Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
SMH Friendly Faces

When Mary Skretteberg severely broke her ankle in September 2019, the prescription of a prolonged hospital stay felt like insult added to injury for the 79-year-old. But when she was discharged two months later, she said goodbye to the staff at Sheridan Memorial Hospital’s Transitional Care Unit (TCU) with tears in her eyes.
Skretteberg was surprised by the level of community she found at the TCU, a recuperative place to heal following an injury, surgery, or serious illness. “It was kind of like a college dormitory,” she explained. “You’re sharing a space: You’re sharing the dining room, you’re sharing the therapy, and you’re sharing your pains and aches and worries.”
By the end of her stay, Skretteberg felt at home in the halls of the TCU.
Today, Skretteberg is thrilled to be home with her husband. She continues to practice physical therapy and is “on the mend.”
And she continues to think fondly of her TCU family. Skretteberg hopes the TCU is able to add more beds “because the community is growing, and once you’re 50, 55, 60 years old, you start to break an ankle here, fall there — you need some time to recover in a hospital that doesn’t feel like a hospital.
“The TCU feels like TLC.”
To learn more about Transitional Care and the current Expansion Project, visit sheridanhospital.org/foundation today!

With the COVID-19 vaccines becoming more and more available to everyone, we asked some of our health care providers why they got the vaccine and what their thoughts are for our community.
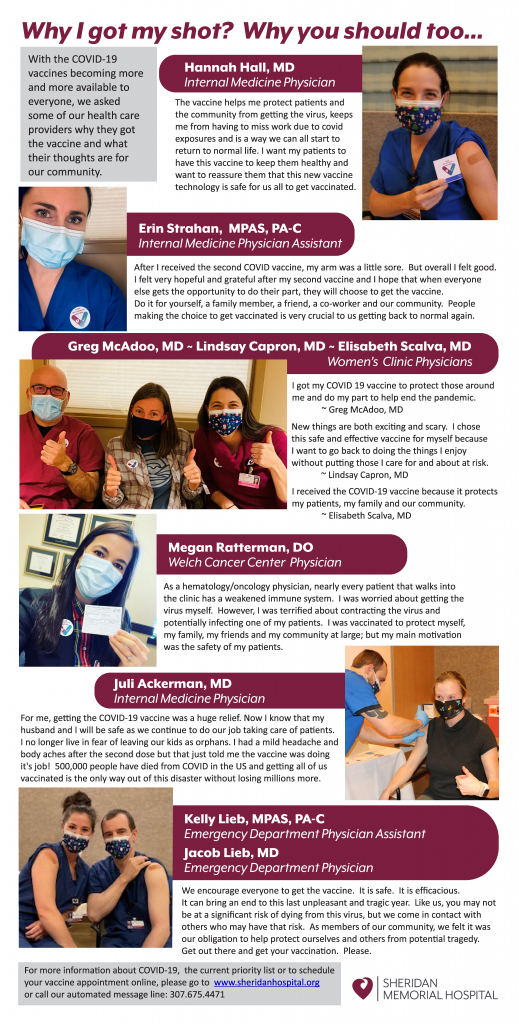
For more information about COVID-19, the current priority list or to schedule your vaccine appointment online, please go to sheridanhospital.org or call our automated message line: 307.675.4471.

It may not be the most glamorous subject, but talking about colorectal cancer saves lives. Among cancer affecting both men and women, colorectal cancer is the second leading cause of cancer-related death in the United States. Unlike many cancers, we have effective tools to help decrease the development of colorectal cancer and identify its presence at an earlier stage.
The risk of colorectal cancer increases with age, with more than 90% of the cases we see being diagnosed in people age 50 or older. There are many factors that are associated with an increased risk of colorectal cancer. Some of these risk factors are related to lifestyle choices and are therefore modifiable. Maintaining a healthy weight, being physically active, not smoking or chewing tobacco, avoiding heavy alcohol intake, and eating a balanced diet that limits intake of red or processed meat can all help decrease your risk of colorectal cancer.
Some risk factors cannot be changed. For one, colorectal cancer is more common as we age. It is also more common in people with a personal history of a certain type of colon polyp, called adenomatous, or a previous colon cancer. Being diagnosed with an inflammatory bowel disease, particularly ulcerative colitis, increases your risk. Most colorectal cancers are diagnosed in people who do not have a family history of colon cancer, but nearly 1 in 3 people who are diagnosed with colon cancer do have a family history of the disease. Only about 5% of cases of colorectal cancer are related to an inherited predisposition, but the rate of colorectal cancer is much higher in these individuals than in the general population, and it tends to develop at an earlier age. Two of the more common genetic predispositions are familial adenomatous polyposis (FAP) and hereditary non-polyposis colorectal cancer (Lynch syndrome). Although we don’t understand why, African Americans have the highest colorectal cancer incidence and mortality rates of all ethnic groups in the US.
Colorectal cancer may cause symptoms as it grows. These symptoms include seeing blood in or on your stool, unintentional weight loss, a change in bowel habits and weakness or fatigue caused by a low blood count.
Screening is the practice of looking for cancer or pre-cancer in individuals without symptoms. Screening is incredibly effective when it comes to colorectal cancer because, from the time the first abnormal cells start to develop, it takes on average 10-15 years for those cells to become a colorectal cancer. Screening is one of our most effective tools for preventing colorectal cancer because it allows us to find and remove precancerous polyps and identify people who would benefit from more frequent screening. Screening can also identify small cancers that aren’t yet big enough to produce symptoms.
There are several screening tools for colorectal cancer, including tests done on your stool, radiographic studies and colonoscopy. The stool studies either look for evidence of trace blood that isn’t enough to be seen by the naked eye or look for altered DNA that can be associated with abnormal cells in the colon. Stool studies that look for blood need to be repeated every year if negative. A negative stool DNA test needs to be repeated every three years. A CT or virtual colonoscopy is a radiographic study that involves cleaning out the colon at home and then coming into the hospital for a CT scan. If any abnormalities are seen, the study needs to be followed up with a colonoscopy at a later date. If the study is negative, it should be repeated every five years. Stool studies and virtual colonoscopy are only appropriate for patients with an average risk of colorectal cancer. A colonoscopy is a procedure that is done using a small fiber-optic tube and air to examine the lining of the colon after a prep has been completed the day before. Colonoscopy allows for the identification of polyps and removal, or biopsy if too large, at the same time as the procedure. Depending on the findings during the procedure and individual risk factors, colonoscopy may be repeated every year for high-risk individuals to a more typical range of 3-5 or 8-10 years.
Talking to your doctor about your risk factors can help identify the most effective and appropriate screening test for you. In general, screening is recommended between the ages of 50 and 75, though there are reasons to start earlier or stop later for some people. It is estimated that only about two-thirds of adults in the US are up to date with their colorectal cancer screening. Every year, about 140,000 people in the US will be diagnosed with colorectal cancer, and 50,000 people will die from it. Our best tool to decrease both of these numbers is screening. Talk to your doctor today.
Talk to your primary care provider about your risk factors. If you don’t have one, check out Sheridan Memorial Hospital’s Internal Medicine practice or call: 307.675.2650
By David Nickerson, MD – Medical Director of Sheridan Memorial Hospital’s Urgent Care
Navigating the healthcare system can be difficult. Even in a small town like Sheridan, there are multiple options for care and it may not always be clear where to start. Sheridan Memorial Hospital offers three different points of access for general medical care.
Internal Medicine
The Internal Medicine Clinic is located in the Outpatient Center at 1333 W. 5th Street and is the best location for treatment of chronic medical problems, such as high blood pressure or cholesterol, and diabetes. There is also a focus on health maintenance and prevention. The Internal Medicine Clinic uses the team model, meaning that you will have a primary doctor or advanced practice clinician but can also see one of the colleagues with whom they work closely if they are not available. In addition, patients can also be referred on to the appropriate specialist, if needed.
For the safety of patients and staff, patients with symptoms that could represent COVID-19 (Fever, chills, body aches, cough, runny nose, sore throat, vomiting, diarrhea, headache, or changes in the sense of smell or taste) are currently being referred to the Urgent Care or Emergency Department.
To make an appointment at the Internal Medicine Clinic, patients may call 307.675.2650.
Urgent Care
Sheridan Memorial Hospital’s Urgent Care recently moved to 1435 Burton Street, the former location of Bighorn Mountain Medicine. It is the ideal location for immediate treatment of new medical problems, such as colds, flu, ear/nose/throat issues, musculoskeletal injuries, skin issues, urinary problems, stomach issues, and headache. It is also the best place to be seen for non-life threatening COVID-19 concerns.
Laboratory and x-ray equipment are onsite and common prescription medications can be dispensed during your visit through local pharmacies. Finally, if you have a medical problem and are unsure where you should be seen, the Urgent Care is an excellent starting place and can refer you to a specialist or transfer you to the Emergency Department.
No appointment is necessary at the Urgent Care and you may walk in or visit www.SheridanUrgentCare.com to save your spot. The Urgent Care may also be reached at 307.675.5850.
Emergency Department
The hospital’s Emergency Department is located at 1401 West 5th Street. It is the best place for treatment of life-threatening medical problems and injuries such as heart attack, stroke, abdominal pain, dislocations, severe fractures, and severe pain. Patients are prioritized based on the severity of their condition. Onsite consultations from surgeons, cardiologists, internists, pediatricians, orthopedists, OB/GYNs, and other specialists can be obtained as appropriate, as are admissions to the hospital and transfers to larger facilities if needed.
When medical issues arise, knowing the most appropriate location to seek care can save you time and money. We wish you the best of health, but Sheridan Memorial Hospital’s outpatient services are here and ready to serve you when needed.
For more information visit Urgent Care vs Emergency Room.

By Sierra Gross Stallman, MD – Medical Director of Sheridan Memorial Hospital’s Internal Medicine Practice
We have all been affected by Covid-19, which is why we look for safe and effective ways To protect our families, communities, businesses and mental health by reducing disease burden, keep us from getting Covid-19, and allow us to resume social functions: Vaccines.
Pfizer-BioNTech and Moderna have been successful in developing Covid-19 mRNA vaccine. Researchers have been studying mRNA vaccines for decades, refining and accomplishing a standardized process for safe and timely production. Having this technology readily available to use allowed for rapid response to the pandemic in developing a safe and effective Covid-19 vaccine. Even though scientists promptly replied to demand with scaled, standardized vaccine development, mRNA vaccines have been held to the same rigorous safety and effectiveness standards as all other types of vaccines to get approval or emergency use authorization from the Food and Drug Administration (FDA).
What is mRNA? It is a messenger that provides information to our immune system. Once recognized, our immune system uses the information as a template to produce antibodies that can detect and destroy the virus causing Covid-19 for future infections. This takes the body a few weeks to complete, so it is possible that a person could be infected with the virus and get sick from Covid-19 just before or just after vaccination because the vaccine has not had enough time to provide protection. Covid-19 mRNA vaccine does not contain live virus; rather, it has harmless protein pieces found on the virus’s surface. The vaccine is given as an injection into the upper arm muscle in two doses separated by ~21 days for Pfizer and ~28 days for Moderna. This two-dose regimen conferred 95% protection against Covid-19 in persons age 16 or older. Side effects from the vaccine are similar to that of other types of vaccines and largely consistent with the appropriate response of the body’s immune system. Transient and mild local reactions such as injection site tenderness, redness, fever, fatigue, headache, and joint pain can occur. The CDC is monitoring reports of allergic reactions, and as of December 23, 2020, there were 21 cases of anaphylaxis out of 1,893,360 doses given. Anaphylaxis is a life-threatening allergic reaction that can occur rarely after vaccination, with onset usually within minutes. All reactions were treated and recovered. Worldwide there have been over 44 million vaccine doses administered in over 50 countries.
Who should get vaccinated? The goal is for everyone to get vaccinated against Covid-19 as soon as enough vaccine is available. Covid-19 can have severe complications, including hospitalization, admission to ICU, intubation or mechanical ventilation, or death, particularly to those at-risk. At-risk persons include any adult older than age 65 and adults of any age with certain underlying conditions such as obesity, type 2 diabetes mellitus, and smoking.
Due to the limited supply of vaccines around the country, Wyoming has a phased approach to ensure equity in vaccine allocation and distribution. The prioritization list can be found here and on the WY Department of Health website. Sheridan County is currently in phase 1b, including people who are 65 years of age or older. Sheridan Memorial Hospital is working closely with Public Health to distribute vaccines to our community as quickly and efficiently as possible. We anticipate it will take about two months to get through this current phase based on allocation supply.
If you fall into this category, call 307.675.4471 to schedule a vaccination time.
As always, reach out to your healthcare provider with questions or concerns regarding your health and the Covid-19 vaccine. Thank you, Sheridan, for sticking together, supporting our community, and doing your part to reduce the spread.

By Charlotte Walter, PT, DPT, ATC – Wyoming Rehab
If there’s one thing we can all agree on, it’s that 2020 was not the year we expected. Increased stressors and disrupted schedules are often accompanied by decreased exercise consistency and other poor health habits. Once bumped off the wagon, it can be difficult to dust ourselves off and clamber back up. If 2020 knocked you off your fitness routine or reminded you of the importance of starting one, read on.
A common barrier for individuals wanting to start an exercise routine is joint pain or stiffness. Luckily, exercising the right way has actually been shown to decrease these symptoms. To avoid flaring up joint pain, it is important to start smart. Take an honest assessment of your current exercise levels – if you are not currently exercising at all, jumping into a six-days-a-week-60-minutes-a-day high-intensity exercise program will cause a significant increase of joint loading. Instead, start by incorporating low-impact cardiovascular activities such as walking, dancing, cycling, swimming, cross-country skiing, or rowing with gradual increase in duration.
Strength training is another joint-friendly activity that strengthens the muscles surrounding the joint, which in turn will support the joint and reduce joint stresses. Good news is you don’t need a full gym set-up to get a good workout! Using bodyweight, resistance bands, or free weights can still load muscle groups enough to induce strength gains. No free weights around the house? Get creative with empty milk or water jugs filled with water, sand, or rocks.
Flexibility exercises are an excellent complement to aerobic and strength training activities. Moving a joint through its full available range of motion encourages circulation of joint fluid and helps to reduce joint stiffness. Gentle stretching or yoga routines are a great way to work this in.
Keep in mind, exercise is just a piece of the fitness puzzle. An effective workout is hard to achieve if you are short on sleep, hydration, or nutrition. Start smart and make small, sustainable changes that will have a long-term positive impact on your health. Additional sources of information about physical activity can be found from the CDC, the American Heart Association, the Department for Health and Human Services, and others.
Does all of this sound great, but you’re unsure of where to start? As with any new exercise program, you should consult your doctor to address any medical concerns that could limit exercise before beginning. If you have medical clearance but are stumped by persistent pain, previous injury, or balance concerns, take advantage of your knowledgeable sports medicine and orthopedic therapy team at Wyoming Rehab! Our therapists offer FREE screens and treatment recommendations on non-emergent physical impairments or injuries. Don’t let those aches and pains hold you back. The therapists at Wyoming Rehab can help guide you in the right direction to get your 2021 on track.
Armed with the right knowledge and a desire to improve our levels of health, there’s no reason to not make 2021 the comeback year we all need.
Find out more about what Wyoming Rehab can do for you: https://www.sheridanhospital.org/medical-services/rehabilitation-services/

On Friday, January 8, 2021, the Sheridan Memorial Hospital Auxiliary voted unanimously to pledge $50,000 to the Transitional Care Expansion at Sheridan Memorial Hospital. With this gift, the Auxiliary has given $724,000 to Sheridan Memorial Hospital since 1991.
With a mission “to provide comfort to and better the welfare of Sheridan Memorial Hospital’s patients,” The Auxiliary Board members voted on the opportunity that best exemplified their purpose. This year’s funds will impact patient care throughout the hospital by going to the Transitional Care Unit (TCU), as this service is a multi-disciplinary team made numerous departments. The TCU team includes Nursing, Physical, Occupational, Speech and Respiratory Therapy, Case Management and Social Services, Nutritional Services, Wound Care, and more.
Foundation Director of Donor Relations – Ada Kirven, Development Coordinator – Jasmine Slater, and Chief Development Officer – Cody Sinclair gratefully accepted the gift presented on behalf of the numerous departments who will be positively impacted by this contribution. The photo includes Foundation Director of Donor Relations – Ada Kirven, Auxiliary Board Members Linda Sutphin, Ann Kilpatrick, Jill Mitchell, Sandy Pilch, Karen Steir, Ethelyn St. John, Maurita Meehan, Stella Montano, and Development Coordinator Jasmine Slater.
“We appreciate the time spent coordinating and working alongside this generous and passionate board of volunteers,” explains Chief Development Officer Cody Sinclair. “This donation is part of a long Auxiliary tradition in continuing to support hospital & Foundation projects that will expand the healthcare available to our community. These women continue to help enhance the patient experience throughout the entire organization, and we are so fortunate to be able to collaborate with such an incredible group.”
To learn more about getting involved in The Sheridan Memorial Hospital Auxiliary Board or Volunteering, please reach out to Development Coordinator Jasmine Slater at 307.675.2620 or by clicking here.

The Sheridan Memorial Hospital Foundation is excited to announce its Transforming Transitional Care Campaign. A Transitional Care Unit (TCU) is a recuperative and supportive place to heal following an injury, surgery, or serious illness. From changes to one’s daily schedule to the adjustments necessary to return home – the care team of nurses, doctors, and therapists manage transitions and help patients regain a level of independence for a safe return home.
Our aging population and the increased need for Transitional Care in our community, led to the design of this project. It will increase the number of patients the hospital is able to offer this specialized care to, before they transition back home. Our community is changing and Sheridan Memorial Hospital wants to ensure the growing number of patients needing transitional care will have the opportunity to stay right here in Sheridan, close to home and family.
“The Foundation is thrilled to support the hospital in repurposing the 2nd and 3rd floors of the main 1954 hospital back to their original use—caring for patients and providing excellent care,” said Chief Development Officer Cody Sinclair. “Meeting the needs of our community through this expansion will also ensure our community hospital is prepared for any future pandemic.” The space was cleared immediately for pandemic care last year, and Sheridan Memorial Hospital applied for the CARES Act funding available through the Wyoming State Loan and Investment Board (SLIB). A grant of $2.1 million made the completion of initial infrastructure and demolition construction possible before December 15.
The Foundation met with community members and local foundations about the project in October, and gained support and momentum to meet the $4.4 million goal. We now look forward to sharing more information with everyone in our region, and raise the remaining 20% needed to begin construction in July. “The response from our community this past year, through COVID and now excitement over this campaign has been truly remarkable,” said Director of Donor Relations Ada Kirven. “Throughout the pandemic we have been fortunate to have the donors, staff, and resources available to support the community – including the ICU that many of these same major donors supported five years ago. We are grateful for our initial contributions as they have shown they believe in the need for the project and laid the foundation for a successful completion. It’s remarkable to bring an expansion like TCU to our community and expand care for our growing and aging population at such a critical time.”
To learn more about the Transforming Transitional Care Campaign or The Foundation, call our offices at 307.673.2418 or visit us at sheridanhosital.org/foundation.
Through January 22, Sheridan Memorial Hospital (SMH) has provided COVID-19 vaccinations to approximately 1,000 people in Sheridan County. That includes SMH employees and the priority populations of essential workers and people over the age of 70.
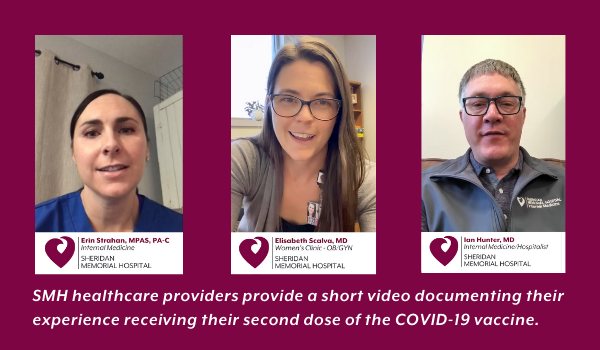
The side effects from the second dose of the vaccination received can include arm soreness at the injection site, minor swelling, chills, fever, fatigue and headaches. A few SMH providers have provided a short video documenting their experience receiving their second dose.
“I’m feeling hopeful, and very grateful,” said Erin Strahan, PA-C with the SMH Internal Medicine Clinic. “This is one chance to get back to normal life.”
“I have a little soreness in my arm but nothing that kept me from seeing my full complement of patients,” explains Dr. Elisabeth Scalva, with the SMH Women’s Clinic. “I’m feeling grateful to be protected and to protect my family, my patients and mostly this community.”
“Initially, I had a little bit of a sore arm,” said Dr. Ian Hunter, Sheridan County Public Health Officer. “Later that night, I woke up and had a fever… I just didn’t feel good for about eight hours, then that resolved.”
Currently, all doses of the vaccine SMH has received or is scheduled to receive is already spoken for. This includes 975 doses of the Pfizer vaccine scheduled for delivery on January 25 or 26.
SMH is accepting calls to place essential workers and people over age 70 on a wait list. Once more information is available regarding additional vaccine, SMH will be working through the wait list to conduct call backs and schedule additional vaccination appointments.
If you have been designated an essential worker or are over the age of 70 and you want to receive the vaccine, please call 307-675-4471 and leave your name, date of birth and phone number. You will receive a call back within the next business day to be placed on the wait list.
Click here for more information on the COVID-19 vaccine in Sheridan County
Click here for the Wyoming Department of Health Phase 1a and 1b COVID Vaccination Priority List

The past year has been a remarkable one for all of us to reflect on. Be it personal or professional; we have faced our own set of challenges that could not have been anticipated 12 months ago. But together, we are now able to identify silver linings, learn from the past, and move forward with gratitude for all that we have been given in time, love, health, and hope for the future.
The Sheridan Memorial Hospital Foundation and Hospital team members had a year we will never forget. The work of our board, donors, and volunteers allows support for exceptional staff, departments, and services at your community hospital. Our donors continue to support opportunities, innovation, and patient-care experiences with their generosity. The nature of these services shifts and changes day-to-day for our teams in our current climate, but we appreciate the opportunity each day to come to work and support the people who choose SMH for their healthcare needs. Our supporters’ tireless efforts are what made it possible for our teams to take care of each – bump, scrape, scan, screening, teleconsultation, birth plan, heart palpitation, allergy shot, common cold, broken bone, and emergency call – on top of all involved in caring for our COVID patients.
An organization’s annual report is meant to share with each of you the contributions received throughout the last fiscal year and how those funds have been put to work. The Foundation’s Gratitude Report is a mere snapshot into the previous 12 months and all of the lives our donors positively change because of their kind and caring actions.
Our Foundation Staff recognizes that in no way could we incorporate all stories to completely capture the outpouring of support, kindness, and generosity we are surrounded by. We take this opportunity to share some of the life-changing efforts, the remarkable tales, and the infinite gratitude we feel for you, our donors, who’ve filled our hearts and hallways over the last 365 days and now into the New Year. Thank you for being a part of our story.
We invite you to share in our full 2020 Gratitude Report by experiencing it here (https://www.sheridanhospital.org/wp-content/uploads/2021/01/2020-Gratitude-Report.pdf).

Each year, Sheridan Memorial Hospital (SMH) employees find ways to give back to the community; 2020 was no different… um, wait, yes it was.
“The generosity and support we received from the community this past year were like nothing we have ever witnessed,” said Cody Sinclair, SMH Chief Development Officer. “It was a great feeling to be able to continue with the traditional fundraisers and food drives we normally have throughout the year. It paled in comparison to the community support we received, for sure. But our employees still stepped up.”
During a year filled with uncertainty, long hours, double shifts, 24-7 masks, head to toe PPE, and lack of social connection due to COVID-19, SMH employees still found a way to contribute.
“We’re proud of the way our employees have responded to all the challenges of COVID-19, and these efforts show how much they really care for this community,” Sinclair added.
Here are some of the various efforts that hospital staff and departments participated in or initiated this past year.
SMH Foundation Employee Partner Program – over 514 employee partners raised over $47,700 in 2020 to provide additional funding for the hospital’s Transitional Care Unit expansion which is currently underway. Over the past 17 years, SMH employee partners have contributed over $500,000 to projects at our community hospital.
Patient Access and Admissions Department – collected food for the People Assistance Food Bank and cash for the Salvation Army over the holidays.
Women’s Health Department – collected toys for Toys for Tots during their annual Christmas toy drive.
Marketing Department – Volunteered to help organize and re-stock food supplies at The Food Group.
Patient Accounts Department – conducted a food and toy drive for Christmas. Food was donated to the People Assistance Food Bank and toys were donated to Toys for Tots.
Internal Medicine Practice – Employees provided gifts for 45 children of patients in the Addiction Medicine Clinic for Christmas.
All SMH Employees – Specific Fridays throughout the year are designated as “Jeans Friday” at SMH. Employees are encouraged to donate $5 for the privilege of wearing jeans on that day and $1,840 was raised from this effort. The funds were distributed among the following causes:
- The Link Partners in Pink
- Kozy Korner Gift program that purchases gifts for those in the hospital on Christmas
- Sheridan Media Christmas Wish Campaign
- Salvation Army
All SMH Employees – 2020 COVID-19 Employees Give Back – Food drive to collect non-perishable items for the People Assistance Food Bank, the Food Group and the Salvation Army.

Wyoming Rehab’s Licensed Physical Therapist Charlotte Walter describes her approach to creating individualized treatment plans to help each patient achieve their goals. In this video, she highlights a treatment plan she created for Pat Hall, who came to Wyoming Rehab with concerns of balance and mobility.
Do you have a condition or impairment preventing you from reaching the recommended amounts of physical activity? Don’t continue to put your health at risk. Find out how physical or occupational therapy may help. Reach out to Wyoming Rehab at 307.674.1632 if you would like to schedule a FREE Screen/Treatment Recommendation for a Non-Emergent Physical Impairment or Injury.

Connie Bachel, a longtime employee of Sheridan Memorial Hospital (SMH), contracted COVID-19 in mid-September.
Bachel and six of her co-workers at the SMH Urgent Care tested positive for the coronavirus, each exhibiting different symptoms. For the next two weeks, they recovered, checking in on each other’s progress and offering words of encouragement.
In early October, Bachel was feeling better, if not fully energized. But by mid-October, COVID-19 reasserted itself in full force, even worse than before. Bachel, suffering from gastrointestinal symptoms, did not immediately want to go to the emergency room.
“It was so embarrassing — I didn’t want to do that in my own sandbox,” she said. “But my husband said, ‘No, you’re going to have to be a patient.’”
Bachel was immediately admitted and placed in a COVID-19 isolation wing.
SMH has two dedicated wings for COVID-19 patients: one in the Intensive Care Unit for critically ill patients and the other on the Med Surg floor for those like Bachel who need to be admitted but don’t need ventilators. Experts across SMH departments have worked together to ensure these wings are as safe as possible for patients and staff.
“It’s very scientific,” said Lacey Johnson, the Med Surg Manager at SMH.
Because COVID-19 is an air-borne disease, Johnson explained, one of the most important elements of the isolation wings is the air flow. Partitioned off from the rest of the hospital, the hallways and rooms have negative air pressure. Instead of filtering, cleaning, and recirculating the air like in most buildings, the mechanics of the hospital bring in air and then send it directly back outdoors, without returning to the hospital. All doors and windows must remain closed to maintain the seal.
In addition, the few dedicated staff members who are allowed into the wings must be in full PPE: gown, gloves, booties, N-95 mask, eye cover, and hair bonnet or a capper.
The cleaning staff for the COVID-19 wings uses “terminal cleaning” agents and gear, the same used in Operating Rooms, a lengthier and more involved sterilizing process.
Perhaps most importantly, the medical team must be conscientious of the time spent in the wings.
“If we go in to deliver medications, we get them all at once,” Johnson said. “We bathe patients, change the bed, etcetera, all in that time frame.”
While crucial for safety, the COVID-19 isolation wings can be just that — isolating.
At the time, Bachel’s daughter, Megan Perkins, was a registered nurse at SMH. Due to the strict safety protocols, even she could not enter the room — only the dedicated on-duty nurse could be admitted.
Perkins herself had worked in the COVID-19 wing. She had seen family members’ frustration at being kept apart and knew the importance of lifting patients’ spirits when at their most ill.
“As a nurse, it’s hard to see your patients struggle that way,” Perkins said. “I saw how much it dropped their mood and their affect. It hurts people’s sense of well-being when they’re so isolated. But I knew why we were doing it and that it had to be done. Just from taking care of previous COVID patients, I knew what my mom was going through.”
So, like many of her patients’ family members, Perkins found a safe way to engage with her mom. Bundling up against the October snowstorm, Perkins headed to the window outside of her mom’s room.
“I called her on the phone, and we sat by the window and drank coffee and pretended the window wasn’t there,” Perkins remembered.
Over the next few days, these chats meant the world to Bachel. And the support continued to flow. Friends, family, and co-workers visited — even her daughter’s friends popped by to throw snowballs and wave an encouraging sign out of the window.
“It means more to the people in that hospital bed than you know,” Bachel said, choking up.
After four days of treatment, Bachel showed improvement, tested negative for the contagious antigen, and was released to recuperate at home for another week. She gradually started working again, building up her hours and strength slowly.
Today, Bachel feels “100% completely better.” When she looks back at the fall, she realizes just how ill she was.
“After about a month and a half of being so sick, when you do finally feel good, you realize just how terrible you felt,” she said. “I’m so glad I went in because I don’t know what would have happened. They took great care of me.”
Back at work, Bachel — already a compassionate person — feels even more empathy for patients and family members after her experience. She sees the same change in her co-workers who also recovered from the disease.
“I know how they feel,” Bachel said. “I feel it. It’s real. We all need to wear our mask and practice hygiene. It’s just here. It’s here all the time.”
Her daughter agrees.
“I just hope that people understand what these regulations are for and what the mask mandates mean for certain people,” Perkins said. “Until it becomes personal for you, you don’t really take it to heart. Until you realize one of these patients is a mother or a grandmother — because one was your mother — you just don’t realize the detrimental effects. I think all the people who make a stink about our mask mandates need to take a step back and realize it’s about being a good person.”

By Erica Ridgeway, BSN, RN – Sheridan Memorial Hospital Trauma Program Coordinator
Sheridan Memorial Hospital’s Trauma Program reviews cases for patients who have suffered a trauma of any kind. Along with this, we review and develop policies and protocols to ensure best practices are followed and that each traumatic injury receives the most appropriate care. We also work to provide education about current policies, changes in policies, and changes in best practices. This includes doing community outreach and information related to injury prevention. By following these protocols, Sheridan Memorial Hospital has earned the designation as an Area Trauma Hospital from the Wyoming State Trauma office.
Injury prevention is an important part of a successful trauma program. One of the most common traumatic injuries in any trauma registry are falls resulting in fractures, therefore making fall prevention and safety extremely important.
The National Coalition on Aging notes that one in four Americans aged 65+ falls each year. Falls are the leading cause of fatal injury in older adults and are the most common cause of trauma-related hospitalizations for that population as well.
According to the Centers for Disease Control and Prevention, one out of five falls results in a serious injury such as a broken bone or a head injury. More than 95% of hip fractures are caused by falling.
There are many conditions that can increase the risk of falls:
- Lower body weakness & impaired balance: As we age, many of us lose some coordination, balance and flexibility, oftentimes due to inactivity.
- Use of medications: Some prescription and even over-the-counter medications can cause dizziness and dehydration, making you more likely to fall.
- Vision problems and changes: In the aging eye, less light reaches the retina, thus making tripping hazards and obstacles harder to see.
If you have concerns about falling or other issues, schedule an appointment to talk to your doctor or healthcare provider. They can evaluate your risk of falling and help implement specific things you can do. They can also refer you to a physical or occupational therapist who can help with balance and strength training. Tai Chi is an exercise that is often taught to help with balance and stability. There are many fitness programs offered both in-person and virtually that are designed for older adults. Additionally, some physical or occupational therapists will even come into your home and help assess safety and tripping hazards.
If you have had a fall or have a nagging ache, pain or physical impairment preventing you from going about your daily activities, Sheridan Memorial Hospital’s Wyoming Rehab may be able to help you. Their physical therapists offer free screens and treatment recommendations for non-emergent physical impairments and injuries.
Some things you may want to consider implementing in your home include:
- Get rid of things you could trip over and reduce clutter; rugs, in particular, can cause falls.
- Add grab bars inside and outside your tub or shower and next to the toilet.
- Put railings on both sides of stairs.
- Make sure your home has lots of light by adding more or brighter light bulbs.
- As the weather is getting colder, make sure you have appropriate footwear with a good grip.
- Devise a plan with family or friends for snow and ice removal around your home’s exterior.
So again, reach out to your healthcare team! They can assess not only your risk of falling but also what steps to take to prevent a fall, as well as assess your ability to participate in a fitness program. Implementing the appropriate safety and health measures can greatly reduce your risk of falls and injury.

Diabetes is different for everyone, at every age. As we celebrate National Diabetes Awareness Month, SMH focuses on the impacts diabetes has on one’s life and the challenges faced. Meet our own smiley, sweet Megan Ripley who works as a Chemo Nurse at Welch Cancer Center. Megan shared with us her Wellness Journey, with Diabetes, and we find it an important one to share with all of you as we navigate this month, together.
While many of us prepare for cranberry sauce, sweet potatoes, and copious amounts of pie, one-third of the US populations is concerned with managing their blood sugar while still enjoying their meal. With much to be grateful for this time of year, we take a moment to appreciate the stories and knowledge surrounding the staff at Sheridan Memorial Hospital. This Diabetes Awareness month, we are excited to share with you how one of our own employees faces and maintains her wellness while facing the everyday realities of Type 1 Diabetes. Megan Ripley is an employee who has not only pursued wellness as a hobby, but has adopted it as her way of life. Even though she has to navigate through obstacles every day, from constantly maintaining healthy blood sugar levels to the everyday challenges of being a Chemo Registered Nurse, Megan strives to maintain her health and she does it all with a beaming smile on her face.
Megan Smith’s journey towards wellness started at the early age of 9, when she was diagnosed with Type 1 Diabetes. Type 1 Diabetes is a chronic condition in which the pancreas produces little or no insulin, a hormone needed to allow sugar to enter cells in order to produce energy. At the discovery of her condition, she feared how diabetes might affect her everyday life. Megan often wondered about what restrictions she would have to implement into her daily routine, or what opportunities she might miss out on because of her condition. However, Megan was fortunate enough to grow up just outside of Cheyenne during her early childhood and because of this, she was able to attend the Barbara Davis Center for Childhood Diabetes. “The doctors and nurses at the center were great and they always had the most cutting edge technology so I was able to get the best treatment possible” Megan shares. The Barbara Davis Center didn’t just have an impact on Megan’s physical health, but they were also able to provide her with tools to help maintain and enhance her mental health. Megan explained “I always wanted to grow up to become a nurse, but with my diabetes, I didn’t know if that would ever be possible. When the nurses in the center found out this was a fear of mine, many came forward to share with me that they too suffered from diabetes, and they showed me how they navigated throughout their day as a nurse with diabetes. The team showed me that I could still be the person I dreamed of becoming and I really can’t thank them enough for all the help they have given me throughout the years.”
The team at the Barbara Davis Center helped to give Megan the confidence that she could still live the life she wanted, but now she needed to figure out how she was going to balance it all. Megan went to work finding what other methods and tools she could use in her life to stay healthy and happy. One of the struggles that Megan was immediately faced with was what kind of exercise regimens she could use. High Intensity Exercise wasn’t on option because even if Megan liked it in the first place, and she didn’t, it could cause complications with her blood sugar due to Adrenaline production. You see, when Adrenaline (Epinephrine) is released from nerve endings or the Adrenals it acts on the liver, promoting increased sugar production as well as the breakdown and release of fat nutrients which travel to the liver and are converted into sugar and ketones. Simply put, Adrenaline raises blood sugar considerably, which for diabetics such as Megan who can’t naturally produce insulin, can lead to Hyperglycemia, causing damage to the vessels that supply blood to vital organs. So any strenuous exercise that would cause a spike in Adrenaline was unsafe for Megan to participate in. And if that wasn’t a large enough hurdle, Megan also was trying to find a way to manage her diet so that she could still enjoy all the foods she enjoyed so dearly, without causing massive spikes or falls in her blood sugar levels.
Megan was committed to finding a solution. She knew what a great influence exercise and diet would have on her physical and mental state, so she never quit looking for answers. Eventually, she found resolution to her exercise dilemma when she realized just how much she liked doing long-distance, moderately paced cardio. Walking, hiking, and biking were also activities that Megan loved doing because they could be done with others. None of them required going to a gym, none of them would produce adrenaline if paced correctly, and all of them promoted muscle growth and weight loss. As for her diet, Megan discovered portion control, a dieting strategy that she could utilize in order to keep eating her favorite foods, by simply adjusting and managing the portion sizes of her meals throughout the day
Once Megan knew how she was going to balance her exercise and diet, all she had to do was find a way to consistently motivate herself to continue eating healthy and exercising on a regular basis. Her motivation to stick to her diet is basic: “If I eat right and stick to my diet then I can stay healthy, but if I’m not willing to maintain my diet then my physical health will be seriously negatively affected.” Megan’s motivation to exercise is a little less cut and dry. Megan relies, for the most part, on friends and family to help her stay motivated throughout the week. On week days, Megan’s biggest motivator is her Dog Laya who is always eager to remind her about their daily walk together, they rarely miss a day, considering Laya is known to not taking no for an answer. A few days a week Megan also gets the opportunity to go on walks with friends from work, who she also credits as being some of her greatest supporters. On the weekends, Megan is motivated by excitement and adventure with her husband John and of course, Laya. Megan is always eager to plan out her family’s adventures and you can bet they’ll be doing a whole lot of hiking, canoeing, backpacking, or fishing with a whole lot of fruit snacks to keep her fueled. Megan’s most recent adventure sent her on a rigorous 16 mile hike, with almost 2450’ vertical gain to the beautiful and secluded Lake Angeline, high in the Bighorn Mountains.
Megan’s advice to all those who have a desire to get well was this: “Start small and set goals that are attainable, all of us progress at our own rate and your rate is completely unique to you, so don’t compare yourself to anybody but yourself. If you need a donut, then eat a donut, but eat less of something else or just exercise more to compensate for it. It’s all about balance. Do not underestimate the power of thinking positively, mental health is just as important as physical health, and being happy and thinking positively can take you just as far as any workout routine.”
We’re so very proud to see how far Megan has come from where she once was and we can’t to see where she goes. We’d like to thank Megan for her inspiring story and providing such positive insight into living a balanced life with Type 1 Diabetes. We appreciate you leading by example and for showing us all what it really means to take wellness into our own hands. Sheridan Memorial Hospital honored to have you as a member of our staff and we are grateful for everything you have done and continue to do for this hospital. Thank you, Megan.

The Sheridan Memorial Hospital Foundation Staff and Board of Directors are pleased to announce J.T. Grainger as their newest Director, voted unanimously to the board during their September 2020 Board Meeting.
Board President Richard Garber shares, “we are thrilled to welcome J.T. to our Foundation Board of Directors. In my time spent with J.T., it is evident that he is a driven, philanthropic, outgoing individual who is going to bring great insight and energy to our board.” Along with the officers and directors, Foundation staff share in the excitement to welcome J.T. as part of the board. “J.T. is a passionate, motivated individual that is an outstanding addition to our well-rounded board,” explains Chief Development Officer Cody Sinclair. “J.T. shares his excitement and passion with individuals of all ages and wants to help develop this community positively for the generations to come. He has already shown initiative in learning more about Sheridan Memorial Hospital and the work of The Foundation and how he can make a strong impact.”
J.T. is a Wyoming native that understands the importance of rural healthcare, having grown up in the small town of Saratoga, Wyoming, eventually ending up in Sheridan two years ago. J.T. currently manages shipping operations for Vacutech LLC, operates a flight school at the Sheridan Airport, and is the Vice President of the Sheridan Pilot’s Association – a non-profit organization committed to improving access to flying for aviation enthusiasts of all ages. When his wheels are on the ground, J.T. spends time appreciating all that Wyoming has to offer. From hunting and fishing to golfing and volunteering, he finds plenty to keep him busy on the land and in the clouds. Beyond his new adventure with The Foundation, Mr. Grainger is involved in The Sheridan County Chamber of Commerce and local chapters of Lions Club, Experimental Aircraft Association, National Wild Turkey Federation, Mule Deer Foundation, and Elk Foundation.
With all the exciting projects and work The Foundation is doing, someone who likes to keep moving is a perfect fit for the board. The Foundation looks forward to the experience, energy, and perspective J.T. will bring to the board in the coming year and all we will accomplish for healthcare in our community – together.
To get the most up to date Foundation information and learn more about The Board of Directors, visit sheridanhospital.org/foundation or call Director of Donor Relations – Ada Kirven at 673.2417.

Your first impression when meeting Dr. Elise Sylar, the newest addition to the Internal Medicine team at Sheridan Memorial Hospital, may be that she is sharp as a tack. But the more you get to know her, the more you’ll come to realize that her heart is just as strong as her intellect. And although she may be brand-new to SMH, it’s clear that Dr. Sylar is by no means new to loving and serving the people around her.
Elise’s interest in healthcare began when she started volunteering at Camp Wapiyapi, a summer camp for children who have pediatric cancer in Estes Park, Colorado. There, Dr. Sylar formed close connections with campers and had the opportunity to leave a lasting, positive impact on the lives of the kids she interacted with. The experiences and memories Elise got from Camp Wapiyapi stirred an even greater desire to help and make a difference in the lives of others. So, when the time came for her to head to new horizons, Dr. Sylar was intent on entering the medical field, with hopes of specializing in pediatrics.
Following her graduation from Kelly Walsh High School, Dr. Sylar packed up and headed from her hometown of Casper to Laramie to attend The University of Wyoming, where she graduated with a degree in Physiology and a minor in Neurology. Before moving on to Med school, Dr. Sylar took a year to get some hands-on experience at the National Institutes of Health in Bethesda, Maryland, researching CAR T-Cell Therapy in an Oncology Lab working to find a cure for Childhood Acute Lymphoblastic Leukemia.
Dr. Sylar then applied and was accepted into the University of Washington School of Medicine, and thanks to the WWAMI program, Dr. Sylar got to complete her first year of med school in Laramie. During her attendance at Med School in both Laramie and Seattle, Dr. Sylar was given the opportunity to study and practice in all fields of medicine. When the time came to decide what she was going to specialize in, she decided against her original idea of pediatrics. Dr. Sylar explained, “I always thought I was going to go into pediatrics, even when I finished studying at UW. I was certain I wanted to become a Pediatric Oncologist. Still, the longer I studied at the University of Washington, the more I realized why adult medicine was a much better fit for me. My favorite part of healthcare is to form that connection between physician and patient. It’s empowering to see people become more knowledgeable and further involved in their healthcare thanks to the advice and resources that I can provide them. The problem I had with becoming a pediatrician was I knew forming a good connection with a child would be a much more difficult process than with an adult. I also wouldn’t be able to see my patients take an active role in their health because they simply don’t have the ability to be independent the way adults do.”
Dr. Sylar finished up Med School with a focus on Internal Medicine, and now, and after finishing her 3-year residency at the University of Arizona, she’s excited to get started building relationships with her patients right here in Sheridan.
Dr. Sylar shared, “I was always planning on coming back to Wyoming after I finished my schooling, in part because of the WWAMI program, but more than anything, the reason I came back was that I wanted to give back. I felt like supporting rural healthcare was the best way I could give back to the state that has provided me with so much throughout my life.”
Sheridan became the ideal community for Dr. Sylar because it suited both her needs and her spouse’s needs. “Sheridan Memorial Hospital offers a very robust healthcare system, which surprised me considering how rural the community is, it houses lots of innovative technology and offers practices which you wouldn’t typically find in rural communities, like vascular surgery, for example. It feels like the perfect place for me to begin my career, and since Sheridan houses a reasonably sized airport, it provides my husband the opportunity to continue his career as a pilot,” she added.
Outside of her profession, Dr. Sylar loves to spend her time hiking, mountain biking, and road cycling. And with the Big Horn Mountains just a few miles outside of town, it seems like Sheridan truly is the perfect place for her and her husband Ken to both work hard and play hard.
“I’m so excited for the opportunity I have to make a positive impact on the health and wellbeing of the people here in Sheridan. And I’m even more excited to start building great relationships, not only with my patients but with all the kind and welcoming people here at SMH.”
Call 307.675.2650 and choose Option 4 to schedule your appointment with Dr. Elise Sylar in Internal Medicine today.

October is National Physical Therapy Month. Did you know that Wyoming Rehab provides FREE Screens and Treatment Recommendation on Non-Emergent Physical Impairments/Injuries? The therapists at Wyoming Rehab want to provide you with some tips for living a healthier life.
Physical activity can significantly impact your long-term health. A study published in the July 2020 edition of the British Medical Journal reported that physical activity is key.
People who regularly get 150 minutes of moderate exercise or 75 minutes of vigorous exercise per week, along with 2 days of strength training, are more likely to live a longer, healthier life.
Here are some simple examples to help you get the exercise you need…
Moderate intensity: you can talk but not sing during the activities such as:
- Walking briskly
- Water aerobics
- Bicycling slower than 10 miles per hour on primarily level terrain
- Doubles tennis
Vigorous intensity: you cannot say more than a few words without having to pause to take a breath during activities such as:
- Race walking, jogging, or running
- Swimming laps
- Bicycling over 10 miles per hour with hills
- Singles tennis
- Aerobic dancing
- Hiking uphill or with a heavy backpack
Strength training: two days per week involves exercises specifically-designed to fatigue muscle groups using weights or other resistance. You can also use your body weight for resistance by doing push-ups, pull-ups, crunches, leg squats or push-ups against a wall.
Do you have a condition or impairment preventing you from reaching the recommended amounts of physical activity? Don’t continue to put your health at risk! Find out how physical or occupational therapy may help.
Reach out to Wyoming Rehab at (307) 674-1632 if you would like to schedule a FREE Screen/Treatment Recommendation for a Non-Emergent Physical Impairment or Injury.

by Lacey Johnson, MSN, RN, Medical-Surgical Manager at Sheridan Memorial Hospital
TCU is, most often, a short-term care facility for medically complex patients who are transitioning from the hospital to home. At Sheridan Memorial Hospital, our TCU is designed to provide rehabilitation and skilled nursing care to ensure you are meeting your goals to be successful when you go home.
The journey towards TCU typically begins with an acute inpatient stay. Whether you are recovering from injury, illness, surgery, or disability, our TCU has a team of therapists, nurses and Case Management staff who are here to assist you in your recovery. Focusing on a patient’s recovery to return to independence and go back home is a goal of the unit.
The benefit of the TCU is that it provides coordination and continuity during transitions between different locations or levels of care. The TCU bridges the gap between various providers, services and settings, ideally providing education about the next stage of recovery for the patient and their family and caregivers.
Our TCU is hospital-based, unlike community-based subacute care facilities, the team of professionals is present 24-7 to collaboratively answer questions and change your care plan as needed.
How it works:
Following a qualifying hospitalization, your physician may recommend that you receive additional skilled nursing care to assure a safe transition back to your home or other living arrangement. The Case Manager speaks with you about your options for skilled nursing, where you make your choice. Once you make that decision, the transition of care begins. The nursing staff works to create your care plan and goals for TCU. Once that is completed, you are moved to the TCU area, where you begin your journey to recovery and strength.

During your stay in TCU, your care is personalized to fit your needs and goals. On a daily basis, your goals and current state are discussed with you, your family, therapist, nursing and Case Management. If you do not feel you are meeting your goals, your care plan is adjusted to move toward success.
Opportunities in the TCU include rehabilitation with some of the best Physical Therapists, Occupational Therapists, Speech Therapists and Nurses. The staff focuses on teaching skills and activities that are needed to prepare for the transition to home including: cooking and baking in the TCU kitchen, completing laundry tasks in the laundry room, exercising either in the therapy gym or outside on the beautiful SMH campus, and practicing entering and exiting a vehicle. Prior to the patient’s discharge, home visits are scheduled. These home visits are a perfect way for the care team to determine, with you and your family, the barriers you may have at home. The team then adds those barriers to your care plan while in TCU for the team to work with you to overcome them for a safe transition home.

Giving back to the community in which you live can be very rewarding. For those who have done it, you know how it feels and what it means to give of your time and talents.
Dr. Kristopher Schamber says, “I want to help; and when someone asks, if I feel I am capable of doing the task, I want to make a difference.”
This kind of positive community attitude, along with his expertise as a physician at Sheridan Memorial Hospital’s Internal Medicine, has led to recognition for the doc.
The American College of Physicians (ACP) recently bestowed on Schamber the designation of Fellow, or FACP, a designation honoring the work he does with his patients as well as in his community.
“It is an honor and distinguishing to be a Fellow of the ACP,” Schamber said. “This recognizes the work we do outside of the workplace, throughout the community, as well as excellence in medicine.”
The ACP website states it this way, “ACP Fellowship is a mark of distinction representing the pinnacle of integrity, professionalism and scholarship for those who aspire to pursue careers in Internal Medicine. The most important considerations for ACP Fellowship are excellence and contributions made to both medicine and to the broader community in which the internist lives and practices.”
While Schamber knows he can’t take on every community challenge put before him, he has honed his efforts to a couple of areas.
“It is important to seek those opportunities I am passionate about and hospice care and dementia care are the two big ones for me,” he says.
That passion gave way to activities at the Senior Center (The Hub) where Schamber volunteers his time for quarterly presentations called Doc Talks and his involvement in the Dementia Friendly Program, among other activities.
“Since my days in medical school and residency, I also have a passion for helping in underserved clinics,” Schamber added. “So when the opportunity came to help at the Sheridan Health Center that was a no-brainer for me.”
To obtain this new accolade, it requires letters of recommendation from two physician colleagues. For Schamber, those two colleagues were Dr. Ian Hunter, Sheridan County Public Health Officer and physician at SMH Internal Medicine; and Dr. Robert Monger, Rheumatologist at Cheyenne Regional Medical Center, Governor of the Wyoming ACP Chapter and Clinical Dean for the Wyoming WWAMI Medical School Program.
“Dr. Schamber certainly deserves to be recognized as a Fellow of the ACP,” Hunter said. “He puts in the work, cares greatly about his patients and community to the point of action beyond his paid job. This recognition speaks to the level of competency and caring of Dr. Schamber and we are lucky to have him in our community.”
Dr. Monger also has high praise for this accomplishment, “Dr. Schamber is an outstanding physician, and being awarded FACP is a true mark of excellence because to be awarded FACP a physician is nominated by and then voted on by fellow physicians for the honor. It’s awarded to physicians who practice excellent patient care and also are involved as leaders in the physician community.”
When asked what may be on the horizon for him, Schamber humbly says he is definitely interested in leadership roles in the community in the future, but they aren’t on his immediate radar.
“Thinking about what’s next is a tough one,” he adds. “I do these things because I’m passionate about them and to help the community. I didn’t have this end in mind. I just hope this demonstrates my dedication to the field of medicine and to the community.”
“That’s not to take anything away from the other physicians in our community who work just as hard and put is just as much time, if not more,” he adds humbly.





