Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
Health and Wellness

These photographs of our SMH Team Members were taken prior to the required use of social distancing and masks.
Federal, state, and local leaders as well as leaders in the healthcare industry have been asking a lot from our citizens during this outbreak of COVID-19… and the latest results are showing some positive movement in flattening the curve of COVID infections over the past few weeks in Sheridan County and Wyoming. This is all due to the diligence of our community members to socially distance themselves and follow the guidelines that have been put forth to slow the spread of this virus.
While this positive trend is amazing to see, it is important that we maintain our efforts. Don’t let up now. We can all stay vigilant and do our part to make a difference. The staff at Sheridan Memorial Hospital join essential workers across the country and throughout the world in requesting all nonessential personnel stay home to help keep our community safe.
Communities around the world are facing extreme circumstances and ranges of emotion as we experience the realities of COVID-19. Many of us turn to the news to compare reports and statistics of each state and the impacts of the virus around us. We wonder how long we will need to stay home and keep social distancing. How long will we need to find things to keep us occupied and our minds off the uncertainty around us?
We may be trying movie marathons, making new recipes, and reading books that have been collecting dust on shelves. We are embracing technology, education, and each other. We continue to wave at each other from our cars, to enjoy FaceTime calls and Zoom family reunions. Our community will find the silver lining in this situation, wherever we can.
Tomorrow, and in the days to come, we ask our community to continue to stay home and make every effort to socially distance ourselves. Sheridan Memorial Hospital healthcare workers – your neighbors, family, and friends – thank you for your continued effort to keep our community healthy.

This month’s W.O.W Employee of the Month is Welch Cancer Center Pharmacist, Sarah Opitz. As a mom to three young girls, Sarah was motivated by her family to start her wellness journey.
“Family is huge for me. I wanted to set a good example for my family and show them what it looks like to maintain overall good health,” said Opitz. “I wanted to be active, exercise, and maintain a healthy weight so that I can be there for them.”
A few months ago, Sarah was motivated to make positive changes after experiencing what many mothers go through after nursing.
“Having young girls, I was nursing for a long time, and I used it to justify eating whatever I wanted because I could do it without gaining weight. Now that stage is over and I realized very quickly that my clothes were fitting tighter,” said Opitz. “Once I noticed I was putting on a few pounds I realized I needed to be more conscious of what I was eating and that I needed to be more active. Once I realized I could do better and should be better, I started to make a few changes.”
Sarah started by making small changes, including exercising and monitoring her portions.
“It wasn’t big and I didn’t really change my diet, I just started being more conscious of the amount I was eating. I also started going to the gym more often,” said Opitz.
She started making sure she had veggies and fruits with meals and paying attention to what was going on her plate.
Before she started making changes, Sarah relied on the activity she got around the house and with her family. She started by creating an exercise routine that fit her schedule.
“I had to find times in my schedule that would work for me. I go to the gym on weekends and Wednesday mornings when my girls are at daycare,” said Opitz.
After she started making time for the gym she started noticing the positive benefits of exercise.
“It helps my mood and my energy, it definitely perks me up,” said Opitz.
Like many others, Sarah’s wellness routine has been interrupted by COVID-19, but she’s found ways to adapt.
“Looking on the bright side, we know that Spring is just around the corner. With the warmer weather we can spend more time outside doing things,” said Opitz. “You’re supposed to stay at home, but that doesn’t mean you have to stay in your house. Bryan, the girls, and I have been able to get out a lot, going for walks, bike rides, and taking the girls on their scooters.”
When asked what advice she would give to others starting their wellness journey she discussed the importance of making time for yourself and simple changes.
“My advice would be that if you’re feeling overwhelmed, or you want things to be better, or you need more structure, just stop and think about simple changes you can make. Find a few minutes to relax or go to the gym,” said Opitz. “The hardest thing for me was just deciding to do it and start. Once I made the choice to start doing it, I found it wasn’t as hard as I thought.”
Sarah uses the MyFitnessPal app to log what she eats and to calorie count. The app has helped her keep her wellness routine.
“Just taking the time to do those entries was daunting. I use the MyFitnessPal app because it’s user-friendly, quick, and slick. It helps make time not a factor. The thought of having to make a change was difficult. “I like routine and liked the way things were so I was lax and I ate whatever and did whatever. I didn’t have a routine and I needed one,” said Opitz
“I have to make sure that I have time for myself, even if it’s just a few minutes, it helps me relax,” said Opitz. “I really enjoy reading but since we had kids time is short and hobbies have fallen by the wayside. I’ve made time to read again and I also read with my daughter before she goes to bed and I really enjoy it.”
As a mom, Sarah knows the impact of making time for yourself and the benefits that a healthy lifestyle can have.
“These changes haven’t made me the perfect mom but they have definitely helped,” said Opitz. “I still struggle with the everyday challenges of being a mom, but it has helped and I can tell a difference.”

March is National Nutrition Month and a great opportunity to recognize our incredible Registered Dietician Nutritionists at Sheridan Memorial Hospital. Our RNDs are experts in food and nutrition and are qualified to support a variety of patient needs including meal planning, nutritional counseling, assessments, progress tracking and much more. To learn about the common reasons to consult an RND, check out the link below:
If you’re interested in seeking the expert, science-based advice of our RNDs, contact your primary physician for a referral today.
On March 11th we celebrated Registered Dietitian Nutritionist Day and we were able to learn some fun facts about each of our RNDs. Get to know them below!
Jordan McCoy MS, RDN, LD (Outpatient/Dialysis Dietitian)
Q: Favorite way to spend a Saturday afternoon?
A: Fly fishing on either the Big Horn River (MT or Thermopolis) or the North Platte with Trinity, my
Boyfriend.
Q: What was the last thing you took a photo of?
A: A rainbow trout at the North Platte in Casper.
Q: Does pineapple belong on pizza?
A: Of course….as long as there is lots of cheese to go with it.
Q: Favorite pie?
A: No pie, only cake!
Q: Summer, Winter, Spring or Fall?
A: OHHH hard to pick! How about SUMMALL a mix of Summer and Fall.
Q: Morning person or night person?
A: Morning! Bring on 4 a.m.
Megan Sexton MS, RDN, LD (Clinical Dietitian)
Q: Favorite way to spend a Saturday afternoon?
A: Hiking in the Big Horns with my two fur-babies.
Q: What was the last thing you took a photo of?
A: The walk-in shower we just remodeled ourselves.
Q: Does pineapple belong on pizza?
A: Absolutely not! No warm fruit for me.
Q: Favorite pie?
A: Doesn’t really matter, I’m in it for the crust.
Q: Summer, Winter, Spring or Fall?
A: Fall for all the hiking, fishing, hunting, and crisp air I can get.
Q: Morning person or night person?
A: Morning, my bedtime keeps getting earlier.
Sarah Sommers RDN, CDE, LD (Outpatient Dietitian/Diabetes Education Coordinator)
Q: Favorite way to spend a Saturday afternoon?
A: Cross country skiing in the Winter or canoeing the Tongue River in the Summer.
Q: What was the last thing you took a photo of?
A: A snow-covered landscape with the Bighorns in the background.
Q: Does pineapple belong on pizza?
A: The more veggies on the pizza the better…but I don’t want fruit on my pizza.
Q: Favorite pie?
A: Do brownies count?
Q: Summer, Winter, Spring or Fall?
A: Definitely Winter – I love the crisp cool mornings and the snow! But ask me in the Fall and I might say then too.
Q: Morning person or night person?
A: Morning without a doubt.
Sheridan Memorial Hospital is very proud of our RNDs and the amazing work that they do to provide our community with excellent patient-centered care.

This month’s W.O.W Employee of the Month is Wyoming Rehab Physical Therapist, Darrin Goyn. Wellness has been a part of Darrin’s life from a young age and running was and continues to be, one of his favorite activities.
“I grew up outside of town and we would ride bikes all over the place. My two older brothers had bikes and for whatever reason, I didn’t have one so the only way I got to go with them was to run. I think that’s where I got my start in running,” said Goyn.
Darrin was involved in athletics throughout school including track, cross country, and wrestling. He also had the opportunity to compete in track at the college level but decided not to. After high school, he still enjoyed running and continued to do it throughout his life for leisure as well as competing in races.
“I started out with 5ks, then 10ks, and then a few half marathons. I’ve never done a full marathon. In the last 4 – 5 years I started doing trail running which I enjoy a lot more and the trails are easier on my legs,” said Goyn. “I’ve done the Big Horn Trail run: the 18 mile and the 52 mile. I trained a while for it and everything went well and I enjoyed it.”
Outside of running, Darrin enjoys woodworking, remodeling homes, and gardening with his wife. It’s also important for him to stay active at home and he’s not someone who can’t sit for very long. Along with staying active, he also prioritizes a healthy diet.
“My biggest motivation is general health and stress reduction. I just eat a healthy well-balanced diet. I try to eat more fresh food, watch the sugars and the carbs, but I still indulge. Just a good overall general healthy diet. My wife is a good cook so that helps,” said Goyn. “My wife and I both eat wild game so we don’t buy a whole lot of other meat because we know how it’s processed. We do a lot of fresh vegetables and fruits and don’t buy too many canned items.”
The advice he would give to others who are ready to make lifestyle changes is to focus on consistency and to know your limitations.
“The biggest part for anyone is the consistency of doing it. We’re all creatures of habit that have a tendency of getting out of the habits that we have worked to get into. The consistency of stressing the body and making sure you’re not injured is important to maintain a general fitness level and staying active,” said Goyn.
He also emphasizes the importance of eating a healthy diet and avoiding certain foods.
“Number one: stay away from fast-food restaurants and avoid eating out too much. Especially when you’re going out and spending money, you feel like, oh I have to eat all of this because I bought it,” said Goyn. “Focus on quantity and portion control and avoid carbonated drinks as much as you can. Just focus on eating fresh food and good lean meats.”

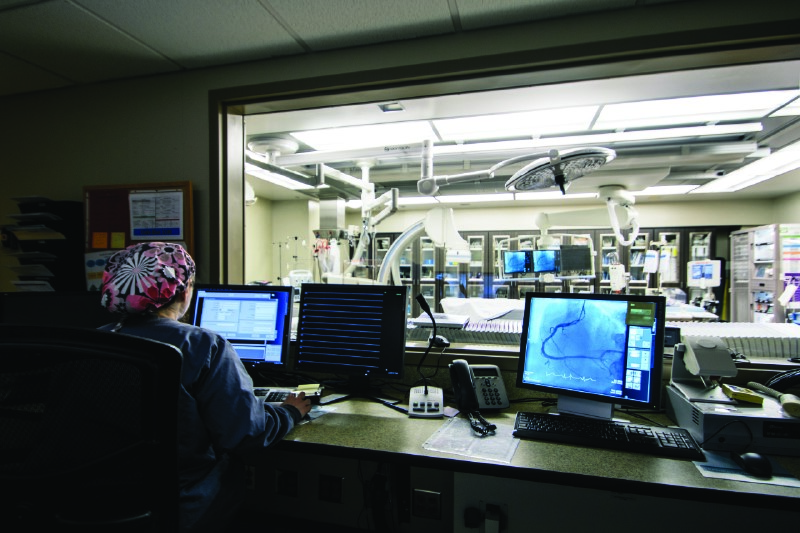
By Cassie Mullins, RN Cardiopulmonary Rehab Supervisor at Sheridan Memorial Hospital
In Sheridan, we are lucky to have many services to support heart health, from the cardiology team at the Heart Center, to our Cardiac Catheterization Lab and state of the art ICU at Sheridan Memorial Hospital. After having a heart attack, being diagnosed with heart failure, or after a heart procedure like a coronary artery bypass, coronary stent placement, or valve replacement, Sheridan Memorial Hospital’s nationally accredited Cardiopulmonary Rehab program provides support to help you recover.
According to the Centers for Disease Control and Prevention, someone has a heart attack every 40 seconds in the United States, and heart failure was a contributing cause of 1 in 8 deaths in 2017. After a major cardiac event, many are scared or uncertain of what to do to get themselves back on track. This fear and uncertainly can come from both being told something went wrong with your heart and from trying to learn a whole new set of “rules” to follow. New foods, new medications, new appointments, and new recommendations regarding physical activity can lead some to feel overwhelmed and underprepared for living a healthy life as a heart disease survivor.
Cardiac rehab plays a huge role in reducing the potentially devastating effects of heart disease. It is here that patients are given guidance and structure to help develop the necessary skills to face their new reality.
In cardiac rehab patients see other people like themselves exercising, socializing, and learning how to manage their heart disease with help from nurses, pharmacists, and dietitians. The foundation of cardiac rehab is physical activity. We monitor your heart rate and rhythm with a heart monitor that you wear during exercise, and check your vital signs before, during and after exercise. This information ensures that staff has the ability to see how your heart is reacting to physical activity in real-time. We work with patients to encourage a slow and safe increase in physical activity. In addition to exercise, at Sheridan Memorial Hospital’s Cardiac Rehab program we also provide education on cardiac disease, exercise safety, a heart-healthy diet, stress management, and medications.
Cardiac rehabilitation is recommended by the American Heart Association and covered by Medicare and many insurance companies. Studies have shown that participating in cardiac rehab substantially reduces the risk of death for individuals who have received a qualifying diagnosis or cardiac procedure. People who attend cardiac rehab programs live longer, are less likely to have a heart attack, and are less likely to be hospitalized. Yet most eligible patients don’t participate at all, let alone complete the recommended number of sessions.
Cardiac rehab has three phases. The first phase is the time immediately after a heart attack or procedure. The second phase is the monitored exercise phase. During this time your doctor can order 18, 24, or 36 closely monitored exercise sessions for you to complete. We encourage our patients to work up to exercising 3 times a week with us. After graduating from the second phase, we encourage our patients to continue to exercise! During the third phase, we provide the opportunity for our patients to continue exercising in our gym with less monitoring. The ultimate goal is for our patients to feel safe and confident participating in whatever kind of exercise they enjoy doing, whether that is in a cardiac rehab setting, at home, or in the community.
If you have had a heart attack, heart failure, or a heart procedure, ask your doctor if you could be eligible to be enrolled in cardiac rehab. For more information call Cardiopulmonary Rehab at Sheridan Memorial Hospital (307) 672-1062.

By Megan Sexton, RND
Which came first: the junk food or the memory decline? This question is being investigated currently by researchers and has revealed a strong correlation between a diet high in sugar and saturated fat with decreased memory function. The mounting evidence points to the significant impact a Western pattern diet likely has on the neurocognitive functions of our hippocampus (a small region in the brain). Our hippocampus is thought to be the control center that regulates motivation, emotion, learning, and memory. Bottom line: as saturated fat and sugar increase presence in a person’s diet, memory function declines.
The term Western pattern diet has been used interchangeably with the standard American diet and is defined as a high intake of red meat, processed meat, pre-packed foods, fried foods, high-fat dairy, refined grains, high-fructose corn syrup, and high-sugar beverages. Additionally, as these food-types increase, the amount of whole fruits, vegetables, fish, legumes and whole grains consumed decreases. Consuming a standard American diet carries other proven complications such as the increased risk for diabetes, heart disease, stroke, constipation, and weight gain. In other words, the evidence for people of all ages to move away from a standard American diet is very compelling and has been long-standing. But the rapidly growing evidence for the negative impacts of an American diet on memory function should make older adults prioritize evaluating their personal diet.
When I ask older adults why they depend on pre-packaged foods, fast-foods, and convenience foods for the majority of food choices, several explanations emerge. The decrease in energy and mobility, flavor and texture changes, dental issues, income restraints, and emotional life events (such as moving homes or loss of partner/loved-one) are the most common reasons. While these are valid reasons to seek out ways to ease the burden of food choice, we can’t ignore the probable impact these foods are having on memory decline.
There are several ideas that can be implemented to help consume high-quality foods for older adults. Sheridan has wonderful resources in Meals-on-Wheels and Designing Dinners that offer homemade meals that can be brought home for reheating. Grocery discount days, grocery delivery and a variety of grocery price-points all help to alleviate some of the cost burdens. I also encourage older adults to think outside of the box; quality food items don’t have to be combined into a whole meal to be beneficial. Having nutritious foods that require minimal assembly can make up the bulk of your calorie intake. Foods such as eggs, packaged tuna or salmon, low-fat cottage cheese, low-fat cheese sticks, low-fat Greek yogurt, hummus, nut butters without added sugar, mixed nuts, microwaveable frozen vegetables, low-sodium canned beans, sunflower and pumpkin seeds, whole-grain bread, microwaveable brown rice, and more.
The social and emotional aspects of mealtimes need to be addressed as well. Older adults have experienced significant changes to where and with whom they dine, and when these changes happen, the effort of grocery shopping, meal planning, and meal preparation can often be extremely daunting. My suggestion: don’t force old habits. Instead, attempt to establish new routines, keep nutritious snacks nearby and keep yourself on a schedule that includes sleep, activity, socialization, and eating. It can be helpful to reach out to various friends/family for reoccurring group meals, attending a community lunch, or rethinking the size and frequency of your in-home meals.
The aging process is difficult for numerous reasons, and to this point, I think we ought to arm ourselves with as much research-based knowledge as possible. While the research is concerning for the standard American diet and memory decline, it also informs us of some nutrition habits that can directly be addressed. Use the resources in our community and in your personal life to decrease the saturated fat and sugar you consume, by reducing the amount of pre-packaged foods, fast-foods, and convenience foods. Your brain will thank you.

Sara Smith Maguire, M.D. FACS
It may not be the most glamorous subject, but talking about colorectal cancer saves lives. Among cancers affecting both men and women, it is the second leading cause of cancer-related death in the US. Unlike many cancers, we have effective tools to help decrease the development of colorectal cancer and identify its presence at an earlier stage.
The risk of colorectal cancer increases with age, with more than 90% of the cases we see being diagnosed in people age 50 or older. There are many factors that are associated with an increased risk of colorectal cancer. Some of these risk factors are related to lifestyle choices and are therefore modifiable. Maintaining a healthy weight, being physically active, not using tobacco, avoiding heavy alcohol intake and eating a balanced diet that limits intake of red or processed meat can all help decrease your risk. Some risk factors can’t be changed; these include increasing age, a family history of colon cancer, inflammatory bowel diseases and belonging to certain ethnic groups.
Colorectal cancer may cause symptoms as it grows. These symptoms include seeing blood in or on your stool, unintentional weight loss, a change in bowel habits and weakness or fatigue caused by a low blood count.
Screening is the practice of looking for cancer or pre-cancer in individuals without symptoms. Screening is incredibly effective when it comes to colorectal cancer because, from the time the first abnormal cells start to develop, it takes on average 10-15 years for those cells to become cancer. Screening is one of our most effective tools for preventing colorectal cancer because it allows us to identify precancerous polyps and identify small cancers that aren’t yet big enough to produce symptoms.
There are several screening tools for colorectal cancer, including colonoscopy which allows us to both find polyps and remove them. Talking to your doctor about your risk factors can help identify the most effective and appropriate screening test for you. In general, screening is recommended between the ages of 50 and 75, though there are reasons to start earlier or stop later for some people. Every year, about 140,000 people in the US will be diagnosed with colorectal cancer and 50,000 people will die from it. Our best tool to decrease both of these numbers is screening. Talk to your doctor today.

February is American Heart Month and there’s no better time to learn about women’s heart health. Heart Disease is the number one killer of women causing more deaths than cancer, including breast cancer. Heart Disease is on the rise in Wyoming and throughout the country.
Sheridan Memorial Hospital invites you to join us on Tuesday, February 18th at 12:00 pm in the Community Conference Room located at 61 S Gould St, for our Health Talk on Women and Cardiovascular Disease. Enjoy lunch on us and learn from SMH Heart Failure Coordinator, Kristi Ramsey BSN, RCIS, CVRN on how Heart Disease affects women in Wyoming and the United States.
At the Health Talk you’ll learn about the common signs and symptoms of different kinds of Heart Disease and how to spot them. You’ll also learn how to optimize heart health and what treatment options are available.
This February protect your heart and join us for our Health Talk: Women and Cardiovascular Disease.
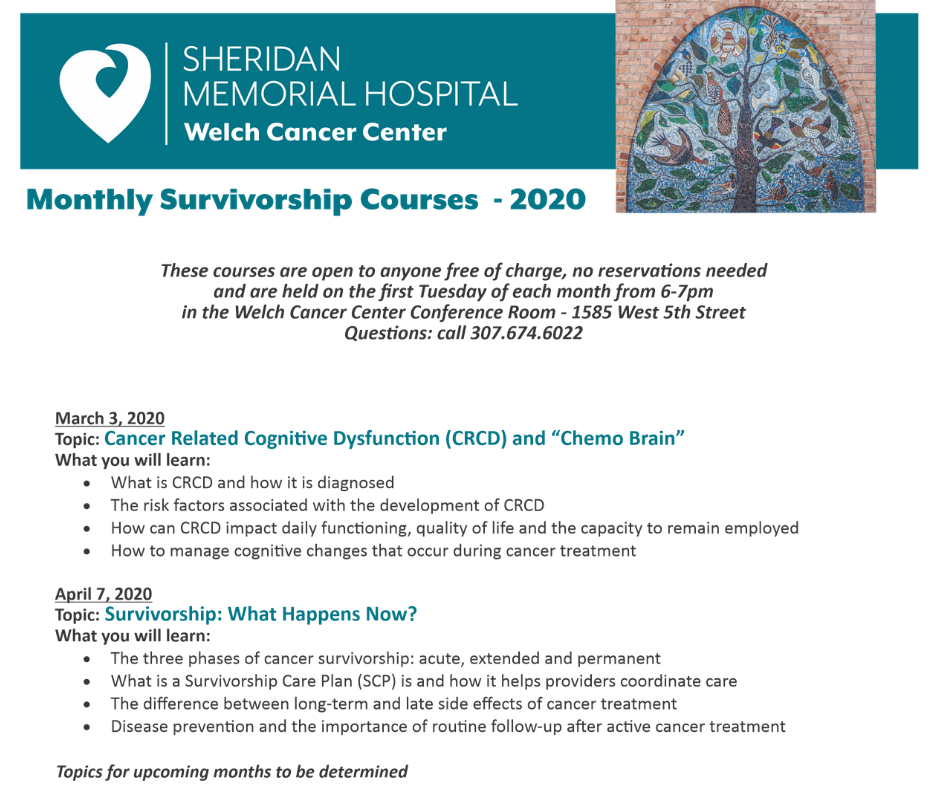
If you have had cancer, are receiving on-going cancer treatment or are closely connected to someone who is a cancer survivor, we invite you to join us.
The courses are designed to help those affected by cancer adjust to the challenges of “living well after cancer treatment”.
Let us partner with you by teaching you some tools to help you manage the distinct psychological, emotional and physical effects that often accompany cancer treatment.
These courses are open to anyone free of charge, no reservations needed and are held on the first Tuesday of each month from 6-7pm in the Welch Cancer Center Conference Room – 1585 West 5th Street.
Check out the schedule for the first quarter of 2020 which is attached to this story – you may attend any or all of the courses.
Questions: call 307.674.6022

Wyoming Rehab’s Cancer Rehabilitation Program can help patients before, during, and after cancer treatment. The program is a comprehensive treatment approach aimed at improving the physical function of individuals who have experienced cancer.
“It’s incredible how important cancer rehab can be in the life of someone who has or has had that diagnosis,” said the head of Wyoming Rehab’s Cancer Rehab Program, Charlotte Walter, DPT. “There are so many things cancer can effect in your physical functioning.”
In the past, patients with cancer were told to “take it easy” but this is no longer the case. Research shows that exercise is a safe and effective addition to an individual’s cancer treatment plan. Patients participating in supervised and structured exercise programs have been shown to have increases in aerobic capacity, leg strength, bone mineral density at the spine, and lean body mass superior to individuals only treated with usual care.
The Cancer Rehab Program is for anyone who has been diagnosed with cancer. An individualized starting point is determined for each patient depending on needs and diagnosis. When patients first come in an initial evaluation is done looking at their strength, balance, endurance, and pain and fatigue levels. Individuals are asked about their current levels of function and anything they’re having trouble with at home, work, and during recreation.
“We try to find things that the patients enjoy. For example I have a patient who enjoys walking and used to walk multiple times a day with her husband. That’s something she wants to get back to, so we focus a lot on walking, pacing, and energy conservation,” said Walter, a Physical Therapist. “The program starts with the initial evaluation, then we come up with an individualized plan to help reach the patient’s goals. The final step is either the transition to a home exercise plan or to a community based exercise program.”
Apart from the many physical benefits patients of the Cancer Rehab Program can see, there are also mental and emotional benefits.
“My favorite part is to see the emotional blossoming. These individuals have gone through an enormous treatment experience. They can come in sad, anxious, and nervous. We can show them this isn’t over yet. We can get them back and show them they don’t have to give up all of the things they used to do. Seeing that hope, confidence, and independence is so rewarding for me when I work with these patients,” said Walter.
Walter also discussed how incredible it is to have a program like this in a small town like Sheridan.
“I’ve had many patients tell me how happy and blessed they feel that they can get this kind of treatment, starting at the Welch Cancer Center, right here in Sheridan. They say how they were so encouraged when they didn’t have to go Billings or Denver to get that treatment. When patients see they can continue and complement that treatment here, with our trained health professionals and get the guidance they need, it’s a really special thing,” said Walter.
If you or someone you know is interested in the Cancer Rehabilitation Program at Wyoming Rehab, all you need to do is get a prescription for physical therapy from your oncologist or primary care physician. Cancer rehab sessions are billed through insurance and can differ based on an individual’s insurance plan.
For more information on the Cancer Rehabilitation Program, call Wyoming Rehab at 307-674-1632 or stop by 135 N Gould St, Sheridan, WY.

This Month’s Working on Wellness Employee of the Month is
Internal Medicine’s Hannah Hall, MD! Hannah prioritizes her health not only for
herself, but for her family, patients, and staff as well. She discussed the
importance of priorities, a healthy lifestyle, and preventative health.
Health has always been an important part of Hannah’s lifestyle and she’s taken
many of the things she gained from an active childhood into her adult life.
“As far as staying healthy I was raised that way. My parents got me involved in lots of activities like tennis, basketball, and soccer,” said Hall. “Growing up we did a lot of outdoor activities like hiking, camping, fishing, hunting, sailing, and water skiing. I had exposure to a lot of activities, including lifelong sports like golf.”
Hannah went on to play tennis in college for a few years and
also participated in intramural sports. She was also a big runner until a knee
injury 5 years ago. Since then, she’s had to find new activities to keep her
healthy and one of those activities is hockey.
“My newest thing is hockey, I started a few years ago as a novice at the rink.
I ice skated a little growing up but not a ton, and I wasn’t very good. Novice is
great and I enjoy it because it’s a lot like soccer and basketball. You get
that same sports feel and its competitive. It satisfies the competitive nature
in me and It’s really fun. I have a smile on my face the whole time I’m out
there,” said Hall.
Along with hockey, Hannah does weight lifting at the hospital’s employee gym
and enjoys using her Pelton bike at home.
When asked what motivates her, she discussed the importance of balancing priorities and making time for self-care.
“You have to figure out a balance in your priorities and for
me that’s taken awhile. You come out of school and your priority is work and
that’s probably not the healthiest to have. For me, I figured out it’s faith,
marriage, family, and then work,” said Hall. “To have those lined out I have to
be healthy and I have to make time for self-care. That’s what motivates me. I
have to take care of myself in order to be available for my family, patients,
and staff.”
For Hannah self-care means exercising, eating healthy, and making time for the
outdoor activities she enjoys. After seeing how health has always been a
priority in her life, it’s easy to see why Hannah is passionate about
preventive health for her patients.
“In my job a lot of issues are related to weight and lifestyle. It’s a big
thing that I talk to people about and I always ask what motivates them. If you
can find out that people are motivated to work on lifestyle changes, I think
that’s the best thing. If you can motivate people to make those lifestyle
changes early on you can prevent things like diabetes and heart disease,” said
Hall.
The advice she would give others who are ready to make a lifestyle changes is to set small goals and to find things you enjoy that you know you can do for a long time.
“Don’t expect that you’re going to go from not exercising ever, to doing an hour a day. Start with small goals and don’t get discouraged if you start a change and you don’t see results right away,” said Hall. “You’re doing something great so give yourself credit. I always ask what works for you? What have you seen success with? Pick something you think you can do for a long time.”

By Joseph Garcia, MD – Cardiologist from Sheridan Memorial Hospital’s Heart Center
February is Heart Month and it is particularly fitting that Sheridan Memorial Hospital has accomplished Accreditation by the American College of Cardiology (ACC) for the treatment of congestive heart failure.
What exactly does this mean?
It means that Sheridan Memorial Hospital has made management and treatment of congestive heart failure a major priority to improve patient quality of life, improve survival rates, reduce hospitalizations, keep patients employed (or doing as much of their daily activities as possible) within the limitations of their heart.
Congestive heart failure occurs when your heart muscle is unable to pump blood efficiently because the heart pump is either too weak or too stiff to be able to function. When the heart is unable to pump efficiently, the pressures inside the heart start to rise and the circulation starts to back up to the point where, in severe cases, you develop fluid in your lungs as well as swelling of your lower extremities.
Persons who start developing heart failure usually begin with symptoms such as shortness of breath on exertion or inability to breathe comfortably while lying flat ad having to prop themselves up to breathe better. Most persons develop fatigue, weakness, a faster than normal heartbeat, reduced exercise tolerance and increased urge to urinate at night. As heart failure symptoms worsen, persons may experience swelling of the abdomen and lower extremities, resulting in rapid weight gain from fluid retention.
Major conditions, which can result in heart failure, include significant obesity, poorly controlled high blood pressure, poorly controlled diabetes and coronary artery disease. Excessive alcohol and tobacco use also contribute to heart disease. Some medications, both prescription and over the counter, can also result in heart damage.
Not all conditions that lead to heart failure can be reversed, but there are treatments that can improve the signs and symptoms of heart failure and help you live longer. A person can undergo lifestyle modifications such as not smoking, controlling diabetes and blood pressure, staying physically active, eating healthy foods, maintaining healthy weight and controlling stress. By reducing these risk factors or undergoing necessary surgical options, heart failure can be minimized. The stronger your heart pump is, the longer the overall life expectancy will be for the patient.
The ultimate goal for diagnosing and managing heart failure is early recognition and intervention. Patients that receive a new diagnosis of heart failure in our facility leave the hospital with a heart failure specific bundle. This bundle consists of a scale, pulse oximeter, blood pressure cuff, a calendar, a recipe book for heart heathy cooking, and an education booklet on living with heart failure. By increasing heart failure education and providing useful tools for success, patients will have a greater awareness and appreciation for their health.
Sheridan Memorial Hospital is proud to announce that the American College of Cardiology (ACC) has awarded SMH the Heart Failure Accreditation based on the hospital’s competence and specific standards that are in place to provide excellent care to patients with heart failure.
The mission of the ACC is to transform
cardiovascular care and to improve heart health. Heart failure is a condition
where the heart is unable to pump enough blood to meet the body’s needs for
blood and oxygen.
“This is not an easy accreditation to obtain,” said Cath Lab and Interventional
Radiology Manager, Kristi Ramsey, RN.
The accreditation is awarded after a
rigorous onsite review by the ACC. The yearlong process is a review of 73
mandatory components that focus on the hospital’s policies, standards,
protocols, and education related to heart failure. SMH staff reviewed policies
and ensured that the ACC heart failure guidelines for patient care were met or
exceeded.
“This is not a one and done process. It’s an ongoing internal look at how we
care for the specific population of our community that has this disease,” Ramsey
added. “It’s
a constant rigorous look at policies, protocols, and standards and making the
appropriate adjustments needed to evolve with the constant changes and
improvements in the care of the heart failure patient.”

The ACC requires the hospital to submit documentation to show its continual process of improvement in heart failure care, including education offerings to providers, staff, EMS and the community; benchmarking and improvement in specific metrics showing a continual improvement over a six-month period; and tracking patient education and follow up post hospitalization.
The Accreditation is for three years and then SMH will be re-reviewed on all 73 mandatory components for re-accreditation.
“We are honored to have earned this accreditation,” Ramsey added. “It took a lot of work on the part of many physicians and employees. It will definitely help us in our mission to provide excellent patient-centered care for our community.”

By Christopher M. Prior, D.O. Sheridan Memorial Hospital Internal Medicine
Have you ever had a bad fall, felt like you were going down from being light headed or dizzy, or due to clutter in your surroundings? If so, then you know how scary it can be to feel out of control as you think about falling.
For almost 20 years now falls have been the leading cause of fatal injury and the most common cause of nonfatal trauma related hospital admissions among older adults. Twenty five percent of people over the age of 65 fall every year. One out of four fall victims will be admitted to the hospital and, on the extreme end, approximately 1% of those admitted to the hospital will die as a direct result of their fall. The financial cost of falls will surpass $67 billion annually next year according to the National Council on Aging.
There are many reasons why older adults may experience a fall. Potential causes for the increased number of falls in the elderly may be in part due to:
- people living longer
- living longer independently
- living longer with chronic conditions
- certain medication use
- neurological deficit
- cognitive impairment
- lower extremity weakness
- malnutrition
- social isolation
Fear of the cost of assisted living and poorly reimbursed home health may also contribute to placing the elderly at risk. Studies show a fear of falling and a sensation of gait unsteadiness are indications for interventions to reduce fall risk.
Some interventions that have proven to decrease fall and fall injury risk include:
- limiting some medications
- regular exercise
- proper diet
- vitamin D supplementation in those with low vitamin D
- correcting visual problems
- appropriate footwear
- removing environmental hazards
Studies show that for every medication taken more than 4/day the risk of fall increases by 14%. Certain medications that affect balance, vision, and alertness may increase risk of falls. While it may be necessary to take certain medications due to individual medical problems (such as Parkinson’s disease, diabetes, or hypertension) a discussion with your medical provider and pharmacist can help with determining the advantages and disadvantages of continuing medications that may increase the risk of falls.
Numerous studies show weight bearing and balance exercise can reduce the risk of falls in the elderly. Neuromuscular training such as Tai Chi reduces the risk of recurrent falls by greater than 50%. While there are no specific guidelines as to the type or duration of exercise, the United States Preventative Task Force recommends exercise to reduce fall risk in those over 65 years old.
Elderly with low vitamin D concentrations are at a greater risk of loss of muscle mass, decreased strength, and hip fractures. Vitamin D supplementation in patients with low vitamin D has shown to reduce risk of falls. The American Geriatric Society recommends supplementing with 1000 international units of vitamin D a day for adults at risk for falls with total vitamin D concentrations less than 30.
Visual problems such as cataracts, glaucoma, and macular degeneration contribute to fall risk.
Users of multifocal glasses had a reduced fall risk when wearing single focal length glasses for outside activities. In addition, delays in second eye cataract surgery place patients at a greater risk of fall with injury at that time.
Environmental hazards such as broken or uneven steps, poor lighting, throw rugs or clutter increased risk of falls. Handrails, slip resistant decking, and grab bars have proven to help reduce fall risk. Proper training and appropriate use of assistive devices such as canes or walkers may also help. Appropriate footwear and orthotic devices to reduce foot pain have shown benefit in fall rate reduction as well.
It is impossible to prevent every fall and fall induced injury. Intervention to identify elderly at risk for falls should include a history of falls, medication review, gait, balance, mobility, and environmental assessments. Multifactorial fall risk assessment has shown reduction in fall risk but no change in fall related morbidity and mortality. The American Geriatric Society recommends a multifactorial approach to identify at risk elderly.

Two years ago, Lori was chosen as one of our first W.O.W employees of the month after starting her health and wellness journey. One of her biggest motivators has been to keep up with her son Sean. After becoming a runner and calorie counting she lost over 40 pounds. We recently sat down with Lori to learn what she’s been up to and see where her lifestyle changes have taken her.
Lori’s journey hasn’t been without trials. After losing over 40 pounds she ended up gaining some of the weight back.
“I did the bounce back, I did the yoyo. After I lost the 40 pounds I went on a two-week vacation and I gained back the weight and I was so disappointed. I knew I had to get back again,” said Lori.
That’s when Lori’s mom introduced her to HealthyWage, a website and app that uses cash prizes as a motivator for weight loss. It’s not a weight loss program but an incentive program where individuals bet on themselves.

“In my case I said I would lose 50 pounds in 6 months and I did $65 dollars a month. I didn’t quite reach my goal in 6 months so it let me extend another 6 months. I did reach my goal and at the end I received a sizeable check. My mom and I both did this and we both came up with the best return on investment. It was a huge incentive and for me it was motivation to keep going. It was the fact that it helped motivate me to lose weight,” said Lori.
Strategy and timing are a huge part of Lori’s wellness journey and along with using resources like HealthyWage and the LoseIt app to calorie count, she also incorporates fitness into her everyday life including when she goes on vacation.
“This year we went to Europe and there was no calorie counting there. Sean and I had a goal that we wanted to do a run in every country. We ran in the Alps, Germany and Austria,” Lori said.

After 4 years in the Airforce and 10 years in law enforcement where she was told she had to run, for the first time in her life Lori is really enjoying running. This year Lori will do the 10-miler run again that she’s done since she first started her health and wellness journey. Her family friend, Marv who helped train her for the police academy also does the race every year.
“I’ll do it every year until Marv stops doing it. He’s in
his 90’s and as long as he’s doing it I’m going to do it,” said Lori.
Lori’s story is inspiring and proof that although there may be ups and downs in
your health and wellness journey, the most important thing is to never give up
and that may mean starting over.

December WOW Employee of the Month- KC McKenzie, Wound Care PA-C
December 2019
A year and a half ago KC had a wake-up call about his health via his results from the annual hospital wellness blood screen.
“I always knew I was kind of heavy, but the yearly blood screens served as a big motivator for me.”
The year before, KC’s blood screen showed that he had an elevated fasting blood sugar, so the following year he had an A1C test done. The results showed that KC was getting close to becoming prediabetic and as a health care professional who knows the consequences and repercussions of diabetes, he knew that he needed to make a change.
“Just knowing that I was getting close made me nervous,” said KC. “I didn’t want to be diabetic and I had control over it and knew that I had to change.”
A healthy diet and exercise routine helped KC reach and maintain his goals. He found success in time restrictive eating by following a schedule of only eating between 2 pm and 6 pm each day. On top of his eating schedule, KC also makes heathy choices by eating more plant-based foods and lean meats as well as limiting alcohol. A healthy lifestyle is all about balance and KC has found that through his new habits he’s able to enjoy a beer with friends or a slice of pizza on Friday nights through moderation.
“I’ve always been a gluttonous eater and I always failed at calorie restriction,” KC said. “Time restrictive eating has been sustainable for me for over a year now. I like that I can grab a salad at 2 pm, try to get a work out in, and have a modest dinner.”
A little exercise every day is KC’s fitness goal and what he’s found sustainable. He tries to get in a mix of moderate cardio, body-weight exercises, and weight lifting throughout the week.
“Having the gym here at the hospital and YMCA has been super helpful. I love to play noon ball at the YMCA and I really enjoy running intervals.”
When asked what advice he would give to people struggling to make healthy changes KC had one answer, try and try again.
“It would just be to try multiple modalities and find what works for you. We’re all so different and you have to know that multiple things are going to fail and that you just have to keep hacking away at small things until you find what’s sustainable for you long term. Expect to relapse and try to get back on the horse as soon as you can.”
KC’s lifestyle changes have given him more endurance, less stress, and mental clarity. However, the biggest benefit to him has happened at home. He’s able to do the things that he and his family enjoy, like skiing and hiking, as well as just being present for them.
“I go home now with a much better attitude and am able to help my kids with their homework and help my wife with chores,” said KC. “I’m a better husband and a better dad overall.”

Liz Mahoney – Director of Quality at Sheridan Memorial Hospital
November 2019
Physical Health Impacts Mental Health
Liz has always enjoyed being active – from swimming competitively growing up to running track in high school. Seven years ago exercise took on a new meaning as she turned to activity to help cope with the pain she experienced upon her young daughter’s accidental death. “The training for my first Ironman event provided an outlet for my grief and pain associated with her death.” Liz learned that her mental health was directly correlated with physical activity and continued to use exercise as a way to manage life’s ups and downs. Since then Liz has several half and full Ironman races (a full Ironman includes a 2.4 mile swim, 112 mile bike ride, and 26.2 mile run). She just returned from an Ironman competition in Florida – completing it in 15 hours.
Accepting the Invitation
As an adult Liz started biking with an invitation from a friend to join her in riding in the Tour De Wyoming. It took a little convincing, but eventually Liz agreed and her love of biking was born. Liz has now completed 6 Tours De Wyoming which is a cycling tour throughout different places in Wyoming ranging from 375 – 400 miles of the course of several days. This love of biking lead to triathlons and now is a large part of Liz’s identity.
Overcoming Set-backs
The amazing success Liz has seen in her athletic endeavors has not come without hard work and the occasional set-back. Liz injured her knee in one training cycle and wasn’t able to race again for 2 years. She worked hard to recover and in her comeback race she was disqualified due to being misdirected by a course official. This still didn’t cause her to quit and she signed up for another ironman a few months later. Liz is motivated by setting and reaching goals and this helps her be successful. “My advice is to set a goal, develop a plan, be flexible when things don’t go as planned, be consistent, surround yourself with people who are supportive or who have similar goals, and don’t give up even when things get ugly.” There isn’t a large triathlete community in Sheridan however Liz allows her internal motivation to push her further and connects with individuals at races around the country when she competes.
Dreaming of Kona
Liz is always learning and growing in her wellness journey. She has made many changes to her nutrition and continues to experiment to find out how to best fuel her training. She uses a training plan called “Training Peaks” and also utilizes her Garmin watch to monitor her training. In the future Liz plans to hire a coach with a goal to eventually qualify for the Ironman World Championships in Kona, Hawaii. This is a big goal but Liz is not deterred because she knows with the help of a supportive community she can be successful and remain competitive.
Click here to learn more about Wellness at Sheridan Memorial Hospital

By Cheryl Relaford, Patient Account Manager at Sheridan Memorial Hospital
November 2019
Healthcare costs can be scary. When you lack health insurance coverage, you find yourself worrying what will happen if you or a family member becomes ill. You avoid taking preventative care measures because you have fears about, not only the financial burden, but also what the test may reveal. But there is a solution. Sheridan Memorial Hospital can help. Plan to drop by the hospital’s downtown location, 61 South Gould, on November 14 from 5:30-7:30 pm for free help navigating the marketplace. Details can be found at the bottom of this story.
Background
Marketplace insurance allows for the protection of you and your family. The Affordable Care Act of 2010 established the insurance marketplace as a means to achieve maximum compliance with the mandate that all Americans carry some form of health insurance. Open Enrollment is currently taking place until December 15. Purchasing marketplace insurance gives you the opportunity to have essential health benefits to help you afford doctor visits, preventative care, hospitalization, prescriptions and more. These insurance plans cannot deny coverage because of pre-existin or chronic conditions, like cancer or diabetes and women and men cannot be charged different premiums.
When you explore the marketplace options at Healthcare.gov, you can find affordable health insurance coverage. You may qualify for tax credits which lower your monthly premiums as well as your out-of-pocket costs. Most people who apply can qualify for savings that the Marketplace offers. Having health insurance gives you an opportunity to provide the necessary protection for you and your family, by helping you establish access to preventative care and early detection to keep your health on the right path.
Insurance obtained through Marketplace Open Enrollment becomes effective January 1st, 2020. Begin preparing for the next chapter in your life by starting 2020 with the security that you have health insurance.
Where to find help
If you’d like to learn more and take the fright out of healthcare costs, visit Healthcare.gov. You can also contact a Sheridan Memorial Hospital Financial Advocate, who is also a Certified Application Counselor, to help you navigate the marketplace. To reach a Sheridan Memorial Hospital Financial Advocate call 307-675-4620 or email financialadvocates@sheridanhospital.org.
If you are unsure about how to get started or need help, we invite you to join us for our Health Talk: Open Enrollment event on Thursday, November 14th from 5:30 – 7:30 pm. Sheridan Memorial Hospital will host the event in the Community Conference Room at its downtown location: 61 S. Gould St. Certified Application Counselors from the hospital who are trained in the Insurance Marketplace enrollment process will be available to speak with you. This service is free and open to the community and there will be hors d’oeuvres and refreshments.
more information

October 2019
Approximately 3 ½ years ago, Brady was given the challenge to participate in the “Run to the Pub.” Thinking that it was probably a time to make some changes in her life, she committed to doing the run with her mom and some friends. “I mean…how bad could it be when you are running to the bar to go have a few beers with friends.” This was the first time she had done any kind of running and she “nearly died. In reality, even though it was hard, she ended up really liking it because of the way it made her feel. She thought to herself that if she could run when she was so out of shape, she was going to give it her all and make it happen.
She and her best friend combined efforts and continually support one another in making significant changes in their lifestyles. “It’s so much fun to have someone to run with and share thoughts and ideas about exercise and diet.” Now 50 pounds lighter and several races behind her, she is more determined than ever to continue down the Wellness Path.
The result of making all these changes in her life has been great for her family. Their priorities have changed and it’s brought about some major changes for all of them. They spend more time together as a family doing outdoor activities like hiking and fishing and her boys even participate in some of the 5K races that she does. Eating healthier, adding in more fruits and veggies instead of eating just meat and potatoes, has been a significant change for all of them. Brady has worked hard on creating a more balanced diet for her and her family. She focuses on portion control and doing things in moderation. “When you are working full time, it’s harder not to order out, but you have to stay committed to leading that balanced lifestyle and know that it’s better for you and your family.”
Another significant change that her running has brought about is a sense of calmness and peacefulness to her life. The energy that she spent on being anxious, she now puts into her running. She recognizes that when she doesn’t exercise it affects her mood and the way she feels physically and mentally. Because of her profession, Brady realizes that what you do now will affect you significantly later in life. She has seen too many patients with COPD, obesity, joint pain, difficulty moving, and living life in a wheelchair. Brady wants everyone to know that it is never too late to start focusing on living a healthier lifestyle and the positive outcomes it can bring to you and your family.
Brady uses her Fitbit and the Runtastic App on her phone to track how far she runs and walks in a week. “They help to keep me on track.” She and her friends like to challenge one another and the competition is fun. More important than devices, though, is running with her friends. “We keep each other accountable and have a little mom-time together.”
Recently, her husband filled a pack with 50 pounds and put it on her. He wanted her to see what an impact the positive lifestyle changes have made in her life. “It helped me to remind myself that your health is so important and there is no value that you can place on it.”

By Kristi Ramsey, RN, BSN, RCIS, CVRN – Sheridan Memorial Hospital Cath Lab Manager
October 2019
Today in the United States, approximately 5.7 million adults have a condition known as Heart Failure, with an additional 500,000 adults being newly diagnosed each year. Heart Failure is when the heart is unable to pump enough blood and oxygen to meet our body’s needs.
Being overweight is one of the main risk factors linked to heart failure. Measuring a person’s Body Mass Index (BMI) can help determine the risk of weight-related diseases. BMI is a tool which measures body fat using height, weight and age to determine where a person falls on a standard weight chart. The chart scores into four different categories: underweight, healthy weight, overweight and obese. The most recent statistics show that at least 20% of Americans fall into the obese category.
Determining BMI is a quick and fast assessment to determine our general overall health. Knowing your BMI can help you and your physician assess what goals or lifestyle changes you may want to consider.
Along with BMI, another important tool is measuring waist circumference. This tells us where our body stores fat. Persons whose bodies store fat around the waist are more likely to have weight-related diseases including Heart Failure, Type 2 Diabetes and High Blood Pressure.

