Listen to what Dr. Lindsay Capron & Liz Becking, RN, share about
Celebrating Women, Women’s Clinic, and Women’s Health at Sheridan Memorial Hospital
Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
Listen to what Dr. Lindsay Capron & Liz Becking, RN, share about
Celebrating Women, Women’s Clinic, and Women’s Health at Sheridan Memorial Hospital
To learn more, visit Dr. Lindsay Capron or SheridanWomensClinic.org or call the clinic at 307.672.2522.
By Luke Goddard, MD – Emergency Department Physician and Chief Medical Officer at Sheridan Memorial Hospital
May is National Stroke Awareness Month with a goal to increase awareness around this very important public health problem. It is estimated that up to 150,000 deaths related to stroke occur each year in the US. That equates to 1 in 19 deaths, making it the 5th leading cause of death in our country.
Because many of the available treatments for stroke are time-dependent, a stroke is a medical emergency, and it is important to seek care as soon as you or someone you know develops signs or symptoms of a stroke.
A simple acronym to remember the most common signs of stroke is FAST.
F – Face drooping: ask the person to smile, does one side droop?
A – Arm weakness: ask the person to raise both arms, does one side drift downward?
S – Speech difficulty: ask the person to repeat a simple sentence, are the words slurred?
T – Time: if the person demonstrates any of these symptoms, call 911.
Other common symptoms include sudden dizziness, trouble walking, loss of vision, or sudden headache.
It is important to know that if you or someone with you is experiencing stroke symptoms, you should call 911 right away. The prehospital professionals at our ambulance service: Wyoming Regional EMS, have extensive training in the recognition of strokes and are able to activate resources at the hospital very quickly – even from your home. Because of this communication with EMS, we can anticipate your arrival at the hospital and be ready to care for you.
Once stroke patients arrive at the Sheridan Memorial Hospital, they are greeted by our team of professionals who are specifically trained in the diagnosis and treatment of stroke. When necessary, we also have the ability to connect via telemedicine with a stroke neurologist (a doctor who specializes in treating strokes) 24 hours per day to help make treatment decisions. In recent years there has been significant progress made in treating strokes using intravascular therapies performed by specialized physicians in larger hospitals, which may require a transfer outside of Sheridan.
Strokes cause brain tissue to die, which leads to brain damage, disability, and even death. Stroke is the leading cause of serious long-term disability. It is, however, estimated that up to 80% of strokes are preventable. You can greatly reduce your risk of stroke by making lifestyle changes such as stopping smoking, drinking alcohol in moderation, getting exercise, and controlling your blood pressure and cholesterol. Work with your doctor to discuss prevention or treatment strategies to lower your risk of stroke.
Let’s Talk Strokes – Free Community Presentation
Want to learn more? I would like to invite anyone who is interested to attend a free community presentation on Tuesday, May 23, beginning at 10:30 AM at The Hub on Smith, 211 Smith Street. Some of the topics I will be covering include: what a stroke is, the symptoms of a stroke, stroke therapies, and how to prevent a stroke. Be sure to bring your questions. This presentation is brought to you by the Stroke Team at Sheridan Memorial Hospital.
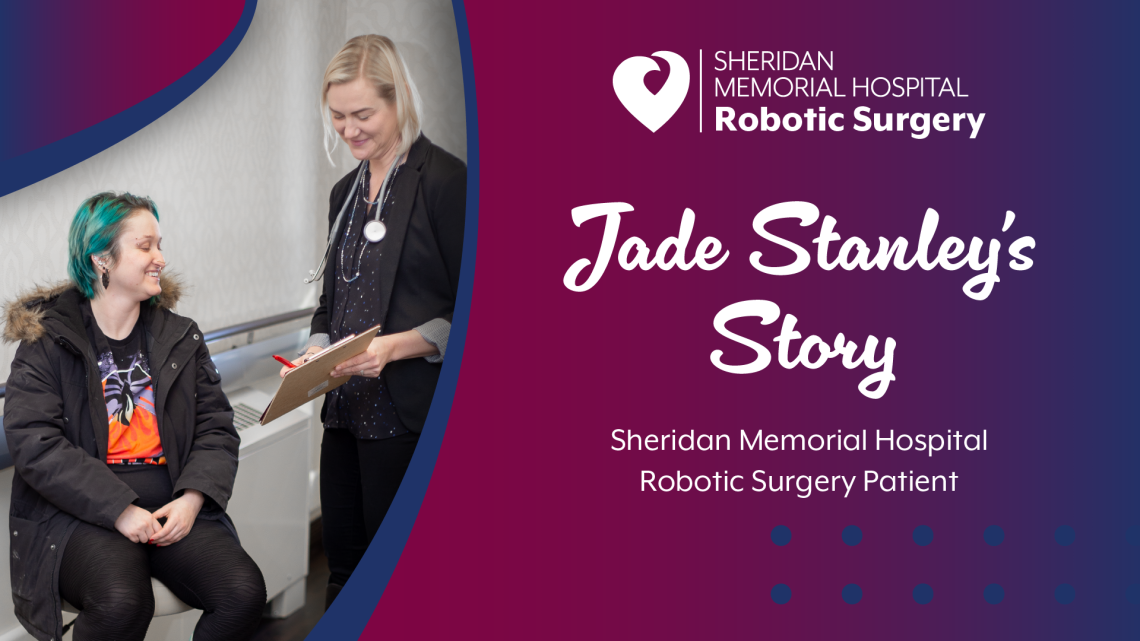
Jade Stanley, a local Sheridan resident, is the first Sheridan Memorial Hospital (SMH) patient to undergo hysterectomy surgery using state-of-the-art da Vinci® robotics. Stanley underwent the hysterectomy at the hospital in December and has been sharing of her positive experience since.
When asked why she chose SMH to perform her hysterectomy, Stanley said, “Our local hospital has great services, and I feel very comfortable there. The staff are all friendly, and the doctors are very knowledgeable. The SMH Women’s Clinic also delivered my child, so I wanted to stick with the people that knew my history.”
Rebecca Krzyminski, DO, one of the physicians at the Women’s Clinic who is specially trained in robotic-assisted surgery, performed the operation. Stanley had previously worked with Dr. Krzyminski, having glowing words for the staff and doctor, calling them “very knowledgeable,” “professional,” and “down to earth.” Stanley continued to share that the team at SMH “are all friendly and eager to assist. Dr. Krzyminski’s confidence is contagious.”
Stanley also spoke positively of her recovery, saying, “It’s been great.” She was able to walk out of the hospital the same day as her surgery and has been going ever since.
When asked if she would recommend SMH and robotic surgery to potential patients, Stanley said, “If you’ve got a hospital as great as this one in your neck of the woods, why go anywhere else? I would tell them not to be afraid. My recovery was virtually painless. It’s definitely the way to go.”
SMH is committed to providing excellent, patient-centered care with an outstanding healthcare team and state-of-the-art technology right here at home. Robotic-assisted surgeries are now available for anyone needing procedures such as hysterectomies, hernia repair, endometriosis, gall bladder removal, ovary removal, and prostate biopsy/removal.
To learn more about Sheridan Memorial Hospital’s minimally invasive robotic-assisted surgery, visit SheridanRoboticSurgery.com and Robotic-Assisted Surgery FAQs.

Listen to what Dr. Jason Ackerman shares about Sheridan Memorial Hospital’s Addiction and Internal Medicine Clinic, who they are, what they do, what addiction is, and MORE!
Learn more at Sheridan Memorial Hospital Addiction and Internal Medicine Clinic or call today for an appointment at 307.675.2674.

It’s Women’s Health Month, and the Sheridan Memorial Hospital Women’s Clinic is here to help answer any questions you have about women’s health. Whether you have questions about common conditions, preventative care, or anything else related to women’s health, we have the answers. This month, we’d like to share a few of the most common questions we receive about OB/GYN and pregnancy care to help women get the answers they need to take charge of their wellness.
OB/GYN Care
What is the difference between gynecology and obstetrics?
In general terms, gynecology focuses on women’s medical issues, specifically those related to the reproductive or urological organs. Obstetrics, on the other hand, is concerned with prenatal care, pregnancy, and labor and delivery. Because these two fields are so closely related, many physicians will study both and provide both types of care.
When should I have my first gynecological exam?
The answer to this question will depend. If you are experiencing problems or become sexual activity, you should see a gynecologist regardless of your age. Otherwise, you should consider scheduling your first pelvic exam around age 21.
What should I expect during my first visit to the gynecologist?
Typically, during your first exam, you will be asked to provide a detailed medical history and be given a few simple screening tests.
Pregnancy Care
When should I have my first prenatal visit?
If you suspect that you may be pregnant—if you have tested positive with a home pregnancy test, for example—you should call to set up an appointment right away. We will schedule a visit about eight weeks from your last menstrual period.
Are there any options for treating morning sickness?
Absolutely. Non-medical treatments may include eating something bland, like dry toast or crackers, before getting out of bed in the mornings. Foods that may be particularly difficult on the digestive system, such as greasy or spicy foods, should be avoided as they can exacerbate nausea. Try to take any medications with food rather than on an empty stomach, and drink plenty of water!
Sheridan Women’s Clinic has a great team of providers ready to take care of you. Our Clinicians offer comprehensive services for complete women’s health, from preventative well women’s exams to specialized OB/GYN care. If you have any questions regarding women’s care, from puberty through menopause and beyond, please don’t hesitate to reach out. We are here to help!
To learn more, visit SheridanWomensClinic.org or call us at 307.672.2522.

By Kelly Lieb, DMSc, PA-C – Director of Patient Experience at Sheridan Memorial Hospital
The Patient Portal: Knowledge is Power…but knowledge is more powerful when we put it into use
Research tells us there are positive relationships between patient engagement and shared-decision making when we evaluate health outcomes for our patients. With this comes the opportunity for patients to be empowered and positively impact their care. The Patient Experience Department at Sheridan Memorial Hospital values effective communication through a human experience and interaction with your care teams. We believe that the simple acts of connection, listening, and understanding of the patient’s journey contribute to the highest quality of care.
Not only are we living in a world of human connections but also digital interactions, which is also part of the patient journey. Providing a digital experience where patients can positively impact their care and, ultimately, health outcomes is a priority of our care team as we move even further into a digital world.
Improved timeliness of responses
The MySheridanHealth patient portal provides a digital opportunity for effective communication with clinical teams and improved timeliness of responses. We want to provide patients with care that respects their time, and supports improved access and decreased wait times. We recognize that your time is valuable, and the desire for quality and timely access to care is a priority for our patients. When we optimize the technology provided, we can connect and effectively empower the patient-provider relationship in real-time and at our fingertips. Knowledge is power, but knowledge is more powerful when we put it into use.
Most efficient way to communicate with your medical team
Did you know that MySheridanHealth is available at no cost to all patients receiving care at Sheridan Memorial Hospital and its affiliated clinics, including Internal Medicine, Primary Care, Big Horn Surgical, Ear, Nose and Throat, Heart Center, Rheumatology, Wound Care, and Women’s Clinic? Here, you can review your appointments, request medication refills, conveniently communicate with your healthcare provider, track health conditions, view results, and much more. “Using the patient portal is the most efficient way to connect with your medical team in any one of our clinics. You can request medication refills, discuss concerns, and feel connected to your care team,” according to Kristopher Schamber, MD.
It is also possible to review summaries of recent visits, surgeries, and procedures. The awareness and understanding of the information the portal provides can help you track your health conditions, manage your goals, and communicate directly with your provider. “Patient portal messaging is a great way to communicate with us, no waiting on the phone, direct communication, and no phone tag,” shares Hannah Hall, MD. It also allows for more effective human connections so that when you and your provider are face-to-face, you are on the same page and can move your care forward together.
Convenient and Confidential
The patient portal is not only convenient but also confidential, secure, and easily accessed 24 hours a day via an app on your cell phone (HealtheLife on the Apple App/Google Play Stores) or through a computer by accessing the MySheridanHealth.org website. We invite you to participate in the patient portal at Sheridan Memorial Hospital and work with us to optimize your knowledge and management of your healthcare. Welcome to the digital experience.
Learn more or get signed up on the patient portal at MySheridanHealth.org. Our SMH Records is here to help! Please reach out with questions at 307.672.1070 today!
By Christopher M. Prior, DO, FAAFP, CAQSM– physician at Sheridan Memorial Hospital’s Primary Care practice
April is Testicular Cancer awareness month. Testicular cancer is the most common solid tumor among males age 15-34 years old. The American Cancer Society estimates almost 10,000 new cases will be diagnosed this year and about 460 deaths. The incidence of testicular cancer is about one per 250 young men, with a peak incidence between ages 30-34 years old. Testicular cancer has an overall five-year survival rate of 97%.
Risk factors include undescended testis, personal or family history of testicular cancer, age, ethnicity, HIV infection, and infertility. Whites, Hispanics, and American Indian/Alaska Natives have the highest rates of testicular cancer. The incidence of testicular cancer has increased over the past several decades for unclear reasons.
Symptoms of testicular cancer include:
Epididymitis is another ailment that can present with similar symptoms to testicular cancer in the same age group. While a clinical exam can help differentiate the epididymitis from testicular cancer, an ultrasound of the scrotum is the imaging test of choice to diagnose these conditions.
The US Preventative Services Task Force recommends against routine screening in asymptomatic men by clinician and patient self-exams. The British Journal of Cancer reports that muscle-building supplements containing creatine, protein, and testosterone enhancing androstenedione increase the risk of testicular cancer by 65%.
Congress passed the PACT Act in August 2022. It included “reproductive cancers of any kind” on the list of presumed conditions for qualifying Gulf War and post-9/11 veterans exposed to toxins from burn pits. In this case, if you were exposed to burn pit toxins and now have testicular cancer, you do not need to prove the exposure caused the cancer because the VA has already established this connection. A claim may be initiated on your own, with the aid of the American Legion, DAV, VFW, or your local Veteran Service Officer Lisa Griffith 307.620.0884 or lisa.griffith@wyo.gov.
Young men must see their medical provider if they have symptoms related to testicular cancer. Survival rates have improved significantly as a result of increased surveillance and improved patient-specific or targeted therapies. Survivors need continued surveillance for possible re-occurrence, cardiovascular disease, infertility, as well complications of therapy.
Listen to what Dr. Emily Denney & Dr. Erica Rinker share about Healthcare for All Ages at SMH Primary Care!
Learn more at SheridanPrimaryCare.org or call today for an appointment at 307.675.2690.
By Joshua Scott, MD – General Surgeon – Advanced GI Minimally Invasive Surgery – Big Horn Surgical
March is National Colon Cancer Awareness Month, an appropriate time to explore this topic. Colon or Colorectal Cancer (CRC) is one of the most common cancers in the United States and the second leading cause of cancer death behind lung cancer.
Screening is recommended simply because it can detect colorectal cancer early and prevent unnecessary deaths. Colorectal cancer incidence and mortality rates have been declining in the US, likely due to the increasing screening uptake.
Since colorectal cancers typically don’t produce symptoms, the practice of screening enables us to look for cancer or precancerous lesions in individuals without symptoms. Screening is incredibly effective when it comes to colorectal cancer because, from the time the first abnormal cells start to develop, it takes an average of 10-15 years for those cells to become a colorectal cancer. Therefore, as one of the most effective tools for preventing colorectal cancer, screening allows us to find and remove precancerous lesions such as polyps and help identify people who would benefit from more frequent screenings. In addition, small cancers that aren’t yet big enough to produce symptoms can also be identified.
The US Preventive Services Task Force recommends adults between the ages of 45 and 75 be screened for colorectal cancer. Although most cases of CRC occur over the age of 50, initiating screening at age 45 balances the benefits of detection and prevention with the burden on the patient and the risk of harm from screening. If you are older than 75, it is recommended that you talk to your doctor about the necessity of continued screening.
There are reasons to start screening earlier or stop later for some people. It is estimated that only about two-thirds of adults in the US are up to date with colorectal cancer screening. Every year, about 140,000 people in the US will be diagnosed with colorectal cancer, and 50,000 people will die from it. Our best tool to decrease both of these numbers is screening.
Risk Factors
The risk of colorectal cancer increases with age, with more than 90% of the cases we see being diagnosed in people age 50 or older. Many factors are associated with an increased risk of colorectal cancer. Some of these risk factors are related to lifestyle choices and are, therefore, modifiable. Maintaining a healthy weight, being physically active, not smoking or chewing tobacco, avoiding heavy alcohol intake, and eating a balanced diet that limits red or processed meat intake can all help decrease your risk of colorectal cancer.
Colorectal cancer can cause symptoms as it grows. These symptoms include seeing blood in or on your stool, unintentional weight loss, a change in bowel habits and weakness or fatigue caused by a low blood count.
Types of CRC Screenings
There are several screening tools for colorectal cancer, including tests done on your stool and colonoscopy. The stool-based studies either look for evidence of trace blood that can’t be seen by the naked eye or look for altered DNA that can be associated with abnormal cells in the colon. Stool-based studies that look for blood must be repeated annually if negative. A negative stool DNA test needs to be repeated every three years. However, if a stool-based test results with a positive outcome, it will need to be followed up with a colonoscopy. Stool-based studies are only appropriate for patients with an average risk of colorectal cancer. Average-risk individuals are those who have no personal or family history of adenomatous polyps or colorectal cancer or other risk factors such as inflammatory bowel disease like ulcerative colitis or a genetic predisposition.
A colonoscopy is a procedure that uses a fiber-optic tube and air to examine the colon’s lining. Colonoscopy allows for the identification of polyps and their removal, or biopsy if the polyp is too large, at the same time as the procedure.
Depending on the findings during the procedure and individual risk factors, a colonoscopy may be repeated every year for high-risk individuals to a more typical range of 7 to 10 years.
For many, the worst part of a colonoscopy is the bowel prep, which is done at home the evening and morning before the procedure. The bowel prep cleans out the colon so it can be adequately examined during the colonoscopy. A good bowel prep is essential to getting a good colonoscopy as it helps the doctor detect and remove polyps more easily.
The colonoscopy itself doesn’t hurt. Patients are given sedating medication, which helps with discomfort, and many patients won’t remember having the procedure once it’s complete. Colonoscopy patients will need a friend or family member to drive them home after the procedure. Typically a patient will be able to eat and drink normally afterward.
Reach out to your physician or provider to talk about your risk factors. Discussing these factors in advance can help identify the most effective and appropriate screening test for you.
To Find a Doctor and their contact information click HERE — https://www.sheridanhospital.org/find-a-doctor/.

By Alexandria Poisel, Dietetic Intern at Sheridan Memorial Hospital
What is National Nutrition Month? Every March, this annual campaign invites people to learn more about making informed food choices and developing healthful eating and physical activity habits. This year’s theme is “FUEL FOR THE FUTURE.” The intention is to eat with sustainability in mind. What does that look like at Sheridan Memorial Hospital?
For us, it means buying local. The Sidewalk Cafe serves Manchester Street Coffee, roasted right here in Sheridan, Wyoming. What can you do at the hospital? Opt for a glass plate and metal silverware instead of Styrofoam to-go boxes if you eat in the cafeteria. Be aware of how much food you take, take what you will eat, and ask for a smaller portion if you need to. This can help cut down on food waste.
How can you “Fuel for the Future” at home? You can buy local! This is a great way to get high-quality products that are within the season, and it also supports the local economy, fueling the future of our town. Unsure where to start? Check out Landon’s Saturday Farmer’s Market for many local food vendors.
“Fuel for the Future” isn’t just about how we can take care of the Earth and our town, but also how we take care of ourselves for the future. Nutrition is a major component of a long and healthy life. It’s important to eat meals that have variety. Taste the rainbow! The colors of our foods are often associated with the different vitamins we need. The most colorful foods? Fruits and Vegetables. You should eat 2 cups of fruit and 2.5 cups of vegetables daily. Not everything has to be fresh; we know it is hard here! Frozen and canned fruits and vegetables are part of a healthful diet.
Pair your healthy eating habits with intentional activity. 150 minutes of exercise a week is recommended for adults. If you don’t enjoy the gym, don’t worry. There are many more options for you! Go for a walk with a friend, swim with your kids, try YouTube at-home yoga, or throw a dance party! Extra movement is good for strengthening bones, building muscle, and keeping your heart healthy.
How will you “Fuel for the Future?”
If you would like to schedule an appointment with one of our dietitians, please call 307.675.2640.
Note: Sheridan Memorial Hospital is committed to supporting the professional development of students and young professionals in our community. Experience in the form of an internship can be a fantastic way to apply knowledge and skills learned in the classroom, to expand on that knowledge, and to gain real-life experience in the healthcare industry. SMH is proud to provide this opportunity, helping educate more people in our community about each facet of the patient experience, and partnering with organizations to provide this experience in countless hospital departments.

Sheridan Memorial Hospital is excited to welcome Emily Denney, DO, to the Primary Care downtown practice at 61 South Gould Street. Dr. Denney is an Air Force veteran who made family practice her focus because she is passionate about working with people of all ages.
Dr. Denney’s desire to create lasting connections drew her to the medical profession: “I love talking with people, learning about them, and trying to help them live their healthiest lives.” After completing her degree in Texas and a residency in Maine, Dr. Denney joined the Air Force. She managed the healthcare of military personnel and their families at Dover Air Force Base, where she also mentored new clinicians.
Dr. Denney comes to Sheridan from a rural community in Montana, where she worked for over five years in a primary care practice. She was drawn to Sheridan in part because of her desire to continue working and serving in a small town. She feels the “supportive atmosphere and collegial environment” that SMH provides are essential to her success as a board-certified Family Medicine Physician.
When she isn’t working, Dr. Denney can be found spending time with her family; she enjoys reading, cooking, gardening, and getting outside with her husband and their two daughters, who are her “daily source of inspiration.” They are excited about all of the local recreation opportunities available and feel welcomed into Sheridan’s family-friendly atmosphere. “I want the people of Sheridan to know I love working with patients to meet their health goals, I am flexible in how we get there, and I am always learning new ways of doing things.”
Follow the respective link to learn more about Dr. Denney or the hospital’s Primary Care practice.

By Kristopher Schamber, MD, FACP – Medical Director, SMH Primary Care
Today we will be talking about gut health. The gut, or gastrointestinal (GI) tract, generally refers to the stomach, through the small and large intestines, and out the rectum and anus. I will include some discussion of the upper GI tract, or esophagus, as well.
I think it is important first to review some definitions. The term bowel refers to the intestines below the stomach. A bowel movement = poop. Stool = poop. Constipation, while different for everybody, signifies harder, less frequent bowel movements that require straining. Diarrhea, also different between individuals, signifies looser, more frequent bowel movements, typically very watery.
The perfect poop is soft but formed, comes out easily and does not leave any residue on your bottom or the toilet bowl. This is achieved with a healthy amount of dietary fiber, the type of fiber that does not get absorbed through your gut (like the stringy stuff in celery or the rind on an apple).
Constipation, while generally not severe, can cause significant illness, including severe pain, confusion, and even a ruptured colon, in addition to the more common hemorrhoids and diverticulosis. It may increase the risk of colon cancer as well. There are many different causes, including multiple medications, neurologic conditions, cancer, not drinking enough water, and poor diet. Treatment ideally targets the underlying cause. Increasing fiber intake, ideally with vegetables or using a fiber supplement, and drinking plenty of water (for most people, 64 ounces per day) is a must. Laxatives and stool softeners should only be used under the direction of your medical provider.
Diarrhea is generally less common than constipation and has a number of different causes, including infections, medications, tobacco, caffeine, alcohol and artificial sweeteners (Splenda, sweet and low, etc.). Treatment, as above, targets the underlying cause, and fiber can also help. Over-the-counter anti-diarrheals should be used under the direction of your medical provider.
Acid reflux, also known as GERD, typically causes stomach pain just below the breastbone, a burning sensation in the esophagus just beneath the breastbone, or an acid taste in the mouth with belching. It can rarely cause esophageal cancer. Common causes include a number of different foods: Acidic foods like tomatoes or citrus fruits, tomato-based sauces, and greasy and fatty foods. Coffee, alcohol, and tobacco are also common causes. Occasionally someone’s genetic makeup causes an increase in acid production.
Screening for colon cancer is an important part of GI health. A screening test is used to diagnose disease prior to it causing any symptoms. Colon cancer, if found early, can be cured. The screening begins between ages 45–50 and continues until at least age 75. A colonoscopy is the standard study in this community, though there are other tests as well that require a small stool sample.
Diet is very important to GI health, and as you read above, dietary factors play a role in many GI conditions. Generally speaking, a balanced diet with 25% whole grains, 25% healthy proteins (white meat, fish, legumes, etc.), 40% veggies with some fruit, and 10% healthy fats and oils (olive oil, avocado, etc.) is healthy for the gut, in addition to known benefits with the cardiovascular system, weight, and other benefits. As noted above, certain specific foods or beverages can contribute to constipation, diarrhea, or GERD. Diets heavy in smoked meats are linked to certain types of GI cancer.
Probiotics can also be helpful for gut health. Our intestines have good bacteria that help in digestion and other processes. This is known as the gut microbiome, and there is much ongoing research into various effects of this microbiome on the GI tract and throughout the body. Taking a probiotic daily can benefit your gut and the rest of your body with very little risk.
Learn more about Dr. Kristopher Schamber and Sheridan Memorial Hospital’s Primary Care practice and the professionals caring for patients by visiting the respective links.

Each year in February, we celebrate National Cardiac Rehabilitation Week to draw attention to the role of cardiac rehab in reducing the potentially devastating effects of heart disease. In Sheridan, we are lucky to have many exceptional services to support heart health, from the cardiology team at the Heart Center, to our Cardiac Catheterization Lab and state-of-the-art ICU at Sheridan Memorial Hospital. After having a heart attack, being diagnosed with heart failure, or after a heart procedure like a coronary artery bypass, coronary stent placement, or valve replacement, Sheridan Memorial Hospital’s nationally accredited Cardiopulmonary Rehab program provides support to help you recover.
 Just over a year ago, we told you about Tom McClain, who has been in the SMH Cardiopulmonary Rehab program since 2019. We thought we would check in on him and learned that he continues to participate in the maintenance program, now logging over 320 sessions over the last three years!
Just over a year ago, we told you about Tom McClain, who has been in the SMH Cardiopulmonary Rehab program since 2019. We thought we would check in on him and learned that he continues to participate in the maintenance program, now logging over 320 sessions over the last three years!
Tom says that since we last talked to him, he had cardiac ablation, a procedure to block his heart from producing irregular or abnormal rhythms, and also had his pacemaker replaced.
He is very grateful to have the program and the beautiful space to work out in. “This is a safe place for cardiac and pulmonary patients, and that’s why I come here. It makes me feel better, and it’s not hard to make myself come because there are people here who are expecting me. Coming to exercise here is just part of my weekly routine.”
He still considers himself one of our “regulars,” saying: “I come twice a week. Socialization is really important to me – there are three of us who come at the same time, and it makes exercising fun. We have a lot in common and encourage each other to do our best. I live alone and really look forward to spending time here.”
“What I particularly like about the hospital program is that there is always a nurse or staff member who monitors me – taking my blood pressure and checking my oxygen levels as I go about my workout. It’s comforting to have a professional on hand, observing me and making sure I’m doing ok. Besides that, I’m on oxygen, and it is so convenient that I can just plug my oxygen line into the wall as I exercise,” Tom adds.
He has also participated in the educational classes offered to patients in the Pulmonary Rehab program.
According to Cassie Mullins, RN, SMH Cardiopulmonary Rehab Supervisor, “Because our patients come so often, the Cardiopulmonary staff really gets to know each individual. A typical program runs from 18-36 sessions, so we learn a lot about our patients: their likes and dislikes, what they care about, and the goals they have. This also helps us develop a plan together with the patient, to reduce their risk of developing worsening heart disease. It can also help us provide continued encouragement for the individual to accomplish a health goal like quitting smoking. If our patients don’t show up, we call to check on them and encourage them to continue their workouts.”
Our Cardiac Rehab program has two phases. The first phase of cardiac rehab is the monitored exercise phase. During this time, your doctor can order up to 36 closely monitored exercise sessions for you to complete. We encourage our patients to work up to exercising 3 times a week with us. After graduating from the monitored exercise program, we encourage our patients to continue to exercise! During the maintenance phase, we provide the opportunity for our patients to continue exercising in our gym with less monitoring. The ultimate goal is for our patients to feel safe and confident participating in whatever kind of exercise they enjoy, whether in a cardiac rehab setting, at home, or in the community.
If you have had a heart attack, heart failure, or a heart procedure, ask your doctor if you could be eligible to be enrolled in cardiac rehab. For more information, call Cardiopulmonary Rehab at Sheridan Memorial Hospital at 307.672.1062.

by Kristi Ramsey, RN, BSN, RCIS, CVRN – Sheridan Memorial Hospital Cath Lab Manager
February is National Heart Month – so this is a particularly appropriate time to share some great news with all of you. Our Cardiac Cath Lab team has been working hard over the past year to achieve yet another national endorsement.
Cardiac Cath Lab Accreditation
I am pleased to announce that The American College of Cardiology (ACC) has recognized Sheridan Memorial Hospital (SMH) for its demonstrated expertise and commitment to treating patients who come to SMH’s Cardiac Cath Lab for care, including for diagnostic catheterizations (cath) and percutaneous coronary intervention (PCI) procedures. SMH was awarded Cardiac Cath Lab Accreditation with PCI based on rigorous onsite evaluation of the staff’s ability to evaluate, diagnose and treat patients who come to the cardiac cath lab.
PCI includes procedures such as PTCA, also known as Percutaneous Coronary Angioplasty, Thrombectomy, and Stent placement. It is a non-surgical procedure that opens narrowed or blocked coronary arteries with a balloon to relieve symptoms of heart disease or reduce heart damage during or after a heart attack. Thrombectomy is the removal of a thrombus (blood clot) from the coronary vessel. A coronary stent, a small expandable mesh-like tube, is often placed in the coronary artery once the narrowed or blocked artery is opened. The stent keeps the artery open and allows blood to flow freely to the cardiac muscle.
Cathy Bealer, SMH Chief Nursing Officer says, “In earning this accreditation, our Cath Lab staff and providers have demonstrated their commitment to providing the Sheridan region with consistent excellent heart care. They completed a multi-faceted clinical process that culminated in a rigorous onsite review. They also applied improved methods and strategies of caring for patients, including streamlining processes, implementing quality cardiovascular guidelines and standards, and adopting best practices in caring for cath lab patients.”
She adds, “Because of our team’s diligent work, our patients here in Sheridan have access to the same heart testing and treatment typically found only in regional medical centers.”
According to the ACC, facilities that achieve accreditation meet or exceed stringent criteria and have organized a team of doctors, nurses, clinicians, and other administrative staff that earnestly support the efforts leading to improved patient outcomes. To maintain the accreditation, hospitals must undergo the review process every three years.
Hospitals that have proven exceptional competency in treating patients requiring cardiac catheterization have standardized their assessment process for patients before catheterization to ensure quality and patient safety. They ensure that care in the procedure room for sedation, infection control, radiation safety, universal protocol, and time-out procedures is fully coordinated; and have mastered the appropriate transfer to a cardiac recovery department to better monitor and track complications, enhance physician-to-patient communication, patient family communication, discharge instructions and follow-up information.
Heart Failure Accreditation earned in 2020
This isn’t the first national accreditation that our Cath Lab has earned. Back in 2020, the ACC awarded SMH the Heart Failure Accreditation, which was based on the hospital’s competence and specific standards that were put in place to provide excellent care to patients with heart failure. The ACC evaluated 73 mandatory components that focus on the hospital’s policies, standards, protocols and education related to heart failure. This was also a three-year accreditation which was renewed again this past year.
Earning these recognitions is not a “one-and-done” process, and both require ongoing internal attention to how we care for members of our community who have heart disease. It’s a constant rigorous look at policies, protocols, and standards and making the appropriate adjustments needed to evolve with the continuous changes and improvements in the care of our cardiac patients.
Thanks to our entire Cardiovascular team for their dedicated focus, extra hours, teamwork and collaboration to achieve both of these outstanding recognitions. All of this means better outcomes for our patients.
In addition to the mentioned procedures in this article, the following procedures are also performed in the cardiac cath lab.
Cardiac Cath Lab History at SMH
The SMH Cardiac Cath Lab opened in 2013 and is one of only seven in the state of Wyoming. It was funded through the SMH Foundation – with a significant gift from the Lorraine Husman Trust, designated for cardiac care, and a generous donation from the Sheridan Memorial Hospital Auxiliary.

2023 Sheridan Memorial Hospital Cath Lab Team
Left to right: Yvette Romero RN, Chris Rojo RN, Jackie Ek RN, Lauryn Cleveland RTR,
Kristi Ramsey RN, Dawn Morgan RN, Matt Elmore RTR, Megan Wetzel RN.
Missing from Photo: Alaina Sottolano RN, James Boulter RTR, Marcus Pedroza RTR
To learn more about awards Sheridan Memorial Hospital has earned, click HERE or visit https://www.sheridanhospital.org/about-us/awards/.

By Cassidy Camino, Sheridan Memorial Hospital Trauma RN
According to the CDC:
In our community, the most common causes of injury for 65 and older are injuries from falls – falling is not a normal part of aging. Per the Sheridan Memorial Hospital (SMH) trauma statistics, from November 2021 to November 2022, 125 of the 138 patients in this age group sustained injuries from falling that were significant enough for hospital admission or transfer to a larger trauma center. Sixty-two of those resulted in hip fractures, and 15 resulted in head injuries.
Seniors are at an increased risk for many types of injuries due to advancing age and decreasing health. As we age, our eyesight, hearing, and reflexes might not be as sharp as they were when we were younger. Certain conditions, such as diabetes, heart disease, or problems with your thyroid, nerves, feet, or blood vessels, can affect your balance and lead to a fall. Certain medications can cause you to feel light-headed and dizzy. Review your medications with your provider.
Falling once increases the chances of falling again. Many people who fall develop a fear of falling again, and this fear causes them to be less active. Being less active causes increased weakness and raises the chance of falling again. This is why it is vital for seniors to keep moving. Many types of exercises or movements can help develop better muscle tone to improve balance and gait.
Many people believe that falls are an inevitable part of aging. However, this is not true, and many falls can be prevented by being aware of hazards and taking some simple steps to correct them. Below are some tips to prevent falls in and out of the home.
Remove home hazards:
Staying safe in our Wyoming Weather:
If you believe you might not be able to get up on your own after a fall, an emergency call system would be highly beneficial. This system enables you to push a button on a special necklace or bracelet to call for help. Some smartwatches also have this feature. Contact your physician for more information.
Injuries among this age group can have devastating consequences, in some cases leading to disability, loss of independence and death. Preventing injuries is the easiest way to protect your health and promote successful aging.
Click here to learn more about Emergency Services at Sheridan Memorial Hospital.
When an older adult falls, they may not be able to get up on their own resulting in laying on the floor for a period of time. In this situation, serious complications can develop such as dehydration, hypothermia, pressure sores and pneumonia.
It is important to know what to do after a fall. Below are some steps to help.
If you are NOT Injured
If you ARE Injured
If you believe that you might not be able to get up on your own after a fall, an emergency call system would be highly beneficial. Having these systems enable you to push a button on a special necklace or bracelet to call for help. Some smartwatches also have this feature. Contact your physician for more information.
After a fall without significant injury, it is common for people to not tell their physician about these incidents. Sometimes, there are underlying causes that could be addressed with treatment or correction, so it’s best to keep your physician in the loop. It may also help to learn more about preventing falls because older adults who’ve fallen once are at greater risk of falling again in the future.
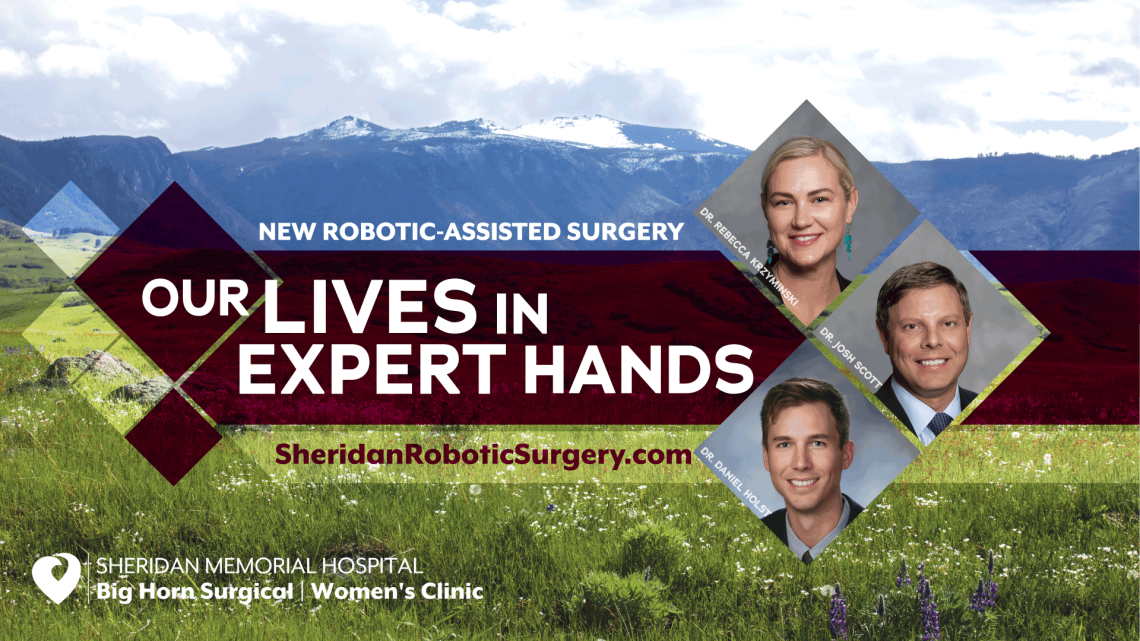
Patients can now access state-of-the-art, minimally invasive surgical technology right here in Sheridan. The new da Vinci Xi Robot-Assisted Surgical System at Sheridan Memorial Hospital provides overall better outcomes. Patients experience shorter hospital stays, reduced recovery time, reduced pain/discomfort, reduced scarring, and reduced blood loss. The da Vinci system is designed to be the safest and least invasive option for many surgical interventions. This is the fourth generation of the da Vinci robotic platform and it brings with it over 20 years of learning for enhancing surgical performance.
Dr. Josh Scott recently moved back home to Sheridan and is a surgeon with Big Horn Surgical at SMH. He says patients should be excited about the capabilities of this new system and what it means for them post-surgery.
“As surgeons, we will be able to conduct even less invasive surgeries because this new robot only requires two to four incisions between eight to 13 millimeters long,” Scott says. “Pair that with the post-surgery benefits of shorter hospital stays and reduced recovery time, and it’s a win-win situation for patients. To have this level of technology here in Sheridan is amazing.”
There are many types of surgery that can be performed using this surgical system according to Dr. Scott. Some of those include hernia repair, gall bladder removal, hysterectomies, ovary removal, prostatectomies, and more.
“As our many specialists become more familiar with this technology, other surgical options will become available in the near future,” Dr. Scott added.
While the robot is what makes this surgery less invasive, Dr. Scott went on to say, “It’s very important for patients to know the surgeon is in control of the robot at all times. The robot does nothing without the surgeon directing every movement of the instruments.”
The surgeon uses a console right at the bedside to control the precision instruments with a 3D, high definition camera with 10x magnification allowing access to hard-to-reach areas of the body not normally visible to the human eye.
“This robot will allow our patients to remain closer to home, family and friends and that always provides a better healing environment after surgery,” Dr. Scott added.
To learn more about the New Robotic-Assisted Surgery Program at Sheridan Memorial Hospital visit SheridanRoboticSurgery.com and Robotic-Assisted Surgery FAQs

SMH Awarded $5.9 Million State Grant to Enhance Mental Healthcare in Sheridan County – Hospital to launch capital campaign to raise matching funds for $12.8 Million Project
On November 16, Sheridan Memorial Hospital (SMH) was awarded a $5.9 million grant from the State Land and Investment Board to develop an Emergency Psychiatric Assessment, Treatment, Healing (EmPATH) and Crisis Stabilization Unit to serve the Sheridan County region.
This critical project will help address the growing mental health and behavioral health needs of our community by providing psychiatric urgent care, crisis stabilization, inpatient psychiatric beds, and therapy space. The total cost of the project is $12.8 million and the SLIB grant requires a one-to-one match.
Over the years SMH has invested heavily to provide a safe environment for behavioral health patients and staff. Currently, the hospital provides tele-psych services, security on-site 24 hours/day, patient support staff, additional full-time licensed clinical mental health professionals, and transportation to get patients to appropriate treatment facilities.
The region does not, however, have the appropriate level of treatment and service for behavioral health patients to meet their needs close to home. Many patients must be transported to treatment facilities far outside our community. The development of the EmPATH and Crisis Stabilization Unit is an opportunity to invest in facilities that will support the mental and behavioral health needs here in Sheridan County.
Sheridan Memorial Hospital’s Chief Executive Officer, Mike McCafferty, expressed his gratitude to everyone who’s working on improving mental health in our community. “Addressing the mental and behavioral healthcare needs of our community is a priority for Sheridan Memorial Hospital. We are grateful to our local, regional, and statewide partners who are working with us to provide additional mental and behavioral health care resources that our community deserves.”
Sheridan Memorial Hospital partnered with local, regional and statewide stakeholders to develop its plan to enhance community partnerships addressing mental health care needs for our region. The hospital looks forward to working with partners, foundations, and community members in making this critical project for our community a reality.
This project will launch quickly as the SLIB grant designates that it must be completed by 2026.
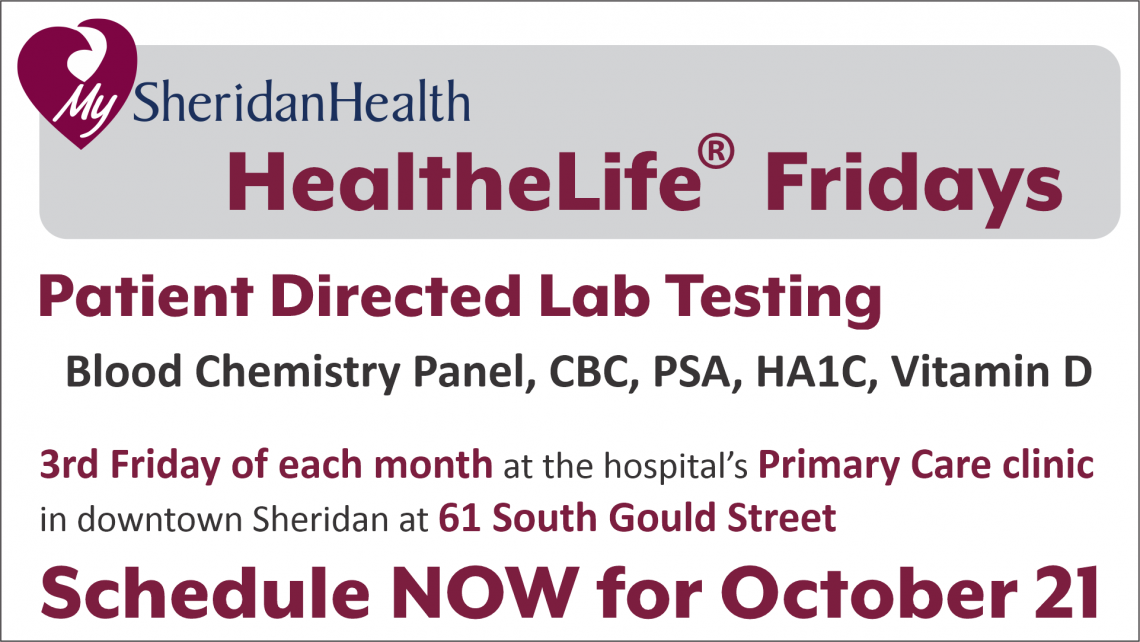
This Friday, October 21, Sheridan Memorial Hospital (SMH) launches an expanded preventative health care program called HealtheLife® Fridays. The new program begins with wellness blood screenings, now called Patient Directed Lab Testing. The preventative panels – which do not require a physician order – include a Blood Chemistry Panel, CBC, PSA, HA1C and Vitamin D.
Andrea Paulson, SMH Laboratory Manager, says HealtheLife Fridays at Primary Care’s downtown location will be good for the community; “Moving our Patient Directed Lab Testing downtown and providing it once a month will streamline things for our patients. Our lab phlebotomists will conduct the blood draws in the spacious conference room and there is ample parking in the hospital’s lot across Gould Street.”
HealtheLife® Fridays will be offered on the 3rd Friday of each month at Sheridan Memorial Hospital’s Primary Care clinic located at 61 South Gould Street in downtown Sheridan. Tyler Crossley, SMH Primary Care Manager, says, “This new service is a way for us to bring exciting new preventative health opportunities to our community. At future HealtheLife Fridays, we look forward to offering more tests, screenings, and education – much like a traditional health fair.”
Online scheduling for this new program allows patients to schedule up to 3 months in advance. Patients may schedule appointments from 6:30 am to 11:30 am via the hospital’s website: sheridanhospital.org. Or patients may leave a message requesting an appointment at 675-4675. Hospital staff will return calls to schedule an appointment date and time.
Sign up for your Patient Directed Lab Tests by clicking HERE.

With October often comes the colors changing not only on the grass and trees, but pink is often around every corner you turn. This year marks the 14th Annual Link Partners in Pink for the Sheridan Memorial Hospital Foundation and our community. It was a hugely successful event with hundreds of participants, volunteers and cancer survivors in attendance. This year’s funds raised will go toward the Comfort Care Program at Sheridan Memorial Hospital’s Welch Cancer Center (WCC). These funds are available to cancer patients of all cancer types and providing them with the most comfortable experience during their cancer journey. But what exactly is comfort care and how does it provide needed resources to your neighbors, patients, and family?
Sheridan Memorial Hospital’s Welch Cancer Center Comfort Care Program began with a few gifts to support the journey of cancer patients through their diagnosis and treatment. Now, through thoughtful and generous donations and memorials, Comfort Care provides this needed funding based on criteria set and the patient’s financial needs. These one-time grants enable the WCC team to help our patients and their families on a personal level. Grants may also be used to help with travel expenses associated with unexpected treatments or to aid patients in the region to travel to Sheridan for their necessary treatments. Our patients and staff are grateful for the funds as they cover numerous other resources, support programs, and other comfort-related items, including individual counseling.
Throughout the last year, these funds have provided:
It is a gift to be able to support this pivotal part of care and healing for some of the most vulnerable patients in our community.
For more information about the WCC’s Patient Comfort Care please contact the Welch Cancer Center at 307.674.6022.
To make a donation to the WCC Patient Comfort Care Program or other vital healthcare programs, please call The Foundation at 307.673.2418.