Our volunteers and community members turned out to celebrate the Sheridan Memorial Hospital Auxiliary’s 62nd annual 5-Year-Old Birthday Party!
With hunting season upon us, the Trauma Team at Sheridan Memorial Hospital provides these tips for Gun Safety.
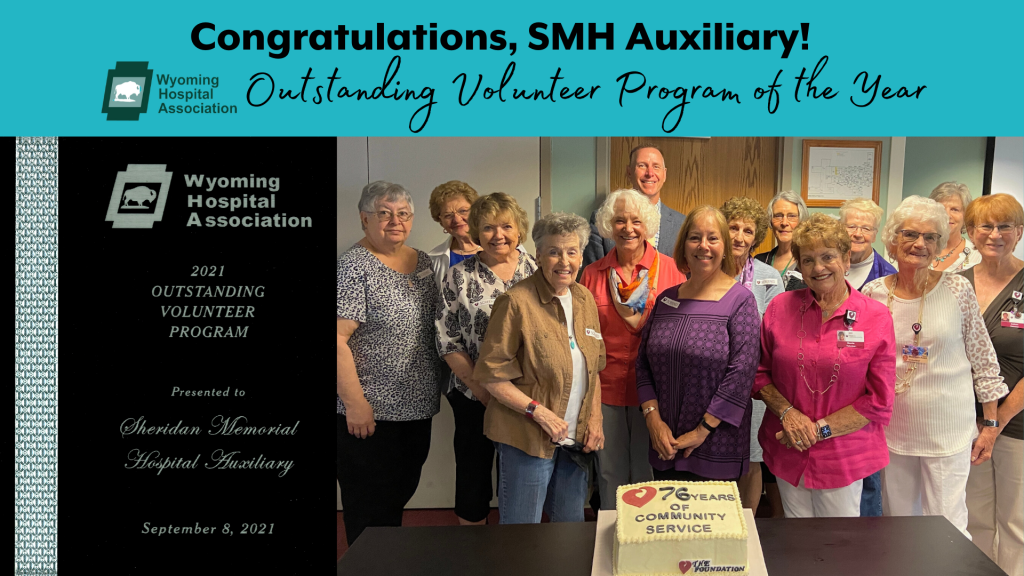
Many times we’re asked who The Sheridan Memorial Hospital Auxiliary is? Below you’re going to read countless things they accomplish
The Sheridan Memorial Hospital Foundation looks forward to its 13th Annual Link - Partners in Pink
More than one out of four older adults fall each year. These falls are NOT a normal part of aging and are serious and costly, causing broken bones
We know how important you are in the healing of your loved one. The following guide is intended to
Stacy Windon was a recent patient in Sheridan Memorial Hospital. Below is her experience in her own words.
With school starting, It is extremely important to take proper safety precautions when transporting your children to and from school.
A first-hand account from recent Urgent Care patient, Janet Dale: My recent experience at the Urgent Care at Sheridan Memorial Hospital was a
The CDC is now recommending a third COVID-19 vaccine dose for certain patients with
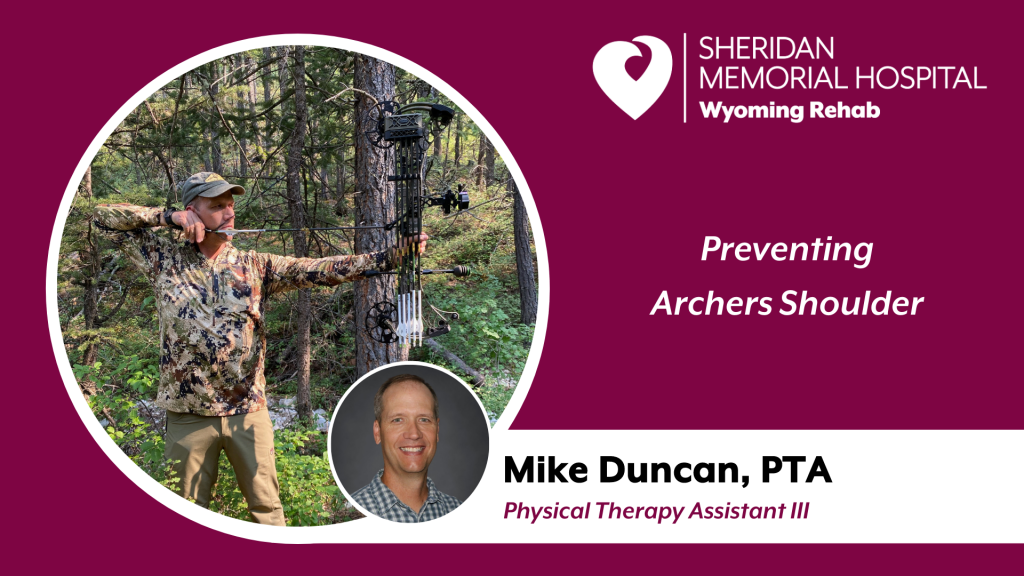
The fall season is rapidly approaching and for many Wyoming residents, that means hunting season. Hunting with archery equipment
The Sheridan Memorial Hospital Foundation Staff and Board of Directors are pleased to welcome Sue Belish, the newest Foundation Board Director.
Trouble hearing? Learn about our new audiology services and what options might be available to help you.
Holly Zajic (pronounced Zeitz) loves helping people be the best they can be every day. When you first meet her, it’s the exuberance and energy
How does a bachelor’s degree in Fisheries Biology end up landing you a job in the housekeeping department of your local hospital and ultimately
The Foundation’s successful Clinical Educational Endowment was initiated in 2003 with private donations. Annually it provides nursing
Urgent Care physician, Dr. David Nickerson, offers up these keys to preventing heat stroke and heat
Vera Olson was suffering from more than illness when first admitted into the Transitional Care Unit
On Friday, July 2, over 100 golfers and hospital volunteers gathered at The Powder Horn Golf Club to raise awareness and funds for patient
Sheridan Memorial Hospital’s (SMH’s) Transitional Care Unit (TCU) is a hospital-based short-term