Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
Health and Wellness

We know there is a lot of pressure on people to enjoy themselves during the holidays. The season is supposed to be merry and bright, but many can feel increasingly isolated and unhappy this time of year.
Knowing how to juggle the holidays can be challenging, especially as the coronavirus pandemic looms overhead. Do what you can to get involved and get into the holiday spirit without stressing yourself beyond your limits or risking anyone’s health. If you put too much on your plate, neither you nor your loved ones will likely enjoy the festivities nearly as much. Remember that most families are facing difficult decisions and holiday celebrations are bound to look very different this year. Get creative and remember: your best efforts are good enough!
Isolation makes the holidays hard. According to the National Institute of Mental Health (NIMH), older adults who are socially isolated are at higher risk for depression. The focus on family, friends and togetherness can bring melancholy feelings to the forefront during this time of year. With coronavirus cases ramping up, it’s more important than ever to be supportive of, and attentive to, our loved ones, but in ways that keep everyone as safe and healthy as possible. This problematic situation poses serious challenges for families across the country and around the world.
If you or a loved one, friend or neighbor feel lonely or depressed, there are steps that you can take to help lift spirits. Remind yourself what the holiday season is truly about. Simplifying some things will allow you to focus on what really matters: the important people in your life.
With more of us forced to celebrate the holidays alone, I’ve assembled this list of suggestions for how to feel more connected during the holidays. I hope you can use some of them to brighten up your winter season.
- It’s not just about you – reach out to others. Some older adults may go days without speaking to anyone, especially those in poor health or who have limited mobility or transportation options. Connecting with them can make you feel better too.
- Make phone calls. Dial-up someone you haven’t spoken to in a long time. The chances are they would welcome a conversation. Make a point of actively listening to what they have to say. Find out what’s going on with them and their families. The call may lift their spirits and yours as well. Then keep the communication going in the new year by setting 15-30 minutes aside once a week to talk. Emails are a great way to stay in touch too.
- Listen to them. Even if the discussion is negative, an honest and empathetic conversation can help someone who might feel distressed. If you know of someone in need, encourage their friends or family members to reach out to them as well. When you help others, you help yourself.
- Share your feelings. Be honest with the people you trust, and tell them you’re feeling lonely. Divulging these feelings is a vulnerable and daring act – which most people will appreciate. They’ll want to help.
- Ask for what you need. Sometimes we hope others can read our minds, and we can become disappointed and feel disconnected and lonely when our needs are not met. It’s important to clearly communicate your needs to others. For instance, you might ask your spouse to give you a hug or your child to make your favorite dessert.
- Remember that you can do some things. Is there a hobby that you used to enjoy, but you don’t do anymore? Maybe it’s time to revive it – or to try something new. Do what you are capable of, and if you can, do something for someone else. Perfect your skills and look toward the future when you are able to share your time and talents with others.
- Try to simplify your holiday plans to focus on the real meaning of these celebrations. Let others know you are trying to ignore the increasing hype over the food, gifts, decorations, and parties to focus on the people and values you cherish. Remind others of the importance of family and friendship and thank them for that.
- Check with your church or religious organization to see if there is a way you can offer social and/or spiritual support. Just having someone to talk to can go a long way toward relieving depression.
- Make plans! A night alone doesn’t have to be a sad occasion. Quite the contrary, make a plan to do something special for yourself. Watch a fun movie or do something that makes you laugh. Genuine laughter creates extreme relaxation. This relaxation affects your hormones. If something makes you laugh, levels of stress hormones drop, and the feel-good chemical dopamine increases.
- Treat yourself and others. Make traditional baked goods or treats. Make your dining table festive – even if it’s just for yourself.
- Often the reason for our loneliness and unhappiness roots in our thoughts or mindset. We focus our thoughts on what we don’t have instead of what we do have, making us feel incomplete and unfulfilled. During this joyous season, cure your loneliness by doing the opposite: focus your thoughts on what you do have instead of what you don’t have. Be grateful for all the blessings and opportunities you’ve had this year.
Have a safe, happy and heartfelt holiday season!

By Erica Ridgeway, BSN, RN – Sheridan Memorial Hospital Trauma Program Coordinator
Sheridan Memorial Hospital’s Trauma Program reviews cases for patients who have suffered a trauma of any kind. Along with this, we review and develop policies and protocols to ensure best practices are followed and that each traumatic injury receives the most appropriate care. We also work to provide education about current policies, changes in policies, and changes in best practices. This includes doing community outreach and information related to injury prevention. By following these protocols, Sheridan Memorial Hospital has earned the designation as an Area Trauma Hospital from the Wyoming State Trauma office.
Injury prevention is an important part of a successful trauma program. One of the most common traumatic injuries in any trauma registry are falls resulting in fractures, therefore making fall prevention and safety extremely important.
The National Coalition on Aging notes that one in four Americans aged 65+ falls each year. Falls are the leading cause of fatal injury in older adults and are the most common cause of trauma-related hospitalizations for that population as well.
According to the Centers for Disease Control and Prevention, one out of five falls results in a serious injury such as a broken bone or a head injury. More than 95% of hip fractures are caused by falling.
There are many conditions that can increase the risk of falls:
- Lower body weakness & impaired balance: As we age, many of us lose some coordination, balance and flexibility, oftentimes due to inactivity.
- Use of medications: Some prescription and even over-the-counter medications can cause dizziness and dehydration, making you more likely to fall.
- Vision problems and changes: In the aging eye, less light reaches the retina, thus making tripping hazards and obstacles harder to see.
If you have concerns about falling or other issues, schedule an appointment to talk to your doctor or healthcare provider. They can evaluate your risk of falling and help implement specific things you can do. They can also refer you to a physical or occupational therapist who can help with balance and strength training. Tai Chi is an exercise that is often taught to help with balance and stability. There are many fitness programs offered both in-person and virtually that are designed for older adults. Additionally, some physical or occupational therapists will even come into your home and help assess safety and tripping hazards.
If you have had a fall or have a nagging ache, pain or physical impairment preventing you from going about your daily activities, Sheridan Memorial Hospital’s Wyoming Rehab may be able to help you. Their physical therapists offer free screens and treatment recommendations for non-emergent physical impairments and injuries.
Some things you may want to consider implementing in your home include:
- Get rid of things you could trip over and reduce clutter; rugs, in particular, can cause falls.
- Add grab bars inside and outside your tub or shower and next to the toilet.
- Put railings on both sides of stairs.
- Make sure your home has lots of light by adding more or brighter light bulbs.
- As the weather is getting colder, make sure you have appropriate footwear with a good grip.
- Devise a plan with family or friends for snow and ice removal around your home’s exterior.
So again, reach out to your healthcare team! They can assess not only your risk of falling but also what steps to take to prevent a fall, as well as assess your ability to participate in a fitness program. Implementing the appropriate safety and health measures can greatly reduce your risk of falls and injury.

Diabetes is different for everyone, at every age. As we celebrate National Diabetes Awareness Month, SMH focuses on the impacts diabetes has on one’s life and the challenges faced. Meet our own smiley, sweet Megan Ripley who works as a Chemo Nurse at Welch Cancer Center. Megan shared with us her Wellness Journey, with Diabetes, and we find it an important one to share with all of you as we navigate this month, together.
While many of us prepare for cranberry sauce, sweet potatoes, and copious amounts of pie, one-third of the US populations is concerned with managing their blood sugar while still enjoying their meal. With much to be grateful for this time of year, we take a moment to appreciate the stories and knowledge surrounding the staff at Sheridan Memorial Hospital. This Diabetes Awareness month, we are excited to share with you how one of our own employees faces and maintains her wellness while facing the everyday realities of Type 1 Diabetes. Megan Ripley is an employee who has not only pursued wellness as a hobby, but has adopted it as her way of life. Even though she has to navigate through obstacles every day, from constantly maintaining healthy blood sugar levels to the everyday challenges of being a Chemo Registered Nurse, Megan strives to maintain her health and she does it all with a beaming smile on her face.
Megan Smith’s journey towards wellness started at the early age of 9, when she was diagnosed with Type 1 Diabetes. Type 1 Diabetes is a chronic condition in which the pancreas produces little or no insulin, a hormone needed to allow sugar to enter cells in order to produce energy. At the discovery of her condition, she feared how diabetes might affect her everyday life. Megan often wondered about what restrictions she would have to implement into her daily routine, or what opportunities she might miss out on because of her condition. However, Megan was fortunate enough to grow up just outside of Cheyenne during her early childhood and because of this, she was able to attend the Barbara Davis Center for Childhood Diabetes. “The doctors and nurses at the center were great and they always had the most cutting edge technology so I was able to get the best treatment possible” Megan shares. The Barbara Davis Center didn’t just have an impact on Megan’s physical health, but they were also able to provide her with tools to help maintain and enhance her mental health. Megan explained “I always wanted to grow up to become a nurse, but with my diabetes, I didn’t know if that would ever be possible. When the nurses in the center found out this was a fear of mine, many came forward to share with me that they too suffered from diabetes, and they showed me how they navigated throughout their day as a nurse with diabetes. The team showed me that I could still be the person I dreamed of becoming and I really can’t thank them enough for all the help they have given me throughout the years.”
The team at the Barbara Davis Center helped to give Megan the confidence that she could still live the life she wanted, but now she needed to figure out how she was going to balance it all. Megan went to work finding what other methods and tools she could use in her life to stay healthy and happy. One of the struggles that Megan was immediately faced with was what kind of exercise regimens she could use. High Intensity Exercise wasn’t on option because even if Megan liked it in the first place, and she didn’t, it could cause complications with her blood sugar due to Adrenaline production. You see, when Adrenaline (Epinephrine) is released from nerve endings or the Adrenals it acts on the liver, promoting increased sugar production as well as the breakdown and release of fat nutrients which travel to the liver and are converted into sugar and ketones. Simply put, Adrenaline raises blood sugar considerably, which for diabetics such as Megan who can’t naturally produce insulin, can lead to Hyperglycemia, causing damage to the vessels that supply blood to vital organs. So any strenuous exercise that would cause a spike in Adrenaline was unsafe for Megan to participate in. And if that wasn’t a large enough hurdle, Megan also was trying to find a way to manage her diet so that she could still enjoy all the foods she enjoyed so dearly, without causing massive spikes or falls in her blood sugar levels.
Megan was committed to finding a solution. She knew what a great influence exercise and diet would have on her physical and mental state, so she never quit looking for answers. Eventually, she found resolution to her exercise dilemma when she realized just how much she liked doing long-distance, moderately paced cardio. Walking, hiking, and biking were also activities that Megan loved doing because they could be done with others. None of them required going to a gym, none of them would produce adrenaline if paced correctly, and all of them promoted muscle growth and weight loss. As for her diet, Megan discovered portion control, a dieting strategy that she could utilize in order to keep eating her favorite foods, by simply adjusting and managing the portion sizes of her meals throughout the day
Once Megan knew how she was going to balance her exercise and diet, all she had to do was find a way to consistently motivate herself to continue eating healthy and exercising on a regular basis. Her motivation to stick to her diet is basic: “If I eat right and stick to my diet then I can stay healthy, but if I’m not willing to maintain my diet then my physical health will be seriously negatively affected.” Megan’s motivation to exercise is a little less cut and dry. Megan relies, for the most part, on friends and family to help her stay motivated throughout the week. On week days, Megan’s biggest motivator is her Dog Laya who is always eager to remind her about their daily walk together, they rarely miss a day, considering Laya is known to not taking no for an answer. A few days a week Megan also gets the opportunity to go on walks with friends from work, who she also credits as being some of her greatest supporters. On the weekends, Megan is motivated by excitement and adventure with her husband John and of course, Laya. Megan is always eager to plan out her family’s adventures and you can bet they’ll be doing a whole lot of hiking, canoeing, backpacking, or fishing with a whole lot of fruit snacks to keep her fueled. Megan’s most recent adventure sent her on a rigorous 16 mile hike, with almost 2450’ vertical gain to the beautiful and secluded Lake Angeline, high in the Bighorn Mountains.
Megan’s advice to all those who have a desire to get well was this: “Start small and set goals that are attainable, all of us progress at our own rate and your rate is completely unique to you, so don’t compare yourself to anybody but yourself. If you need a donut, then eat a donut, but eat less of something else or just exercise more to compensate for it. It’s all about balance. Do not underestimate the power of thinking positively, mental health is just as important as physical health, and being happy and thinking positively can take you just as far as any workout routine.”
We’re so very proud to see how far Megan has come from where she once was and we can’t to see where she goes. We’d like to thank Megan for her inspiring story and providing such positive insight into living a balanced life with Type 1 Diabetes. We appreciate you leading by example and for showing us all what it really means to take wellness into our own hands. Sheridan Memorial Hospital honored to have you as a member of our staff and we are grateful for everything you have done and continue to do for this hospital. Thank you, Megan.

This video displays the stark reality of how COVID is affecting St. Vincent’s Healthcare in Billings, MT. We are not far behind them and we need your help to slow the spread of the virus.
This week, October 26-30, 2020, active cases in Sheridan went up by 38% and COVID hospitalizations continue to climb. This trajectory will have a negative impact on our ability to provide healthcare services for Sheridan and the Region. We need to keep our healthcare system from becoming overwhelmed.
We are acutely focused on making sure we have people to take care of anyone who shows up at our hospital. People injured in accidents, heart attacks, strokes and acute illness. All of this becomes extremely difficult when we are not flattening the curve of this virus in our community.
We need your help!
- Maintain your distance with people
- Wear a mask in public settings
- Wash your hands

Your first impression when meeting Dr. Elise Sylar, the newest addition to the Internal Medicine team at Sheridan Memorial Hospital, may be that she is sharp as a tack. But the more you get to know her, the more you’ll come to realize that her heart is just as strong as her intellect. And although she may be brand-new to SMH, it’s clear that Dr. Sylar is by no means new to loving and serving the people around her.
Elise’s interest in healthcare began when she started volunteering at Camp Wapiyapi, a summer camp for children who have pediatric cancer in Estes Park, Colorado. There, Dr. Sylar formed close connections with campers and had the opportunity to leave a lasting, positive impact on the lives of the kids she interacted with. The experiences and memories Elise got from Camp Wapiyapi stirred an even greater desire to help and make a difference in the lives of others. So, when the time came for her to head to new horizons, Dr. Sylar was intent on entering the medical field, with hopes of specializing in pediatrics.
Following her graduation from Kelly Walsh High School, Dr. Sylar packed up and headed from her hometown of Casper to Laramie to attend The University of Wyoming, where she graduated with a degree in Physiology and a minor in Neurology. Before moving on to Med school, Dr. Sylar took a year to get some hands-on experience at the National Institutes of Health in Bethesda, Maryland, researching CAR T-Cell Therapy in an Oncology Lab working to find a cure for Childhood Acute Lymphoblastic Leukemia.
Dr. Sylar then applied and was accepted into the University of Washington School of Medicine, and thanks to the WWAMI program, Dr. Sylar got to complete her first year of med school in Laramie. During her attendance at Med School in both Laramie and Seattle, Dr. Sylar was given the opportunity to study and practice in all fields of medicine. When the time came to decide what she was going to specialize in, she decided against her original idea of pediatrics. Dr. Sylar explained, “I always thought I was going to go into pediatrics, even when I finished studying at UW. I was certain I wanted to become a Pediatric Oncologist. Still, the longer I studied at the University of Washington, the more I realized why adult medicine was a much better fit for me. My favorite part of healthcare is to form that connection between physician and patient. It’s empowering to see people become more knowledgeable and further involved in their healthcare thanks to the advice and resources that I can provide them. The problem I had with becoming a pediatrician was I knew forming a good connection with a child would be a much more difficult process than with an adult. I also wouldn’t be able to see my patients take an active role in their health because they simply don’t have the ability to be independent the way adults do.”
Dr. Sylar finished up Med School with a focus on Internal Medicine, and now, and after finishing her 3-year residency at the University of Arizona, she’s excited to get started building relationships with her patients right here in Sheridan.
Dr. Sylar shared, “I was always planning on coming back to Wyoming after I finished my schooling, in part because of the WWAMI program, but more than anything, the reason I came back was that I wanted to give back. I felt like supporting rural healthcare was the best way I could give back to the state that has provided me with so much throughout my life.”
Sheridan became the ideal community for Dr. Sylar because it suited both her needs and her spouse’s needs. “Sheridan Memorial Hospital offers a very robust healthcare system, which surprised me considering how rural the community is, it houses lots of innovative technology and offers practices which you wouldn’t typically find in rural communities, like vascular surgery, for example. It feels like the perfect place for me to begin my career, and since Sheridan houses a reasonably sized airport, it provides my husband the opportunity to continue his career as a pilot,” she added.
Outside of her profession, Dr. Sylar loves to spend her time hiking, mountain biking, and road cycling. And with the Big Horn Mountains just a few miles outside of town, it seems like Sheridan truly is the perfect place for her and her husband Ken to both work hard and play hard.
“I’m so excited for the opportunity I have to make a positive impact on the health and wellbeing of the people here in Sheridan. And I’m even more excited to start building great relationships, not only with my patients but with all the kind and welcoming people here at SMH.”
Call 307.675.2650 and choose Option 4 to schedule your appointment with Dr. Elise Sylar in Internal Medicine today.

October is National Physical Therapy Month. Did you know that Wyoming Rehab provides FREE Screens and Treatment Recommendation on Non-Emergent Physical Impairments/Injuries? The therapists at Wyoming Rehab want to provide you with some tips for living a healthier life.
Physical activity can significantly impact your long-term health. A study published in the July 2020 edition of the British Medical Journal reported that physical activity is key.
People who regularly get 150 minutes of moderate exercise or 75 minutes of vigorous exercise per week, along with 2 days of strength training, are more likely to live a longer, healthier life.
Here are some simple examples to help you get the exercise you need…
Moderate intensity: you can talk but not sing during the activities such as:
- Walking briskly
- Water aerobics
- Bicycling slower than 10 miles per hour on primarily level terrain
- Doubles tennis
Vigorous intensity: you cannot say more than a few words without having to pause to take a breath during activities such as:
- Race walking, jogging, or running
- Swimming laps
- Bicycling over 10 miles per hour with hills
- Singles tennis
- Aerobic dancing
- Hiking uphill or with a heavy backpack
Strength training: two days per week involves exercises specifically-designed to fatigue muscle groups using weights or other resistance. You can also use your body weight for resistance by doing push-ups, pull-ups, crunches, leg squats or push-ups against a wall.
Do you have a condition or impairment preventing you from reaching the recommended amounts of physical activity? Don’t continue to put your health at risk! Find out how physical or occupational therapy may help.
Reach out to Wyoming Rehab at (307) 674-1632 if you would like to schedule a FREE Screen/Treatment Recommendation for a Non-Emergent Physical Impairment or Injury.

By Nina Beach, MN, FNP-C, AOCNP, Advanced Oncology Certified Nurse Practitioner at Sheridan Memorial Hospital’s Welch Cancer Center
Cancer screening and preventive care are important aspects of overall health. Screenings look for cancer before a person has symptoms. If caught early, many cancers are much more treatable and potentially curable the sooner they are discovered. Wyoming has a particularly low rate of cancer screening. According to the American Cancer Society Cancer Statistics Center, Wyoming is now ranked 52nd (they count the District of Columbia and Puerto Rico) in breast cancer screening with mammography, 51st in colon cancer screening, and 40th in cervical cancer screening.
In other forms of cancer prevention, we are doing better with HPV vaccination for our girls with a ranking of 28th with 54% getting vaccinated, but doing a poor job with our boys – we are ranked 51st. Up to 93% of cervical cancers could be prevented through screening and vaccination.
There are many screening tests available. Research is continually being done to determine if screening actually prolongs life. We know that finding some cancers before they spread or metastasize increases the chance of successful treatment and potential cure. The recommendations for each particular test are weighed out regarding risk and benefit, and some tests are not without risks. Screening tests are not routinely recommended unless the benefit outweighs the risk. Additionally, people are living longer with cancer today than they used to – both because of screening techniques and the fact that treatments continue to improve.
At this time of uncertainty with COVID-19, a volatile election year, and just a time of feeling vulnerable to things out of our control, this is your way to make a difference. Choose to quit smoking, or maybe choose to work on obtaining a healthy weight. In Wyoming, we have a helpful factor in our favor, of low air pollution levels, which helps lower our cancer risk. We can continue to fight cancer by finding cancer sooner. Take control and make the choice for your health – talk to your health care professional about a mammogram, colonoscopy, Pap smear and vaccinations appropriate for you and your family members.
We begin to treat patients who have metastatic cancer (stage IV) at the time of their diagnosis. Sometimes these individuals have said they could not afford to be tested or see a health care provider. Paying for screenings should not be a deterrent.
There are a number of funding options for those in need. The Wyoming Cancer Program reimburses participating providers for some screenings for the uninsured. Sheridan Memorial Hospital’s Patient Financial Advocates work with people who need assistance paying for cancer screenings and/or have questions about the services available. Some of the assistance comes from funds raised each October at the Hospital Foundation’s: The Link ~ Partners in Pink run/walk.
To find out more or to see if you qualify for screening funds, contact the Sheridan Memorial Hospital Patient Financial Advocates at 307-675-4620. They can help you understand the available funding options and obtain the care you need.

By Cashlee Cates, Financial Advocate Supervisor at Sheridan Memorial Hospital
There are two different but important, health insurance enrollment periods this time of year. The first is the open enrollment period for Medicare, which runs from October 15 through December 7. The second is the open enrollment period for the Health Insurance Marketplace, which runs November 1 through December 15.
Medicare
For enrolling in Medicare, now is the time to take action. You can enroll in Medicare Advantage plans, Medicare Supplemental plans, or you can make changes to your existing plan during this same time period.
Enrolling in Medicare, or making changes to your existing Medicare plan, is done online at www.Medicare.gov. Once you are at the website, click on the “Sign Up/Change Plans” button at the top of the website and walk through the questions to provide the necessary information. There are many resources on this site to help answer frequently asked questions (FAQ) about general Medicare enrollment, Part D (drug coverage), the various costs of Medicare, general Medicare plan updates and much more.
If you have specific questions or don’t feel comfortable walking through the online process, the Hub on Smith is currently scheduling appointments to provide assistance with Medicare enrollment. To schedule your appointment, call 672-2240. It is important to call early on in this process as the appointment times fill up quickly.
If you are unable to get an appointment with the Hub, other resources are available for phone consultations across the state. Phone consultations may be available through:
- The Casper Senior Center – 877-634-1006
- Riverton Senior Center – 800-856-4398
- Wyoming Senior Citizens Inc. – 307-856-6880
There are many different resources available online to help provide answers to your Medicare questions. The few listed here offer excellent videos to walk you through the process:
www.MedicareOnVideo.com – This site provides a complete set of video tutorials about all things Medicare.
www.MedicareMadeClear.com – This site provides a series of videos on Medicare basics designed to simplify the four basic parts of Medicare.
Health Insurance Marketplace
Now, for those not quite ready to enter the world of Medicare, the Health Insurance Marketplace is for you; if you don’t have health insurance coverage already or want to explore options available to you. Remember, the Marketplace enrollment period is from November 1 through December 15, 2020.
Marketplace health plans offer essential health insurance benefits. These benefits cover things like doctors’ visits, prescriptions, hospitalizations, pregnancy and more. Preventive healthcare is another benefit offered through Marketplace plans. Some of the preventative benefits covered include blood pressure screenings, cholesterol screenings, immunizations and breast and cervical cancer screenings for adults. Preventive benefits for children include hearing screening, vision screening, behavioral assessments, developmental screening and immunization vaccines.
Plans through the State of Wyoming Healthcare Marketplace are available from Blue Cross Blue Shield of Wyoming. There are several ways to apply for coverage or look into coverage through the Marketplace program, including online, by phone, by paper application or with the assistance of a Certified Marketplace Navigator.
Sheridan Memorial Hospital (SMH) has Financial Advocates who are Certified Marketplace Navigators and are available to help you understand the coverage you could receive through a Marketplace plan. As Navigators, the Financial Advocates can explain plan options such as preventative care coverage, deductibles, out of pocket expenses and even dental care plans.
Your next question may be, can I get help paying for Marketplace coverage? You may qualify for financial help to lower the cost of your coverage. The Financial Advocates at SMH are here to help explain complex insurance options. If you are interested in assistance with the Health Insurance Marketplace, please call 675-4620 to make an appointment. You can also go to www.healthcare.gov to look into other options available through the Marketplace.

Taylor Wendtland came to Wyoming Rehab after living with moderate to severe low back pain for nearly 10 years. The pain affected his ability to participate in many of the outdoor activities he enjoys. Since coming for treatment, Taylor’s pain has completely resolved, and he is back to doing all the things he loves. Here Taylor is playing Ultimate Frisbee in the park after just a few weeks of treatment at Wyoming Rehab. Congratulations Taylor!!
Call Wyoming Rehab today at 307.674.1632 and ask about our FREE Screens and Treatment Recommendations on Non-Emergent Physical Impairments/Injuries.

By Sierra Gross Stallman, MD – Medical Director for Sheridan Memorial Hospital’s Internal Medicine practice
With our sunny 90 degree days and all the attention currently on COVID-19, it seems impossible to fathom flu season is coming near. Uncertainty about the future seems to be the one sure thing in the coronavirus pandemic. However, a few things are clear: the virus is circulating through the population and flu season is only a few months away. According to the Centers for Disease Control and Prevention (CDC), up to 62,000 people died and up to 740,000 people were hospitalized due to flu complications between October 2019 – April 2020. Hence, it is crucial we continue to be aware of, attempt to prevent and treat the flu, especially now with the COVID-19 pandemic wreaking havoc in our world.
Flu and COVID-19 can share many, though not all, symptoms including fever, chills, cough, sore throat, muscle or body aches, headaches, and fatigue. While as a community, we are working on limiting the spread of COVID-19 through multiple methods including proper hand hygiene, getting vaccinated is already an established prevention for flu. It is the best option to prevent, control, and decrease the socioeconomic burden of influenza. The influenza vaccine is more important now than ever as the Novel Coronavirus continues to spread.
Even though the flu shot is not perfect at preventing the flu, it can lower your risk of developing serious complications. Flu vaccinations have been shown to reduce deaths, ICU admissions, and overall duration of hospitalization. Within a population, the more people that receive the vaccine, the better it becomes at preventing the flu and its complications. Therefore, everyone who is able to get the flu vaccine, generally those six months or older, should get vaccinated, not only for your own health, but also for those around you. It is especially important for those at high risk of flu complications to get vaccinated, which includes: children 6 months to four years old, pregnant women, people older than 50, immunosuppressed individuals, and those with certain chronic diseases. Keep in mind that many people who are at high risk for developing a serious case of the flu are considered high risk for severe complications of COVID-19. In addition, health officials have confirmed that coinfection of flu and COVID-19 is possible and was seen at the end of the last flu season.
To protect our community through this coming flu season, it is important to consider timing of vaccination. Once people are vaccinated it takes about 14 days for the immune system to generate a protective response. The standard flu shot cannot give you the flu as it does not contain live virus, though it is possible to catch the flu before your vaccine takes effect. Studies have detected a steady decline in vaccine protection the months following administration. By six months after vaccination, flu vaccine effectiveness can be reduced by more than half. Therefore, individuals should try to get the vaccine just before flu activity starts, so that they are optimally protected for the duration of the season. Flu activity begins to increase in October and November, peaks between December and February and lasts until April and May. CDC guidelines are currently recommending people get vaccinated in September or October. This is based on data from previous flu seasons, suggesting tens of thousands of influenza cases and hundreds of deaths can likely be avoided if older adults wait until October to get their immunizations. While COVID-19 has been compared to the flu in regards to symptoms, they are not the same, and the flu vaccine cannot prevent COVID-19. With the Novel Coronavirus in our community and flu season coming upon us, getting the flu vaccine is your best first-line defense against getting sick. Please help us protect you, your loved ones, and those around you. Get vaccinated!

While the hot, summer month of August melts away and we rush on with the hope of cooler days, Sheridan Memorial Hospital would like to slow down for a moment to celebrate August’s WOW Employee of the Month: Megan Ripley. Megan is an employee who has not only pursued wellness as a hobby but has adopted it as her way of life and navigating through obstacles every day. From consistently maintaining healthy blood sugar levels to the everyday challenges of being an Oncology Registered Nurse, she strives to maintain her health, and she does it all with a beaming smile on her face.
Megan Ripley’s journey towards wellness started at the early age of 9 when she was diagnosed with Type 1 Diabetes. At the discovery of her condition, she feared how diabetes might affect the rest of her life. Megan grew up just outside of Cheyenne during her early childhood, and because of this, she was able to attend the Barbara Davis Center for Childhood Diabetes in Denver. Megan explained, “I always knew that I wanted to become a nurse. Many nurses that cared for me came forward to share with me that they, too, lived with diabetes, showed me how they navigated throughout their day as a nurse with diabetes. The team showed me that I could still be the person I dreamed of becoming, and I really can’t thank them enough for all the help they have given me throughout the years.”
Megan often wondered about what restrictions she would have to implement into her daily routine, or what opportunities she might miss. Still, this girl was committed to finding a solution. She knew what a great influence exercise and diet would have on her physical and mental state, so she never gave up looking for results. Eventually, she found the answer to the exercise dilemma when she realized just how much she liked doing long distance, moderately paced cardio. Walking, hiking, and biking are great activities for our WOW Employee of the Month because they are often enjoyed with others. Megan enjoys biking to work with her coworkers, walking her dog, backpacking with her husband, and riding her spin bike if the weather doesn’t permit outside activities.
As for what Megan eats, she doesn’t believe in sticking to a strict diet. Megan does her best to eat as many whole foods as possible. She enjoys eating fresh fruits; her favorites include honeydew melon, berries, and frozen mango chunks for a sweet treat. She also likes to eat fresh vegetables and always fills half of her plate with greens. She also likes to keep small healthy packs of trail mix on hand for snacking. Megan always feels her best when she is eating healthy and thinks that this is the best reward.
Megan’s advice to all those who desire to get well is this: “Start small and set goals that are attainable, all of us progress at our own rate and your rate is completely unique to you, so don’t compare yourself to anybody but yourself. If you want a jelly donut, then eat a donut, and go for a walk later, it is all about balance. Do not underestimate the power of thinking positively; mental health is just as important as physical health. Being happy and positive thinking can take you just as far as any workout routine.” Now more than ever, Megan’s advice reigns true in focusing on health and wellness in all aspects of our lives.

This month’s W.O.W Employees of the Month are the “Home Girls” from Sheridan Memorial Hospital’s Home Care, who won the hospital’s Spring Wellness Challenge, “The Amazing Race ‘Round Wyoming.” Casi Morgareidge, Shannon Stellingwerf, Jill Hegy and Martha Cover-Killian all competed together to win for the second year in a row!
This year’s challenge was held from June 1st to July 4th and encouraged teams to practice healthy habits daily. Each day, team members could earn points as follows:
– Eat 5 fruits or vegetables – 5 points
– Drink 64 oz. of water – 5 points
– Exercise for 30 minutes or more – 5 points
– 7 to 9 hours of sleep of each night – 5 points
We had the pleasure of sitting down with the Home Care team to discuss how they’ve been consistently successful.
The Home Care team has competed together in different challenges for the past three years. When asked about their success, it all comes down to teamwork and the bond they have toward one another. Their expectations of each other during a challenge is to commit to giving 100%, and they definitely hold each other to it. Their accountability and support for one another, both at work and during challenges, is truly the success of the Home Care team. If one of them is struggling, they unite together to do what is necessary to help their friend and co-worker stay on track.
When asked what the most difficult part of the challenge was, each of them struggled in different ways. Jill and Shannon felt that getting enough sleep and letting go of things at night so they could get to bed earlier was difficult. Casi said that eating her fruits and vegetables is always her biggest challenge, and Martha struggled to find the motivation to exercise on Sundays because of family time.
Their advice to future challenge competitors would be to set aside time for yourself to be active and schedule your exercise time like you would a meeting or a doctor’s appointment. It is best if you make every aspect of the challenge a priority in order to develop habits that continue long after the challenge is over. Doing this can have a major impact on your health.
They are a great team that is dedicated to each other, and repeatedly challenge one another to do their best. Congratulations ladies! You are an inspiration to all of us.

By Kristi Ramsey, RN, BSN, RCIS, CVRN – Sheridan Memorial Hospital Cath Lab Manager
The connection between diabetes and the heart starts with high blood sugar levels. Over time, those high sugar levels cause the arteries in the body to become hard and stiff. The less pliable the arteries are the greater chance for fatty deposits to build upon the inside of the vessel wall. This condition is known as atherosclerosis. These fatty deposits are also commonly called plaque buildup. The plaque can build upon itself to the point where it can completely stop blood flow to the heart muscle.
How can the heart be protected against other diseases such as diabetes?
- Maintain a normal blood pressure: less than or equal to 120/80 mmHg
- Keep Cholesterol in check – Normal range is less than or equal to 100mg/dl
- Stay in optimal weight range for your age and stature
- Be physically active: recommendation is 150 minutes of moderate intensity exercise or 75 minutes of vigorous activity per week
- Keep Blood sugars in normal range: Fasting <100; Before meal : 70-130
- Kick the habit of smoking and drinking alcohol
Some facts about diabetes:
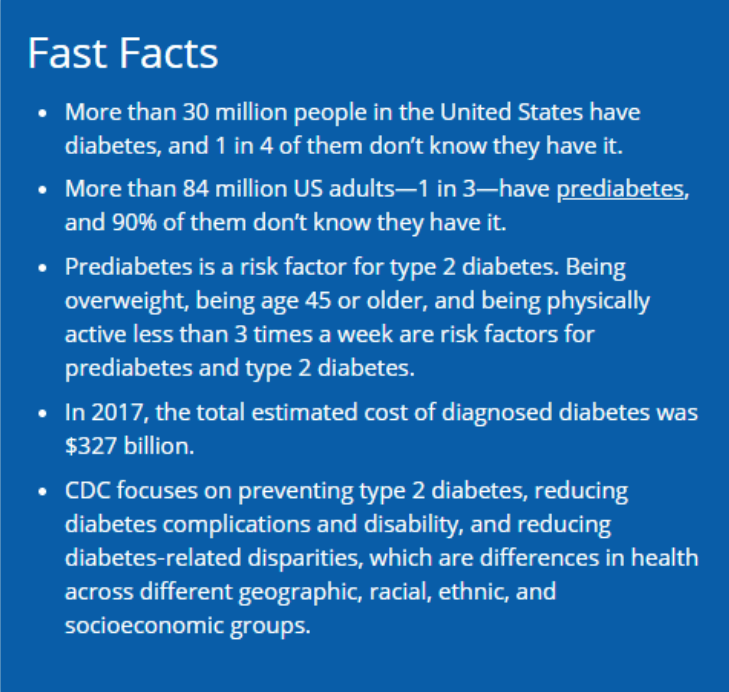
https://www.cdc.gov/diabetes/library/features/diabetes-and-heart.html
Sheridan Memorial Hospital is hosting a free drive-by Glucose Screening on Tuesday, June 30th. If you would like your glucose checked, just come to the employee parking lot outside of the cafeteria on June 30th from 9am to 1pm. Appointments are not necessary. No need to get out of your vehicle – just follow the signs and look for the tent in the parking lot on the North side of the hospital cafeteria. Health care professionals will be out there to give you a quick glucose test. They will also provide healthy heart information on living with heart disease and a handout on how to use your dinner plate format to help you plan healthy meals.
We do ask that wear a face covering when you come and if you are not feeling well that day, please stay at home.

If you have a dad, know a dad or are a dad… this is important. With Father’s Day coming up this Sunday, it is the perfect time to celebrate Dad. Now we all know the stereotype that men don’t like going to the doctor. However, it is necessary and best to do preventative maintenance before restorative maintenance is “required.” Ask any car guy and the advice will be the same. As they say, “An ounce of prevention is worth a pound of cure.”
So these health tips are focused on good ‘ol Dad. Let’s help breakdown the stereotype.
Schedule an Annual Checkup
The most preventative part of preventative healthcare. An annual checkup will cover from head to toe and everything in between. Even if you feel fine, consistent checkups and screenings are vital to protect your health. Find a primary care physician and be an active part of your healthcare plan going forward.
Make Sleep a Priority
Based on some research, up to 25% of men are sleep-deprived. Sleep deprivation can be linked to obesity, heart disease, depression and diabetes. Getting those eight hours a night can really work to improve work performance and your body’s ability to fight disease.
Eat Healthy
Today’s fast-paced society lends itself to fast-paced meals that are easy to acquire. This leads to too many fatty foods and drinks loaded with sugar. A little meal pre-planning and you can find yourself eating more fruits, veggies and lean proteins, which will make all the difference in your daily routine.
Unplug to De-Stress
While small amounts of stress can get you moving and help you complete a project, too much stress is hard on the body and mind. Find time to get away from the screens in your life (computer, phone). Go for a hike, take the kids fishing, enjoy a picnic with the family. This time away will not only help you come back refreshed, but also help with the most important social connections in your life.
Exercise
We’ve all heard it at some point… the benefits of exercise are tremendously helpful. It helps reduce the chances of heart attack, stroke, diabetes and host of other “issues” that can crop up. Exercise can also help you sleep better (see above). Even if you can only get in 30 minutes a day, that’s 2.5 hours per week, or 130 hours per year. Moreover, you are probably already getting some of this time in through yard work, shoveling snow, or other chores around the house.
Obviously, the key to all of this is to work on making habitual choices to improve your health. Healthy habits lead to longer lives with the ones we love.

Our W.O.W Employee of the Month for June is Kim Gilbert, Nurse Practitioner at Sheridan Memorial Hospital’s Internal Medicine practice. Kim recently completed a Post Master’s Certification program in Adult Gerontology Acute Care and passed her boards a couple of weeks ago. It is evident that life has been very busy for Kim as a student, Nurse Practitioner, wife, and mother of five. However, wellness is and continues to be a very important priority in her life.
As a young girl, Kim saw her mom as a dedicated runner. This inspired and motivated her to run with her mom and at the age of 11, she completed her first 10 K run. In January of 2020, Kim started training to run her first ½ marathon with her mom. Unfortunately, they had to cancel the race because of the dynamics of her mom’s new job. Instead, she joined her coworkers and together they ran the “Run ‘til Your Green”10K race in Sheridan in March. She is currently training to run the Crazy Horse and the Denver Rock-n-Roll ½ marathons in October.
Kim’s friends help keep her motivated and dedicated to her Wellness goals. In November of 2018, she and Amber Friis made a commitment to one another to run a mile every day until the end of the year. On December 31, 2019 they decided to continue their pact to one another and ran for 365 consecutive days.
It was difficult to carve out time to do the run, but her commitment to herself and to Amber kept her going. She looked to Liz Mahoney for encouragement and motivation. Kim was with her in Florida when Liz completed the Ironman. Liz told her, “Start where you are at, not where I am at.” That was the inspiration that she needed. Planning a week ahead and having an accountability partner also helps to keep her on task.
At Christmas that year, her kids gave her a trophy for running 365 consecutive days in a row. This acknowledgement from her family was an awesome lesson on persistence and commitment for her children to witness.
Kim struggles with her own body image and has worked hard to move past that. “You have to love yourself and give yourself the grace to accept who you are.”
Currently, Kim uses the “Couch to 5K” app and the Runners World training guide to prepare for her ½ marathons. She has engaged her daughter to train with her so she can get faster and her daughter can stay in shape for soccer. Her goal is to finish both races in October and run the entire time. Someone once told her, “It is so much easier to stay in shape than to get in shape”. How true this is…


At Sheridan Memorial Hospital volunteers are an integral part of our daily routine. During National Volunteer Week in April, we were pleased to honor the over 100 hardworking individuals who give us their time and talents every day. During these extraordinary times, we have asked most of our “regular” volunteers to stay safe at home. We thank them for their service and we miss their smiling faces. We can’t wait for them to come back to us.
Right now we have a call out for a different kind of volunteer — health care professionals who can help us care for patients in anticipation of a surge in hospitalized patients due to COVID-19.
Regardless of the kind of volunteer, we truly appreciate their commitment of personal time and energy to make a difference in the lives of others. Many people volunteer with the intention to help those in need, most times not thinking about what’s in it for them. But there are health benefits associated with volunteering that are good for the mind and body. The Mayo Clinic and Franciscan Health System suggest that volunteering offers many health benefits from lowering stress to boosting self-confidence.
Reduce stress, anger, anxiety
Volunteering may enhance a person’s social networks to lower stress and reduce the risk of disease. It can create a sense of meaning and appreciation, which can have a stress-reducing effect. The social contact aspect of helping and working with others can have an effect on a person’s overall psychological well-being. Nothing relieves stress better than a meaningful connection to another person.
Decrease risk of depression
Volunteering leads to lower rates of depression because people are in regular contact with others. Volunteering increases social interaction and helps build a support system based on common interests — both of which have been shown to decrease depression.
Stay mentally, physically active
Volunteer activities help people stay physically and mentally active — getting people moving and thinking at the same time. Older volunteers tend to walk more, find it easier to cope with everyday tasks and stressors, are less likely to develop high blood pressure, and have better-thinking skills. Volunteering can also lessen symptoms of chronic pain and reduce the risk of heart disease.
Increase happiness
Volunteering gives a sense of purpose. Researchers have measured hormones and brain activity of volunteers and discovered that being helpful to others delivers pleasure. Human beings are hard-wired to give to others. The more we give, the happier we feel. The more meaning people feel in their lives, the more likely they are to stay healthy.
Make new friends
Volunteering helps people meet others and develop new relationships. One of the best ways to make new friends and strengthen existing relationships is to participate in a shared activity. Volunteering is a great way to meet new people with common interests as well as expand a person’s network.
We are so thankful to our incredible volunteers and to our amazing community for the outpouring of support we have received.
Cody Sinclair is the Chief Development Officer at Sheridan Memorial Hospital.

by Melanie Aksamit, Process Improvement Coordinator, and Kristopher Schamber, MD – both of Sheridan Memorial Hospital’s Internal Medicine Practice.
Tele-health. Tele-medicine. Zoom. These are terms that have been thrown around frequently in the last few months. Chances are you have either experienced one of these or know someone who has.
But what do the terms mean? Tele-health and Tele-medicine are synonymous terms given to medical care visits performed through the internet via video and audio software on a computer, smartphone, or tablet. These visits are also sometimes called virtual house calls or video visits. During these visits, you and your medical provider can see and hear each other throughout your appointment.
While a traditional in-person office visit cannot be fully replaced by telehealth visits, there are many medical conditions and appointment types that can be seen in this way. Medication follow-up, mental health, and chronic stable medical conditions can all be safely discussed during a video visit. Some conditions simply cannot be evaluated in a video visit. These include serious conditions like heart attacks, strokes, and breathing problems, or a condition that requires a physical examination. When you call to schedule an appointment, your care team will help you determine if you need to be seen in person.
During the current COVID-19 pandemic, a video visit can be a great way to see your medical provider, while staying safe in the comfort of your own home. The visits function the same basic way that your in-person visits do. A care team member will confirm your appointment, request a video visit in place of the standard office visit if appropriate, and review the necessary requirements to participate in a video visit. If you do not feel comfortable or do not have the technology to join a video visit, a telephone visit will be set up in its place. You will be sent an email containing the link to join the visit and detailed instructions on how to work the Zoom video visit program. On the day of your video visit, the office staff will call you prior to your appointment start time and confirm that you are ready, and assist you with getting online with your care team. Once it is confirmed that you are good to go, a nursing staff member will join you, and review the reason for the visit and confirm the medications you are taking. The medical provider will then join you as soon as they are finished with their prior appointment. Your provider will ask questions and discuss your concerns similar to a standard in-person visit. He or she may ask for home blood pressure measurements, or ask to view the problem area over the video, if appropriate to do so (for example, a skin rash, area of swelling, or even observe you walk). At the end of your visit, your provider will review your care plan as usual, and the nursing staff member will ensure all testing has been ordered and other medical visits have been scheduled.
A telehealth video visit can be a scary proposition when experiencing it for the first time. However, once you are connected it feels a lot like a regular office visit. If you struggle with the Zoom program when testing it prior to your visit, please call our office and we will be happy to help walk you through it. We also encourage you to have a family member or caregiver assist you, and if possible stay close by or join you during your visit.
Due to special circumstances with the COVID-19 pandemic, we are fortunate to provide this service to our patients. In the past, due to regulations, we have not been able to. If you access telehealth video visits and find the service useful and positive, please contact your local, state, and federal legislators to inform them of your experience so they might consider supporting modifications to telehealth regulations long term.

This month’s W.O.W Employee of the Month is the Women’s Clinic’s Gregg McAdoo, M.D., FACOG! Dr. McAdoo is motivated to maintain his health and wellness so that he can continue to do the activities that he loves.
“As we get older, one of the hardest struggles we have is being able to do the things that we enjoy doing. If you don’t maintain your health as much as possible you’re going to lose out on active lifestyle activities and you won’t get the most out of life. Being able to continue the activities I enjoy doing for as long in life as I can, is important to me,” said McAdoo.
Dr. McAdoo enjoys many outdoor activities including hunting and hiking.
“I enjoy active hunting with my dog: pheasant hunting, bird hunting, and elk hunting. Recently I’ve been hauling 50-pound bags of sweet feed to bait bears,” said McAdoo. “When you’re hunting and climbing the mountain you realize quickly if you haven’t maintained your health, our mountain is a humbling experience.”
When asked what advice he would give to others who are wanting to start a healthy lifestyle, he stressed the importance of balance and finding things you enjoy.
“I think picking things that you enjoy doing and will
continue doing is very important. If you don’t enjoy it and its too hard on
your body you won’t be able to continue to do it. Finding what you will do
regularly is more important than what it is,” said McAdoo.
He also has the same mentality when it comes to nutrition and finding a balance
that works for you.
“It’s about trying to balance. If kale is good for you but you don’t like it, you’re not going to keep eating it. It’s trying to find the things you enjoy and are willing to eat regularly. If you’re too rigid you’re not going to follow it. There has to be flexibility to it,” said McAdoo.
He also makes small changes to incorporate healthy habits
into his everyday life.
“Instead of reading and drinking coffee for an hour in the morning or watching
T.V. at night, go on a walk instead. You have to change and make different
decisions to stay active in life. It’s finding ways to exercise while spending
time with family, as well as finding ways to incorporate exercise and how you
eat into your life,” said McAdoo.
Dr. McAdoo says that for both activity and diet his son has been his best example.
“He’s been cooking his own meals for 6 years and rarely eats out because he’s worried about what it’s getting cooked in and how it’s prepared. As a teen he was getting me up to do P90X at 4 am before work,” said McAdoo. “I always ask myself, if he saw me eating it, would he approve?