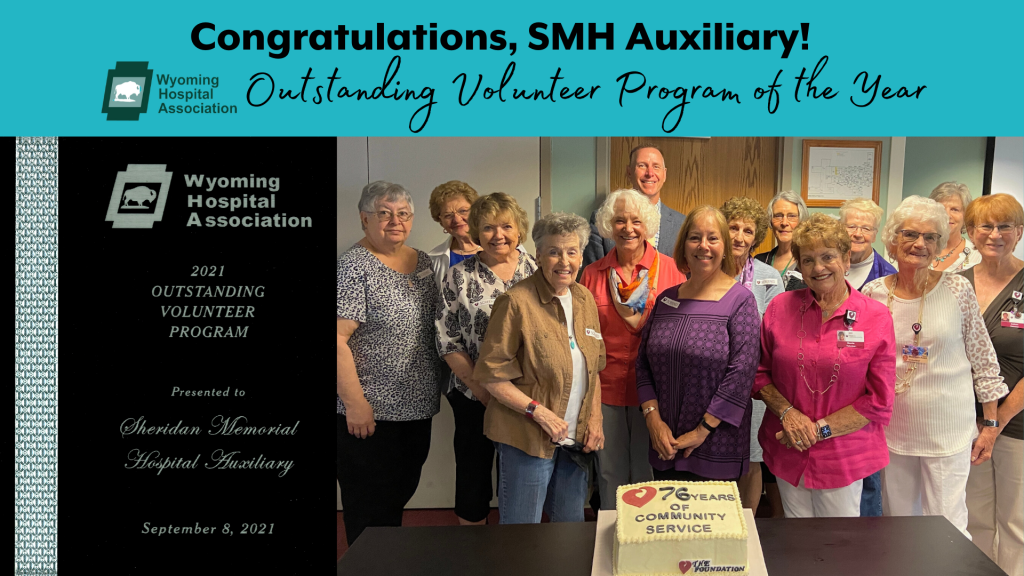
Many times we’re asked who The Sheridan Memorial Hospital Auxiliary is? Below you’re going to read countless things they accomplish year after year to support your community hospital. They are one of twenty-seven Auxiliaries and numerous hospital volunteer organizations in the state of Wyoming. However, this unique group of individuals comes together, day after day, to support our mission, the staff, patients, and the community that we live in. They ensure that the traditions of our hospital live on through Trees of Love and 5-year-old Birthday parties. They presently gift patients of all ages with baby books, scrubby bears, or Gifts of Kindness during the holidays to provide comfort during their stay. They raise funds through all their projects and donate tens of thousands of dollars and volunteer hours to ensure a future for your community hospital. For these reasons and all those listed below in their nomination letter, The Sheridan Memorial Hospital Auxilary has been named The Wyoming Hospital Association’s Outstanding Volunteer Program of The Year for 2021.
Dear Selection Committee:
I am writing to nominate the Sheridan Memorial Hospital Auxiliary for the Wyoming Hospital Association’s Volunteer Program of the Year. During 2020, there were no celebrations to recognize the Auxiliary members for their 75th year of support, but they continued to do what they do best: fulfill their mission “to provide comfort to and better the welfare of Sheridan Memorial Hospital’s patients.”
The SMH Auxiliary was founded in 1945 and since then has supported nearly every department and project at the hospital. Just before COVID broke out in early 2020, the Auxiliary announced a gift of $37,000 to enhance patient care in several departments including Respiratory Therapy, Urgent Care and Family Waiting Rooms. Although, COVID restrictions meant closing down the Auxiliary gift shop, waiting room volunteering and other annual events, the Auxiliary and other hospital volunteers kicked into full support mode and changed things up with new ideas to continue their mission. Auxiliary members made masks and gowns. They volunteered to iron the nearly 10,000 donated, hand-made masks after they were laundered. Annual events turned from in-person events to fun filled drive by celebrations and socially distanced spirit-lifters. At the end of the summer, their tradition of celebrating all five year old birthdays in our community was a huge success, with over 150 cars driving by to watch their favorite animated characters (Auxiliary members in full costume) hand out activity bags. And during the holiday season, the Auxiliary helped bring comfort and joy to our community by hosting a socially distanced Trees of Love ceremony, lighting the trees out in front of the hospital.
Over one of their monthly Zoom meetings in February, the Auxiliary once again stepped up to help the hospital with a pledge of $50,000 for the Transitional Care Expansion Campaign. This generous gift kicked off the community fund drive that successfully raised $4.4 million in just over 10 months. With this gift, the Auxiliary has given $724,000 to Sheridan Memorial Hospital over the last 20 years.
Last month, the SMH Auxiliary Board hosted a welcome back lunch and celebrated 76 years of community service with cake and special visit from Mike McCafferty, CEO of SMH. We are so happy to have them back on campus. Volunteers of the Auxiliary are once again working in our hospital’s Kozy Korner gift shop and recently returned to the Hospital’s Outpatient Waiting Area to help and assist our patient families and caregivers
I am so proud to have the opportunity to work with this incredibly dedicated group of SMH supporters. Our hospital would not be what it is today without their support. I highly recommend the Sheridan Memorial Hospital Auxiliary and all of our dedicated volunteers for the Wyoming Hospital Association’s Volunteer Program of the Year.
Sincerely,
Cody S. Sinclair
Chief Development Officer
To learn more about The Auxiliary contact our Volunteer and Development Coordinator – Jasmine Slater at 307.675.2620 or visit https://www.sheridanhospital.org/community/volunteer-opportunities/.

By Charlotte Walter, PT, DPT, ATC – Physical Therapist at Sheridan Memorial Hospital’s Wyoming Rehab
Falls Prevention Awareness Day is coming on September 22, and I’d like to take this opportunity to remind folks why falls prevention is so important. According to the Centers for Disease Control and Prevention (CDC), more than one out of four older adults – those 65 and older – fall each year. These falls are serious and costly, causing broken bones or head injury. In fact, falls are the most common cause of traumatic brain injuries. Falls can lead to reduced mobility, decreased independence, and an increased fear of falling, all of which profoundly affect an individual’s quality of life. However, less than half of people who do fall tell their doctor.
Falls are not a normal part of aging and can be prevented. Four key steps to falls prevention include speaking to your doctor, staying active, getting your eyes checked and making your home safer.
As mentioned above, many people who fall do not tell their doctor. However, your physician plays a crucial role in keeping you safe. They can evaluate your risk for falling, review your medications to see if any may cause dizziness or drowsiness, and offer suggestions for vitamin D supplementation, seeing a physical therapist, or seeing a podiatrist if needed. Another concern to bring up to your doctor is how frequently you get up at night to use the bathroom. Research shows that individuals that get up more than 2-3 times per night have a significantly higher risk of falling. Your doctor may suggest medications or pelvic floor physical therapy to help address this.
Simply staying active can play a major role in fall prevention. Older adults should engage in regular, intentional physical activity that builds balance, strength, and flexibility. Unfortunately, the COVID-19 pandemic put most in-person exercise classes on hold, but many offerings through the Hub on Smith and the YMCA have returned. Online exercise class options via Zoom are also being offered. Contact these organizations for more information on current class schedules. Keep in mind that physical activity does not have to happen inside a gym. Strength training can be performed using objects around the home. Clear some space and dance to your favorite music to get your heart rate up. Exercise videos can be found on YouTube. Sheridan residents are fortunate to have an abundance of trails and parks available for walking, bicycling and hiking. Gardening and yard work are also forms of physical activity that don’t require exercise equipment. In short: sit less, move more.
If health conditions or physical limitations are preventing you from being physically active, ask your doctor about physical therapy. Physical therapists are highly trained health care professionals with expertise in movement and exercise. Physical therapy is not just for after a surgery or injury, but also an excellent way to prevent injury, falls or deconditioning. A physical therapist can evaluate your strength, balance and endurance and create an individualized plan to help meet your goals for physical activity. Not sure of where to start? Wyoming Rehab provides a free screening for individuals looking for treatment recommendations that do not require a physician referral. Don’t let a small barrier become a wall that continues to limit your physical activity.
When was the last time you had your eyes checked? Quality of vision is important to provide your brain with accurate information about your position in space. Conditions like cataracts and glaucoma limit your vision. If your eyeglass prescription is outdated or no longer appropriate, that can negatively affect your balance ability. The current recommendation is to have your eyes checked by an eye doctor at least once a year.
Another way to prevent falls is to make your home safer. Take a look around and ask yourself the following questions: Are there papers, shoes, books, or other objects on the stairs? Is a stairway light bulb burnt out? Are there handrails on both sides of the stairs? Are there throw rugs on the floor? When you walk through a room, do you have to walk around furniture? Is your step-stool sturdy? Is the light near the bed hard to reach? Is there a clear path from the bedroom to the bathroom? Is the tub or shower floor slippery? Do you need support when getting off the toilet or out of the shower? It’s time to consider these and other obstacles that can intensify someone’s fall risk in their own home.
Some easy tweaks can make a big difference. Want to learn more? Some excellent online resources include the CDC, National Council on Aging and National Institute on Aging websites. Here, you can find articles, action plans, infographics, exercise suggestions, exercise videos and more information on staying active and preventing falls.
Here in Sheridan, we are lucky to have many resources available to older adults, both in-person and online. Take the steps to keep yourself safe, active, and healthy this fall!
Do you have a condition or impairment preventing you from reaching the recommended amounts of physical activity? Don’t continue to put your health at risk. Find out how physical or occupational therapy may help. Reach out to Wyoming Rehab at 307.674.1632 if you would like to schedule a FREE Screen/Treatment Recommendation for a Non-Emergent Physical Impairment or Injury.
Learn More about Wyoming Rehab and their free screenings for non-emergent physicial impairments or injuries by clicking HERE or following the link https://www.sheridanhospital.org/medical-services/rehabilitation-services/
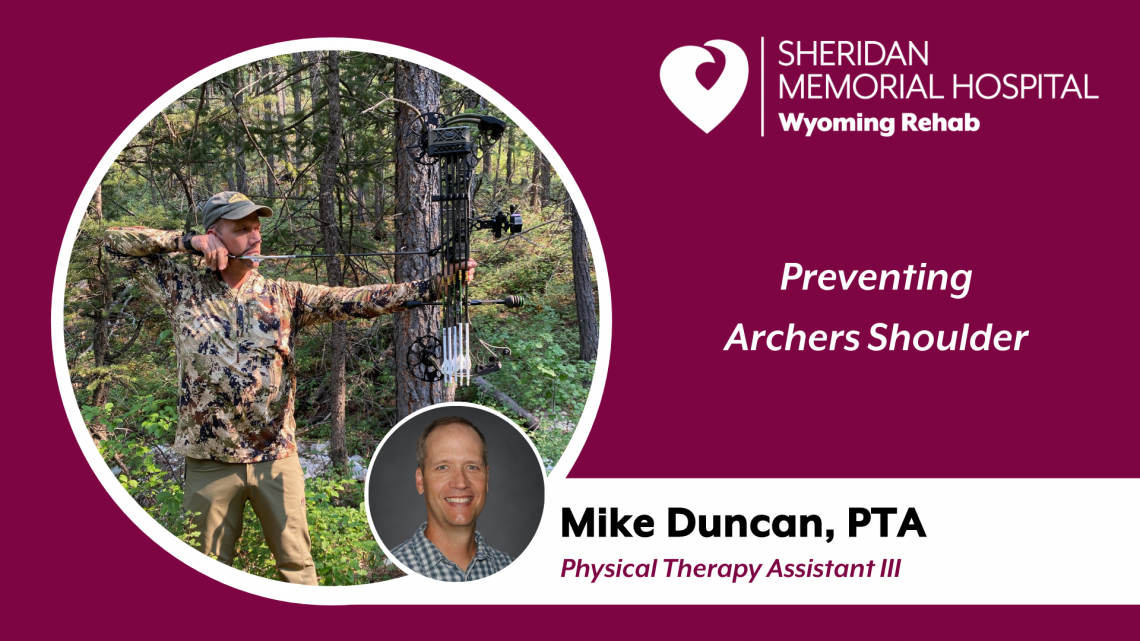
By Mike Duncan, Physical Therapy Assistant III at Sheridan Memorial Hospital’s Wyoming Rehab
The fall season is rapidly approaching and for many Wyoming residents, that means hunting season. Hunting with archery equipment or bow hunting thrills many Wyoming hunters.
Archery is truly an amazing sport. Saxton Pope summarized it perfectly when he said this, “Here we have a weapon of beauty and romance. He who shoots with a bow, puts his life’s energy into it. The force behind the flying shaft must be placed there by the archer. At the moment of greatest strain he must draw every sinew to the utmost; his hand must be steady; his nerves under absolute control; his eye keen and clear. In the hunt he pits his well-trained skill against the instinctive cunning of his quarry. By the most adroit cleverness, he must approach within striking distance, and when he speeds his low whispering shaft and strikes his game, he has won by the strength of arm and nerve. It is a noble sport.”
If you think about the basic actions of shooting a bow – pull back with the fingers or wrist and arm, rotate through the shoulder, hold, and release – it probably becomes clear why upper extremity conditions are some of the most commonly diagnosed injuries among bow hunters. The drawing back of the strings demands a lot from the smaller muscles of the rotator cuff, forearm, wrist, and fingers. Plus, repetitive target practice to improve aim, timing, and other hunting skills can easily result in chronic pain or injury from overuse, referred to as Archers shoulder.
Injuries to the rotator cuff are archery’s most common problem. The rotator cuff is a complex system of muscles and tendons in your upper arm that is used to draw a bow and to raise and rotate your arm. Rotator cuff injuries include tendinitis, bursitis, and, in severe cases, a rotator cuff tear. Tendonitis is a condition that results from the rotator cuff tendons becoming irritated or damaged. Bursitis involves the fluid-filled “pillow” that acts as a cushion between the rotator cuff tendon and shoulder blade, which may become irritated or inflamed. A torn rotator cuff tear may put you out for the season but is not always easy to diagnose. Symptoms include having trouble lifting, raising your arm, pain when moving, shoulder weakness, or a clicking sound in your shoulder when moving it. If you have any of these symptoms, stop shooting and seek competent medical advice. Through skilled rehabilitation, most archers recover and resume shooting upon completing physical therapy.
Specific exercises and stretches from a qualified professional at Wyoming Rehab will alleviate and can prevent the common conditions associated with Archers shoulder and return you to the range or to the hunt. Call us today to set up a free screening for non-emergent physical impairments or injuries – 307.674.1632.
Learn more about Wyoming Rehab services by following the link sheridanhospital.org/medical-services/rehabilitation-services/
The Sheridan Memorial Hospital Foundation Staff and Board of Directors are pleased to welcome Sue Belish, the newest Foundation Board Director.
During the Foundation’s Annual Meeting, held this past July, the current board unanimously voted to induct Sue into the Foundation board of directors. Additionally, the following Board members were elected as this year’s Foundation officers: President-Richard Garber, Vice President-Rob Johnson, Secretary-Vicki Jorgenson, and Treasurer-Matt Ebzery. Joe Wright will also return back to The Foundation Board, but in a new role, as the Hospital Board of Trustee Representative.
“Sue has dedicated so much of her life and energy into caring for others and improving our community. We are excited to have her join The Foundation Board of Directors,” said Chief Development Officer Cody Sinclair. “Sue will help us meet The Foundation’s mission to cultivate community involvement and support the hospital’s vision: When people think of excellent healthcare, they think of Sheridan.”
Sue likes to spend much of her free time landscaping around her home and reading when she’s not too busy remodeling her kitchen and visiting with her grandchildren as often as possible. Beyond her recent induction into The Foundation, Belish currently serves on the Chandler H. Kibbee and Mercedes K. Kibbee Foundation Board and works for the Wyoming School Boards Association in leadership development. She has also served in the past on the Wyoming State Board of Education, on the Center for a Vital Community Board, on the Tongue River Valley Community Center Board, on the Big Horn Education Fund Board, as an interim administrator for Northern Wyoming Community College District, as the principal for Tongue River Middle School, and as the superintendent of Sheridan County School District #1. Sue shared, “My reason for joining the Foundation is not because I have always had a deep passion for healthcare per say, but because I have an interest in giving back to this community. The many relationships I have formed here have been integral to my own personal success in life and I see serving on the Foundation as an opportunity to give back to that community which has given me so much.”
With all the challenging work ahead of The Foundation, Sue’s leadership, knowledge, and community spirit is a welcome addition to The Foundation Board. The Foundation looks forward to the experience, passion, and perspective Sue will bring in the coming year and all we will accomplish for healthcare in our community – together.
To learn more about The Foundation and its Board of Directors, visit sheridanhospital.org/foundation or call The Foundation Offices at 307.673.2418.

By Pattie Visscher, Au.D., Audiologist
I’m excited to join the hospital staff as the new audiologist at Sheridan Memorial Hospital’s Ear, Nose and Throat (ENT) clinic. As an audiologist, I am a healthcare professional who can help prevent, diagnose and treat hearing and balance disorders in people of all ages. Audiologists help people improve their communication with others around them by offering those with listening difficulties increased access to auditory information via amplification options as well as communication and listening strategies.

I have been practicing audiology for more than 25 years, with an emphasis on pediatric care. I began my professional career at the Colorado School for the Deaf and the Blind in Colorado Springs. That experience gave me knowledge of Deaf culture, many types of amplification (traditional hearing aids, bone-anchored hearing aids, and cochlear implants), as well as the opportunity to become fluent in American Sign Language (ASL). My husband and I moved to Sheridan this summer and are so happy to be here.
I look forward to offering the Sheridan community comprehensive audiologic care. At our office, the focus for audiology is diagnostic testing, both to support Dr. Cheryl Varner, our otolaryngologist, and to work with patients directly to monitor hearing status and investigate the need for amplification, possibly with hearing aids. Our diagnostic services include complete hearing evaluations and a variety of testing techniques that specifically determine the status of the middle ear, inner ear and the auditory neural pathways.
Individuals with hearing loss commonly report feeling they misunderstand others or miss out on important conversations around them. They have trouble understanding others when in noisy environments such as restaurants. They have difficulty following dialogue on television programs, and many experience a ringing sound in one or both ears. Some people report a feeling of pressure or fullness in their ears and many report concerns with balance. Sometimes people suffer from dizziness or vertigo. Knowing and understanding your hearing status gives you the information you need to make informed decisions regarding your hearing.
Dr. Carol Flexer is a well-known professional in the field of audiology. She is famous for saying, “we hear with our brains,” calling our ears the “doorway” for sound to get to the brain. She emphasizes the sensory importance of the ears to deliver information to our brains so we can understand and organize auditory information. Good hearing is so important during childhood development in order for a child to hear and understand and know the difference between mom saying, “good morning” or “no, no, that’s hot, don’t touch.” Good hearing remains important throughout the lifespan. Much research has been devoted to examining the connection between cognitive decline and impaired hearing. Remaining engaged in communication keeps your brain active. Hearing impairment can lead to withdrawal from social interactions and decreased communicative interactions.
In today’s world, dealing with hearing loss while attempting to communicate with someone wearing a face covering or mask can be especially difficult. Many individuals wearing hearing aids have reported difficulty removing a mask without a hearing aid flying across the room. Shortly after mask mandates began, hearing aid manufacturers saw a spike in claims for hearing aid replacements or repairs due to loss or damage associated with wearing a mask and hearing aids. There are face covering styles that may work better for individuals with hearing aids, including masks that tie behind the head. Another option is the use of mask extenders that may reduce fatigue from pressure on your ears and redirect the mask ear loops.
YouTube has videos with suggestions regarding Face Masks and Hearing aids:
https://www.youtube.com/watch?v=wuPZAjhT_cQ
https://www.youtube.com/watch?v=FLP5CwiZn3I
Here are some hearing-related statistics from the NIDCD (National Institute on Deafness and Other Communication Disorders) that demonstrate how prevalent hearing concerns are in the United States:
- Approximately 15% of American adults (37.5 million) aged 18 and over report some trouble hearing.
- Roughly 10% of the U.S. adult population, or about 25 million Americans, has experienced tinnitus lasting at least five minutes in the past year.
- Five out of 6 children experience an ear infection (otitis media) by the time they are 3 years old.
In the near future, the hospital’s ENT will offer hearing aid services, including consultation, sales, fitting and follow-up. We plan to offer hearing aids from major manufacturers, including Phonak, Oticon, Resound and Starkey. Selection and fitting of custom earmolds for hearing protection will also be offered. Audiology’s future goals include offering aural rehabilitation services, where a plan is developed to help target a hearing impaired individual’s specific listening and communication needs. This may also include aural rehabilitation group activities. I am also particularly interested in using my previous experience to partner with our local pediatric professionals.
If you are experiencing listening difficulties or suspect you have hearing loss, there are options to help you manage these issues. Your first step should be to ask your primary care provider if they feel you should see an Audiologist. A referral to our office is not necessary, but before making an appointment without a referral, you should check with your insurance company to see what is required.
To make an appointment, call 307.675.4646.
Resources you can check out for more information about Audiology are:
https://www.asha.org/public/hearing/
https://www.nidcd.nih.gov/health/hearing-ear-infections-deafness
To learn more about our Ear, Nose & Throat Clinc here at Sheridan Memorial Hospital and our new Audiology services, click HERE or visit sheridanhospital.org/medical-services/clinics/ear-nose-throat

Holly Zajic (pronounced Zeitz) loves helping people be the best they can be every day. When you first meet her, it’s the exuberance and energy she conveys that you notice first. Zajic is the new Chief Ambulatory Officer for Sheridan Memorial Hospital (SMH) and is excited about her new role and new home.
But you may be asking yourself, ‘What is a Chief Ambulatory Officer?’ Zajic acknowledges that ambulatory is a new term that can be used interchangeably to describe outpatient healthcare services.
“I have been asked that question numerous times,” Zajic explains, “And my goal is to partner with our ambulatory (outpatient) teams to advance the care model for our patients and ensure that we continue to provide excellent, safe, timely and reliable care. I truly believe the future of healthcare is in ambulatory services and driving value for our patients through these services is essential to the health of our community.”
Mike McCafferty, SMH Chief Executive Officer, had this to say when addressing employees at a recent forum for all SMH employees, “The goals we have in front of us as a healthcare system will require exceptional leadership. We have outstanding leaders in our ranks and, going forward, we want to make sure we have the best leaders possible; leaders who will respect and support the work being done every day. We believe Holly fits this mold and will be a great addition to our organization.”
When talking about the opportunity she has in front of her at SMH, Zajic is very impressed with the level of care and expertise SMH has in place within its ambulatory clinics.
“Not many communities the size of Sheridan has the depth of healthcare services and expertise SMH provides,” she said. “Streamlining and coordinating these services for our patients, is exciting, and I look forward to working with our providers, staff and patients to develop them.”
The ambulatory clinics Zajic will have in her purview include: Women’s Clinic, Internal Medicine, Urgent Care, Occupational Health, Cardiology, ENT, Audiology, Big Horn Surgical, Rheumatology, Geriatric Medicine, Addiction Medicine and Wound Care.
Hailing from the small western Nebraska community of Hemingford, Zajic received her undergraduate and graduate degrees from Chadron State College. She had spent the majority of her professional career as Chief Operating Officer at Ivinson Memorial Hospital in Laramie.
So why make the move to Sheridan?
“My two boys are in college now and I couldn’t pass up this remarkable opportunity with SMH. Sheridan is absolutely beautiful and I couldn’t pick a better place that fits my interests and hobbies,” Zajic says. “Plus, my twin sister lives here with her family.”
I love everything outdoors and Sheridan has that in abundance. I enjoy mountain biking, paddle boarding, downhill and cross-country skiing and snowshoeing. If I’m not working and you need to find me, I’ll be outdoors.”
Her driving passion of service seems to be what will help Zajic be successful at SMH.
“I am passionate about service to others and creating an environment in which people are able to thrive,” Zajic states. “In healthcare, we have the opportunity to impact lives every day. That really drives me.”

How does a bachelor’s degree in Fisheries Biology end up landing you a job in the housekeeping department of your local hospital and ultimately lead to a position as a Registered Nurse? Jennifer Meineke, RN at Sheridan Memorial Hospital’s Medical-Surgical unit, can tell you.
Coming out of high school, Meineke, originally from Ohio, was looking to get away from the Midwest and landed in Laramie at the University of Wyoming (UW) where she graduated with the degree that had her working in federal and state fish hatcheries for approximately 20 years. Even though she loved her job and was good at it, she decided a different direction was needed in her life.
“As you age, your back starts hurting, and you start thinking long term and what you want to do with your life and nursing seemed like a good fit,” Meineke said. “I had been a volunteer at one of the local rural fire departments and really enjoyed interacting with the patients.”
It was at this time Meineke made a plan to reach her goal of becoming a nurse. So the next step, obviously, is landing a job in the SMH Environmental Services Department (EVS). This really was part of her career plan.
“I thought working in housekeeping would give me a really good opportunity to get to know people from across the entire hospital,” Meineke explained. “I know at least one person in each department and I was able to see how they operate and work together. It made my transition into the RN position much easier.”
The other factor that made the EVS position so attractive was the fact her manager was able to work with her schedule. This was important as she took the leap to attend Sheridan College and complete her associate’s degree in nursing. Now she is enrolled at UW, again, this time for a bachelor’s in nursing.
“Luckily a lot of my credits from my previous fisheries degree were science related and transferred to my new degree. I didn’t realize fish and people were so similar,” she said with a chuckle. “Those credits were from classes like biology, genetics and statistics.”
Meineke reached her goal and is now serving as an RN in a Preceptorship at SMH and continues to fit in UW courses towards her bachelor’s degree. Looking back, she is very thankful for the SMH Foundation and specifically the Cato Scholar Award she received. The award is made possible by the Wayland H. Cato, Jr. and Marion R. Cato Foundation.
“That scholarship made a huge difference in my ability to pursue this dream of becoming a nurse,” Meineke said. “It allowed me to be able to do a Preceptorship at Wyoming Medical Center in Casper on the neurology floor. It was very valuable to see how things are done at a different hospital. I am very grateful to the Cato family members for their generosity and vision which supports the Foundation’s Clinical Scholarship Program.”
Meineke is also grateful for Laura Ray and Nicole Haley, the preceptors who are mentoring her as an RN in her current position at SMH.
“There have been a lot of people who have helped me get where I am today and Laura and Nicole have been great,” Meineke said.
She went on to say, “Ada (Kirven) has been very helpful with any Foundation questions I had. My previous EVS Manager Casey Cornell and the current EVS Manager Karen Wemple were always helpful in working with my schedule. Lacey (Johnson) and Meghan (Reinemer) in MedSurg have been very helpful and positive. Our CFO (Chief Financial Officer) Nathan Stutte really helped mentor me when I was helping lead the EVS team during COVID last year. I appreciated Nathan’s approach, he really understands the importance of showing people that you care.”
Meineke is scheduled to graduate from UW with her bachelor’s in nursing degree in August of 2022.

The Foundation’s successful Clinical Educational Endowment was initiated in 2003 with private donations. Annually it provides nursing scholarships and clinical education opportunities for hospital staff members. The goal of the program has remained the same throughout the years, to strengthen and ensure excellent patient-centered care for our patients and their families. The endowment continues to grow with new gifts, and evolve with the growth of Sheridan Memorial Hospital and healthcare needs of our community.
The Foundation proudly announces Miranda Cone as the recipient of the 2021-2022 Cato Scholar Award. Miranda has been a member of Sheridan Memorial Hospital’s Medical/Surgical team for over two years and is an active community volunteer with The Food Group in Sheridan. The annual Cato Award is possible because of a generous donation from the Wayland H. Cato, Jr. and Marion R. Cato Foundation.
Sheridan Memorial Hospital’s Medical/Surgical team for over two years and is an active community volunteer with The Food Group in Sheridan. The annual Cato Award is possible because of a generous donation from the Wayland H. Cato, Jr. and Marion R. Cato Foundation.
Miranda expects to graduate with her Associate Degree of Nursing from Sheridan College in spring 2022 and work as an RN while completing her BSN. The Foundation along with our hospital’s Nursing Leadership applaud Miranda on her efforts to achieve her goals. As she stated, “Whether in school or at work, I strive to give my best effort and be successful. Becoming a nurse has been a dream of mine since I was in high school, and receiving this scholarship gets me one step closer to achieving that dream.”
Along with The Foundation’s Cato Scholar Award, 27 additional clinical scholarships were awarded to hospital staff members.
Scholarship funds are distributed annually each spring through an application and interview process. Nursing leadership from the hospital, along with Foundation Board members and staff, review and select the recipients. Including this year’s awards, The Foundation has granted nearly $400,000 in nursing and clinical scholarships. “We are extremely proud of our Sheridan Memorial Hospital staff, and grateful to provide opportunities for development through this endowment built by our generous community,” states Director of Donor Relations Ada Kirven. “The Foundation’s ability to assist in advancing team members with the skills and knowledge they need is a wonderful investment in the hospital’s greatest asset – our people – this program has positivity impacted excellent care for the region, and the endowment will continue for years to come.”
Awardees received scholarship funds for a variety of educational opportunities such as Associate, Bachelor, and Graduate Degrees at a diverse group of colleges and universities; and specialty certifications and training. Recipients come from clinics and departments across the organization including: Women’s Health Labor and Delivery, Medical/Surgical Unit, Women’s Clinic, Welch Cancer Center, Wyoming Rehab, Wound Care, Emergency Department, ICU, Primary Care, and Surgical Services.
To learn more about The Foundation or make a gift to our educational programs, contact us at sheridanhospital.org/foundation or by calling 307.673.2418 today!

Summer weather calls many of us to spend more time outdoors. While this time of year brings a welcome respite from our cold Wyoming winters, it also brings higher temperatures and risk for heat-related illnesses and heat stroke. As the body’s temperature rises and gets too hot, some of the first symptoms that occur are excessive sweating, cool clammy skin, nausea and vomiting and muscle cramps. This is known as heat exhaustion, and can occur with or without heat cramps or heat syncope (passing out).
However, if your body’s temperature continues to rise to 104 degrees Fahrenheit or higher, you can progress to heat stroke. Symptoms of heat stroke include balance difficulties, hallucinations, confusion, passing out, seizures and other complications involving the central nervous system. Heat stroke can cause permanent brain damage and is life-threatening.
There are several myths regarding heat stroke that should be dispelled. A common misconception is that you stop sweating when heat stroke occurs. In reality, heat stroke often occurs during extended exertion in the heat, so people are almost always still sweaty as they enter the territory of heat stroke.
Another myth is that you must be severely dehydrated to develop heat stroke. Dehydration may predispose you to heat illness, and can make it worse, but does not have to be present. Heat stroke can occur after only 20 minutes of exertion and before you have lost much fluid. The intensity of exertion and temperature are the main contributors.
Keep in mind that things are not always as they appear. For instance, the most common ways to take your temperature are with an oral or forehead thermometer. However, your body’s external temperature does not always match its core temperature. In addition, people who are developing heat stroke may not appear dizzy, confused, or off balance initially while they are in the early stages of heat stroke and may then deteriorate rapidly as their body temperature rises further.
Certain factors can put you at higher risk of developing heat stroke. These include high environmental temperature, intense exertion, being out of shape, equipment preventing heat loss (football pads, firefighter PPE, and multiple layers of clothes), obesity, sleep deprivation, dehydration, and fever.
Heat stroke is a risk for any age group. For example, infants do not have the ability to change their environment or clothing on their own. Children left in hot vehicles are at particular risk. High school football players are also at risk from intense exercise, sometimes twice a day at the beginning of the season in August. Working adults such as roofers and firefighters should be aware as they exert themselves in hot environments. Finally, seniors are also predisposed to heat related illness, particularly if they do not have air conditioning, their air conditioning fails, or there is a power outage.
There are several steps that you can take to prevent heat exhaustion and heat stroke. Be mindful of the weather forecast and be willing to adjust your plans for the day. If it is going to be hot, don’t make big plans for exertion and plan to take frequent breaks. Plan any exercise, hikes, or outdoor work earlier in the day, when it is not as hot.
Avoid dehydration by drinking plenty of fluids such as water or sports drinks and avoid caffeine and alcohol. Keep in mind that diarrhea, vomiting, and fever all increase your water loss and can also predispose you to dehydration and heat-related illnesses. An easy way to track your hydration level is to monitor your urine color. The darker the urine, the more dehydrated you are. Hydrate to the point that your urine is pale yellow or clear.
Also keep in mind that our vehicles are a particular risk for exposure to high temperatures. A car in the sun can heat up by 20 degrees in only 10 minutes. A study measuring temperatures in cars parked in the sun on a 95 degree found the average temperature reached to be 116 degrees. Consider running your vehicle’s air conditioning for 10 minutes before entering and never leave a vulnerable adult or child in a hot vehicle.
If you plan to be outside in the heat, wear loose lightweight clothes and avoid wearing multiple layers that would keep your body from cooling properly. If you feel that you are getting too hot, remove extra clothing and move to the shade or air conditioning if possible. Taking a cool shower or bath can also be very effective. If this is not possible, getting wet and sitting in front of a fan can cool you through evaporation. Cold packs (or anything else cold such as a bottle of water from the refrigerator) can be placed on your neck and in your armpits and groin to cool you further.
However, if you or someone else continue to worsen despite these measures or begin to experience balance difficulties, confusion, hallucinations, passing out, or seizures seek medical attention immediately, even if you have to call 911. Enjoy the summer weather, but do so safely.

The Sheridan Memorial Hospital Foundation board members and staff are excited to announce, thanks to the generosity of our community; we’ve met the $4.4 million fundraising goal for the Transitional Care Expansion. All gifts and pledges in the last month were matched by The Foundation and helped complete the final push to reach the goal. Nearly 1,000 donors from our community made it all possible.
As initially planned, reaching this goal allowed Sheridan Memorial Hospital to begin construction on the 2nd and 3rd floor of the original 1954 hospital on Thursday, July 1st. The expansion increases the hospital’s eight current Transitional Care rooms to 20 comfortable, private rooms. The new Transitional Care Unit is scheduled to open in the summer of 2022.
Foundation Board President and Campaign Co-Chair Richard Garber shared the good news, “It not only fills the growing need to care for individuals after a hospital stay, but will also help ensure their safe and successful return home. Another positive is that this project repurposes the original 1954 building back to patient care. This is an excellent use of space and, once completed, our professional care team of providers and rehabilitation staff will be able to offer excellent care to more individuals. It all comes down to keeping people in Sheridan, close to home and their loved ones.”
Cody Sinclair, Chief Development Officer for the Foundation, said, “It has been an amazing experience sharing this project with our community, and we appreciate everyone who’s contributed to the success of this campaign. We have heard countless stories of the gratitude our patients and families feel to have excellent healthcare close to home.”
Those still interested in supporting the Transitional Care Expansion are welcome to play a part in the project. Any additional donations and gifts received will be utilized to help the hospital defer additional construction. Initial estimates of the project were at $8 million, while the final cost is $8.3 million.
At the Sheridan Memorial Hospital Board of Trustee meeting held on Wednesday, June 30, at 4 pm, Dr. Doughty, Richard Garber, Ada Kirven and Cody Sinclair presented a ceremonial check to the hospital announcing The Foundation reached its goal of $4.4 million thanks to our generous community.
The Foundation plans to host a celebration of the past year’s successes on July 27th at the hospital starting at 5 pm. The Foundation invites all donors to the event, on the patio in front of the Sheridan Memorial Outpatient Center. For more information, please get in touch with The Foundation at 307.673.2418.
To get the most up to date Foundation information and learn more about the Transitional Care Expansion Project, visit sheridanhospital.org/foundation.

David Nickerson, MD, urgent care physician at Sheridan Memorial Hospital, has completed the necessary training through the Federal Aviation Administration (FAA) to become an authorized Aviation Medical Examiner (AME) for second-and third-class pilots. Dr. Nickerson completed the FAA Aerospace Medical Certification Division training in Oklahoma City and has passed the national certification exam.
An AME is a physician designated by the FAA and given the authority to perform flight physical examinations and issue aviation medical certificates if the applicant meets FAA standards. There are approximately 6,000 AMEs nationwide; there are only 10 in Wyoming.
While all pilots must receive some type of health assessment before flying, the levels of certification vary. Generally, the first-class certification is designed for airline transport pilots; second-class for commercial pilots, including corporate aviators, crop dusters and charter pilots; and third-class for student, recreational and private pilots.
For pilots seeking a flight physical medical certificate, the process requires a physical exam, in addition to testing to assess mental, neurological and general health. A vision and hearing test is also performed, as well as a urinalysis to check for diseases or other potential medical conditions.
Dr. Nickerson is board certified in Emergency Medicine and has worked in Emergency Medicine, Urgent Care, and Occupational Health at Sheridan Memorial Hospital for the past eight years.
To schedule your 2nd or 3rd Class Flight Physical with Dr. David Nickerson today, call 307.675.5850.

By Dr. Christopher M. Prior, DO, FAAFP – Physician at Sheridan Memorial Hospital’s Internal Medicine Practice
June is Men’s Health Month, and according to studies, 60% of men don’t consult their physician regularly and 33% are less likely to visit the doctor than women. But one area of men’s health is seeing a surge in activity.
Use of testosterone hormone as well as natural testosterone level boosting supplements has skyrocketed in recent years with people looking for treatment of fatigue, poor cognition, difficulty losing weight or gaining too much weight, and erectile dysfunction. The most common cause of low testosterone is age related low testosterone. Most adult males lose 1-2% testosterone annually after their mid-thirties. Chronic diseases such as obesity, sleep apnea, drug and alcohol abuse, hemochromatosis (harmful levels of iron in the body), as well as exposure to radiation or chemotherapeutics are potential causes of low testosterone. Rarely do genetic disorders lead to hypogonadism (a failure of the gonads, or testes, in men).
Treating potential causes of hypogonadism before starting testosterone supplementation would be the most common recommendation. Many people, however, seek over the counter supplements first. Unfortunately, some over the counter supplements can worsen symptoms or have adverse side effects. For example, there has been an increased number of young men in their 20’s and 30’s diagnosed with secondary hypogonadism caused by taking testosterone boosting supplements or illegally using testosterone hormone. Inappropriate use of testosterone can worsen sleep apnea, cause polycythemia (increases red blood cell count), elevate prostate specific antigen, increase cholesterol, as well as increase risk for stroke and heart attack.
Many urban areas have seen an increased number of low testosterone retail clinics. Most of these are cash only, with no insurance coverage for medications, lab tests or the prescription supplementation frequently recommended. Expensive blood work, estrogen blocking medications, pituitary stimulating hormones as well as testosterone supplementation can be cost prohibitive for most. While some users claim to feel better, think better, sleep better, and lose weight, there is very little evidence to support these claims.
Recently, the two largest medical organizations in the United States, the American Academy of Family Physicians and American College of Physicians agreed that the only clear reason to treat low testosterone is erectile dysfunction. While testosterone has been used to help bone density, cognition, anemia, overall well-being, and infertility—there are no articles suggesting benefits in these areas with testosterone supplementation.
Routine screening of testosterone levels is not recommended for asymptomatic males. When a patient has symptoms that may be related to hypogonadism they may be screened for low testosterone in addition to the previously listed chronic causes of hypogonadism. If testosterone levels come back low, testosterone replacement therapy can be initiated, with appropriate monitoring regularly with blood tests and clinical symptoms. This is generally a mutually agreed upon decision by the patient and provider after a review of risks and benefits.
Talk to your primary care provider about your healthcare concerns. If you don’t have one, check out Sheridan Memorial Hospital’s Internal Medicine practice or call: 307.675.2650

By Barb Hespen DNP, RN, Chief Nursing Officer at Sheridan Memorial Hospital
National Certified Nursing Assistant (CNA) week is June 17-23, 2021. This week is a way to honor those who work in this demanding profession which requires meeting the basic care needs for patients in hospitals, skilled nursing facilities, in assisted living and in patients’ homes.
At Sheridan Memorial Hospital (SMH), we have 40 CNAs who are the heart of our patient care areas. They provide bedside, hands-on care to our patients – assisting the nurses with many, many responsibilities. CNAs play a critical role in the patient care team — answering the patient’s questions and responding to their needs. Quite a few of our CNAs perform a dual role as unit clerks, managing information and communication within their departments.
The most common duties that CNAs provide to patients under the direction of Registered Nurses (RN) include:
- Assisting patients to clean and bathe themselves
- Helping with dressing and toileting needs
- Turning and repositioning patients to keep skin healthy and to prevent skin breakdown
- Serving meals and assisting with eating as needed
- Completing and documenting Vital Signs (Blood pressure, Temperature, Pulse Rate, Respiratory Rate, and Oxygen Saturation readings)
These duties are clearly very important to patients, as are the CNA’s behavioral skills, including having a high level of patience, compassion, empathy, attention to detail, communication skills, sense of humor, and physical strength. All of these characteristics of CNAs ensure that patients receive excellent care while in hospitals, nursing homes or in their own homes.
The CNA career is a rewarding and fulfilling one, and these skills are in high demand with the expanding healthcare needs of our aging population. A CNA can make this a life-long career, or they can build on the learning and experience and expand their schooling into another healthcare field.
I have worked with CNAs who have cared for patients and their families for 30+ years and are excellent in the care that they provide. I also have worked with CNAs who have advanced their knowledge by becoming RN’s, Physical Therapists and Lab Technologists. I started as a CNA early in my career and learned valuable skills that have continued throughout my nursing career.
Please take time this week to thank a CNA who you work with for all of the care that they provide to our patients. Happy CNA week!
If you are interested in becoming a CNA, learn more about Sheridan College’s CNA course by clicking HERE. If you are a CNA and would like to join our Team at Sheridan Memorial Hospital, visit our careers page and check out our current job opportunities HERE.

By Cody Sinclair, Chief Development Officer of Sheridan Memorial Hospital
Sheridan Memorial Hospital (SMH) strives to meet community and regional demand for patient care. Over the past year we have become even more aware of the importance of growing and adapting in ways that add value for our patients and appropriately meet the needs of the Sheridan community and region. Providing care close to home ensures people are able to stay near their family and friends when health issues arise.
One area where care close to home is especially important is Transitional Care. Having a comfortable, private environment to heal and regain strength and confidence for a safe return home following a serious illness, injury, or surgery is critical. SMH is fortunate to have an outstanding Transitional Care team of providers, therapists, nurses, and case managers who work with patients to help them recuperate and rehabilitate. The goal is to help each individual regain their strength, confidence and independence for a safe return home and to their lives.
SMH’s Transitional Care service began in 2006. Since then, our patient’s need has continually grown. In 2017, the hospital cared for an average of four patients per day. Today, the hospital averages eight Transitional Care patients per day; however, the need already surpasses the hospital’s current bed capacity to provide or expand with the growing senior population. According to data from the Centers for Medicare & Medicaid Services (CMS), SMH currently serves approximately 17% of all Transitional Care needs for our community, while over 18% of Transitional Care needs are being met outside our community. This means patients and their families may have to leave Sheridan and travel long distances for care. This presents a hardship for families to visit and support their loved one throughout their recovery process. Based on data from two separate third-party vendors, the hospital anticipates a continued increase in patients due to growth in our community, especially in the over 65 and retirement age population. Because the majority of patients (85%) are in this growing demographic, SMH has made plans for an average of 18 to 19 patients per day by 2024 based on this data.
Fortunately, through the support of The Foundation and generous contributions from our community, SMH will expand Transitional Care to fully meet the need for care close to home. The expansion, which includes repurposing space on the 2nd and 3rd floors of the original 1954 hospital, will increase the hospital’s Transitional Care rooms from 8 semi-private rooms to 20 comfortable, private rooms. Thanks to our community’s generosity over the past eight months, The Foundation is nearing its fundraising finish line with a completion goal of June 2021. With our community’s generosity and support, SMH plans to begin construction in July 2021 and open its new Transitional Care Expansion in the summer of 2022.
To learn more about the Transitional Care Expansion, please visit sheridanhospital.org or call our Foundation Office at 307.673.2418.
Dr. Jason Ackerman has been practicing medicine in Sheridan for the past 8 years and has been a mainstay in the Sheridan Memorial Hospital Internal Medicine Clinic. He is excited about opening an Addiction Medicine Clinic here in Sheridan. We sat down with him recently to get his thoughts on this new adventure in his career, why he is taking this leap into addiction medicine and what it means for the Sheridan community.
Q: Dr. Ackerman, tell us why you felt it was important to get this certification and open this clinic in Sheridan.
A: I started treating opiate addiction while I was in residency and continued that when we moved to Sheridan after residency. It was initially a very small part of my practice, but it began to grow more rapidly the last few years. I came to realize how underserved and undertreated patients with addiction are in our community. When I had a chance to get boarded in Addiction Medicine it seemed like a good opportunity to broaden my knowledge base and start helping more patients with a variety of addiction problems.
While it’s been needed in Sheridan and our surrounding communities for a while, it’s also been one of the most rewarding aspects of my practice. Not only is it a chance to improve patients’ health, in many cases it is truly giving people a second chance at life. I have had homeless patients find housing and start working. I have had patients go back and get college degrees and others start new careers. Parents who have lost their children due to addiction have been able to get their kids back home. They see successes that they never thought were possible and it’s amazing to be a part of that.
Q: What does it mean to see a doctor/physician who specializes in addiction? Aren’t most internists focused on physical health?
A: That certainly is our primary training and focus. But internal medicine spans a broad range of specialties. One of the great things about practicing here is that we can find our niche and develop skills in our area of interest. There is a big component of mental health in addiction, but as research progresses in the field we are learning more and more that this is a true disease process and not simply a series of bad choices. The good news is that means there are medications and therapies that we can use to help people recover and succeed.
Q: Is this a pain management clinic? What services are offered through the new clinic?
A: This is not a pain management clinic, although we have certainly helped people taper off of pain medications. Our focus is treating the disease of addiction, whether it is opioid pain medications, heroin, alcohol, stimulants, gambling – it really runs the gamut of substances and behavioral addiction.
Q: Can you talk about medication assisted therapy and what exactly is suboxone?
A: Just as some people are able to treat their diabetes with diet and exercise while others need insulin and other medications, there are a number of ways to approach the disease of addiction. Some people do well with counseling or groups like Alcoholics Anonymous. But when we start looking at the process of disease, there are some medications that can significantly improve people’s chances of recovery. Medication assisted therapy is using evidence-based, targeted medications to help people achieve that recovery. Suboxone is probably one of the best known and most effective medications. The primary component of it is buprenorphine, which is a partial opioid agonist. That’s essentially a fancy way of saying a medication that hits all the same receptors as opiates like pain medications or heroin, but turns on those receptors just enough that people do not have cravings or withdrawal symptoms. That allows people to not only remain clean and sober, but also increases their ability to incorporate all the important tools from other aspects of treatment – groups, counselors, etc. – and substantially increases the chances of long term sobriety.
Q: Are there specific areas of addiction on which you concentrate?
A: Not really. Part of that is that addiction is a broad field that seems to be evolving fairly rapidly at this point. The other part is that addictions don’t always come packaged quite as neatly as we used to think. Many people are able to get off of pain pills, only to develop an alcohol problem or a meth problem. There seems to be a genetic component and it can definitely run in families. Some people just seem to be wired to have problems and addictive tendencies with whatever substance crosses their path. I will say treating opiate addiction is very satisfying. We all see the headlines about skyrocketing fatalities from opiate overdoses. In clinic we see patients that have been using for years and cannot function without massive, potentially lethal doses of opioids in their system. They are literally a bad night or a tainted batch of pills away from dying. But when we can find the right doses and combinations of medications they are able to get clean relatively quickly. The patients frequently tell us that they feel “normal” for the first time in years.
Q: Do prospective patients need a referral to this new clinic? How does the process work?
A: We are always happy to take referrals, but you certainly don’t need one to get an appointment. People can just call us at 307.675.2674.
Q: If I have concerns about a family member or friend who may be addicted, how can I best help them?
A: That’s an incredibly difficult position to be in. Ultimately, patients with addiction need to be ready to get better. Sometimes that readiness comes with the urging of friends and family, sometimes it happens spontaneously, and sometimes a person has to hit bottom before they see that change needs to happen. I think being supportive and encouraging them to get help is really important. And if they’re just not ready at this moment, don’t give up – they will need your support when they are.
Q: Tell us a little about the partnership with Northern Wyoming Mental Health (NWMH).
A: A few years ago we realized how much better our treatment for opiate addiction would be if we teamed up. At the time I was treating opiate addiction with suboxone, but had no real links with counselors. Meanwhile they were treating a number of patients with opiate addictions but nobody to prescribe suboxone or other medications. Since then the partnership has really expanded and blossomed and covers all aspects of addiction. We have been fortunate enough to secure grant funding that can help some patients with the cost of medications and visits. We are able to have an amazing peer specialist (an addiction counselor who has recovered from addiction partially with the help of our program) and a wonderful case manager in our clinic on our main addiction treatment days. The partnership also opens up all the resources of NWMH to patients going through our program, including various group therapies, relapse prevention groups, individual counselors, and vocational rehab. I think a lot of our success stems from being able to align ourselves with their team.
Dr. Ackerman and the team at the SMH Addiction Medicine and Recovery Clinic are ready to serve the Sheridan community. If you have questions or need to schedule an appointment, please call 307.675.2674. For additional information please click here.

Thanks to generous gifts from planned giving and The Link annual event participants and sponsors, the Sheridan Memorial Hospital Foundation Board approved funding for over $325,000 in vital equipment upgrades at the hospital. The funding supports the replacement of equipment, which ensures excellent patient-centered care throughout the hospital.
According to Cody Sinclair, Chief Development Officer, “The Foundation is grateful for our community’s ongoing support. This tradition of healthcare philanthropy helps ensure our expert physicians and care teams have the equipment and technology necessary to provide the care our community has come to appreciate and value. ”
Specific funding announced today will purchase needed cardiology EKG (electrocardiogram) equipment to monitor various heart conditions in Internal Medicine, the Heart Center, Griffith Emergency Department, Intensive Care Unit, and the Cardiac Cath Lab. This equipment supports patient safety as well as faster turnaround time for physician diagnosis. The funds will also support the upgrade and replacement of the video monitoring system in the Cath Lab. The improved technology and additional capacity will provide clear and precise views during procedures, support quality care and patient safety in the Cath Lab. This special cardiology equipment purchase is possible through a planned gift from The Lorraine S. Husman Trust.
The other vital piece of equipment approved for funding is known as a Gamma Finder. Used in the operating room by the hospital’s surgeons and clinical staff, it allows the team to identify potential cancer nodes and, if indicated, an actual biopsy completed during the procedure. The Foundation’s Annual Link – Partners in Pink event proceeds used to make this purchase support cancer care, prevention, screening, and early cancer detection for our patients.
“Philanthropy continues to fund important projects for Sheridan Memorial Hospital and ensures everyone in our community receives needed care. A big ‘Thank You’ goes out to all those people, past and present, who through their generosity helped make these projects all possible,” Sinclair added.
To learn more about The Foundation, please visit sheridanhospital.org/foundation.

By Lynn Grady, RN, BSN – Sheridan Memorial Hospital Emergency Department and Intensive Care Unit Manager who also heads up the hospital’s Stroke Program
Every 40 seconds in the United States, someone experiences a stroke. Stroke is a debilitating and deadly injury to the brain that causes a death every 3.5 minutes in this country. Often the death follows a lengthy illness that limits a person’s participation in the daily activities of life.
Fortunately, there are several things you can do to minimize the risk factors of experiencing a stroke. Managing health conditions such as atrial fibrillation, high blood pressure, high cholesterol, diabetes, and eliminating lifestyle risk factors such as smoking can significantly decrease your risk of experiencing a stroke. Other lifestyle changes one can make to decrease the risk of stroke include maintaining a healthy weight by eating a healthy diet and engaging in regular exercise regimens, minimizing alcohol consumption, reducing personal stress levels, and maintaining regular appointments with one’s healthcare provider. Despite the best efforts of the healthcare industry in providing education and resources, stroke remains the 5th leading cause of death in the US since 2015.
If you do experience signs and symptoms of a stroke, such as sudden numbness in the face, arm, or leg, especially on one side of the body, or sudden confusion, difficulty speaking, or loss of coordination, call 911 immediately or immediately get to the Emergency Department. If someone you know is experiencing these symptoms, a quick and easy way to determine if this person may be experiencing a stroke is the F.A.S.T. mnemonic.
F – Face: Ask the person to smile. Does one side of the face droop?
A – Arms: Ask the person to raise both arms. Does one arm drift downward?
S – Speech: Ask the person to repeat a simple phrase. Is the speech slurred or strange?
T – Time: If you see any of these signs, call 911 right away.
As a stroke can happen in several different areas of the brain, a patient may experience varying degrees of speech and motor symptoms. This is why it is important to immediately seek medical attention if you are experiencing even one of the symptoms above. Acting F.A.S.T is key to minimizing long-term effects that may be experienced due to a stroke. A quick diagnosis is critical to ensure that a patient receives the treatment and medication they need in order to regain as much function as possible.
At Sheridan Memorial Hospital, we are able to offer our community rapid brain imaging and access to a neurologist by using our Tele-Stroke services provided through Wyoming Medical Center. This provides our staff and patients direct access to stroke experts and optimal treatment options that would otherwise not be available in a community in the size of Sheridan. One of the potential treatment options is a medication called TPA, a powerful anticoagulant (blood thinner) that can be used to help dissolve the clot that is causing the stroke. We are able to provide this particular treatment in Sheridan so that our patients can stay home in their community alongside their families while receiving care. TPA, however, must be administered within 4 hours of the initial onset of symptoms — another reason why time is of the essence if you think you may be experiencing a stroke.
After the initial treatment of the stroke, our patients can then go on to receive physical and occupational therapy services offered by Sheridan Memorial Hospital’s Wyoming Rehab to ensure that they can regain as much strength and function as possible prior to being discharged. If TPA is not an option for the particular type of stroke a patient is experiencing, a treatment plan can be quickly determined between our physicians at Sheridan Memorial Hospital and the neurologists through Wyoming Medical Center.
If you have any questions regarding your potential stroke risk factors, you are highly encouraged to schedule an appointment with your primary care provider to address these concerns. If you don’t have one, check out Sheridan Memorial Hospital’s Internal Medicine practice or call: 307.675.2650

The Sheridan Memorial Hospital Foundation Staff and Board of Directors are pleased to announce Wendy Smith as their newest Board Member. Wendy is the Associate Vice President for Strategic Communication at Sheridan College.
Board President Richard Garber shares, “We are thrilled to welcome Wendy Smith to our Foundation Board of Directors. I have known Wendy for at least ten years. I had the pleasure of serving with Wendy on the Sheridan County Chamber of Commerce Board of Directors, where she demonstrated excellent communication and leadership skills. I look forward to seeing how her unique insight and energy will influence the work we do here at The Foundation.” Along with the officers and directors, Foundation staff share in the excitement to welcome Wendy as part of the board. “Wendy is a leader and connector in our community,” said Chief Development Officer Cody Sinclair. “She cares deeply about Sheridan and the Foundation’s mission to cultivate community involvement and support the hospital’s vision: When people think of excellent healthcare, they think of Sheridan.”
Wendy is an outdoor enthusiast who enjoys all of the wonderful wilderness Wyoming has to offer. From kayaking and hiking in the summer to skiing in the winter, Wendy takes every opportunity to embrace adventure with good friends and family. Beyond her recent induction into The Foundation, Smith currently serves as a board member for Leadership Wyoming and is a longtime member of the FAB Women’s Conference planning committee. She has also served on the Center for a Vital Community (CVC) Board, as well as on the Sheridan County Chamber of Commerce Board and Governmental Affairs Committee. Her extensive leadership training includes Leadership Sheridan County, Sheridan CiViC Project, Leadership Wyoming and Academic Management Institute. She has also earned her Gracious Space certification through the Center for Ethical Leadership.
With all the challenging work ahead of The Foundation, Wendy’s leadership, drive, and community spirit is a welcome addition to The Foundation Board. The Foundation looks forward to the experience, energy, and perspective Wendy will bring in the coming year and all we will accomplish for healthcare in our community – together.
To get the most up-to-date Foundation information and learn more about The Board of Directors, visit sheridanhospital.org/foundation or call Director of Donor Relations – Ada Kirven at 673-2417.

National Volunteer week falls in April of each year and provides an opportunity for organizations around the country to celebrate the impact of their selfless and inspirational Volunteers. At Sheridan Memorial Hospital (SMH), our volunteers are the heart of our organization. Every service given to our hospital is another chance to provide excellent patient-centered care to everyone in our community.
At SMH, we are lucky enough to work alongside unique, talented, and genuine volunteers who serve as irreplaceable resources to our organization. We are gifted with a group of individuals dedicated to this organization and the health and wellness of our entire community. Our volunteers make an effort to create an environment of comfort and cultivate a Culture of Kindness in everything that they do, and it wouldn’t be possible without them.
Our volunteers are part of our culture, our patient experience, our family. Their friendly greetings and genuine smiles, kind hearts, and overwhelming support to all those they encounter are what complete the heart of Sheridan Memorial Hospital. This last year has taught us how truly invaluable our volunteers are. It was challenging to ask them to stay home and while we selfishly wish they were by our side to support our patients and staff, the overall health and safety of our volunteer family had to come first.
Looking back, it is humbling to think that even when not in our presence, though, in true fashion of our SMH volunteers, they met the pandemic like much of our community with heart and continued to help us support our patients and neighbors. They sewed masks, brought in PPE and other provisions, donated to COVID care funds, dropped off treats for our staff, but most importantly, they stayed home and helped us stop the spread. Our hospital volunteers wanted to be out there doing all they could, but what they did was much more significant and likely more challenging for such an active and social group. Our SMH volunteers stayed home, they masked up, and they distanced themselves to yet again support our staff in some of the most selfless of ways.
A year later, we look forward to what lies ahead. We look forward to gradually opening back up our Volunteer Program areas and welcoming back nearly 100 volunteers who serve our community at Sheridan Memorial Hospital. SMH can’t wait to see the smiles in their eyes, hear their laughs, and feel their warm presence in the hallways of our hospital. The staff is waiting patiently for your triumphant return, but know that all you did while away means just as much to all of us.
Thank you for every book you’ve donated to our newborn babies. We appreciate all of the shelves you’ve stocked with trendy and unique inventory in our Kozy Korner Gift Shop, so we are well dressed or decorated. We are grateful for all the Blood Drives you continue to coordinate, so we ensure our blood supplies are stocked and replenished when Sheridan Memorial Hospital patients and neighbors need it.
We are thankful for every tiny patient you comforted with your scrubby bears before and after surgery, every 5-year-old you have celebrated in the last 61 years (including over 150 children at this year’s drive-by event), and every time you guided us to our next appointment or relocated office on our hospital’s growing campus.
Our team can’t even begin to count how many people you’ve gifted a piece of home with the thousands of newspapers you’ve delivered, the cards you’ve sold visitors to leave our patients a kind note, or the sweet tooth you cured with our favorite candy bar in the late afternoons.
Thank you for joining us for the virtual zoom meetings and phone calls, being present, for sharing your thoughts and ideas, and for all the events you have attended because you, too, believe in medical excellence – right here at home.
It’s impossible to measure how many times you’ve warmed our hearts and hallways, the number of people who have been positively affected by your generosity, and it’s incomprehensible where Sheridan Memorial Hospital would be without you.
To learn more about Sheridan Memorial Hospital’s volunteer program go to www.sheridanhospital.org/community/volunteer-opportunities/ or
contact Jasmine Slater at jasmineslater@sheridanhospital.org or call 307.675.2620

Upon your initial introduction to Dr. Marty Lucas, you may notice that she carries a unique characteristic: a subtle southern inflection in the tone of her voice, so subtle, in fact, that you may not even notice it during your first interaction with her. However, while her accent may go unnoticed, her sincere passion for the service she provides and for the patients she treats is distinct and unmistakable, and we are grateful that Dr. Lucas has decided to bring her intense desire to help others to Sheridan Memorial Hospital’s Welch Cancer Center.
But Dr. Lucas didn’t develop her southern accent from living in Billings for 20 years. She was born and raised in the bustling city of Chattanooga, TN where she spent all of her early life before traveling to Knoxville to further her education at the University of Tennessee.
Dr. Lucas initially went to UT in hopes of becoming a nurse, and although she succeeded in doing so, she soon felt a desire to dive deeper into the medical field. “My father was a physician, and I just felt like that was the logical step for me to take in my life,” she explained. And so she decided to return to UT where she would soon find her passion for hematology. She recalled, “I had a mentor in Med School, who was probably the smartest lady I ever knew, who could just look at a blood smear under a microscope and almost immediately have a diagnosis for her patient, and she was the one who really led me into hematology.”
Soon after completing all of her schooling, including her residency, at the University of Tennessee Health Science Center in Memphis, Dr. Lucas began to practice as a hematologist. And although she has always enjoyed the science of hematology, she soon realized that there was nothing she loved more than the relationships she built and the lives she touched.
She expressed, “The best part of being a hematologist is getting to know the people and their families. None of the diagnoses we deal with are very easy diagnoses. Having the honor of walking these people and their families through these tough times, having the honor to be a part of their family, and to be able to help them through the good and the bad has to be my favorite part of practicing hematology.”
Dr. Lucas has come a long way from her early days in Memphis, she now has over 35 years of experience as a hematologist, and has practiced in both Tennessee and Billings. She anticipates a more relaxed pace here in Sheridan. “I look forward to the slower pace that comes with working in a small town community because it means that I get to have more one-on-one time with each patient and I can add more of a personal touch to the service I provide. It’s the main reason I believed that Sheridan Memorial Hospital was the right place for me.”
Dr. Lucas is a lover of the outdoors, with her hobbies including hiking, camping, horseback riding, dog walking, and doing “just about anything outdoors,” as she put it. And considering Sheridan is on the doorstep of the Big Horn Mountains, it wouldn’t be surprising if Dr. Lucas had more than one reason to choose Sheridan Memorial Hospital as the next stop in her life’s journey.
We are excited to welcome Dr. Marty Lucas to our team here at Sheridan Memorial Hospital and we look forward to seeing her passion for hematology and dedication to her patients at work here in our community.
To learn more about the Cancer Care team, based out of the Welch Cancer Center, go to www.sheridanhospital.org/medical-services/cancer-care/