The Sheridan Memorial Hospital Foundation board members and staff are excited to announce, thanks to the generosity of our community; we’ve
David Nickerson, MD, urgent care physician at SMH, has completed the necessary training through the Federal Aviation Administration (FAA)
Sheridan Memorial Hospital has been advised of a
The use of natural testosterone and testosterone supplements has skyrocketed the past few years. Dr. Christopher Prior offers his insights on this
Sheridan Memorial Hospital’s Covid-19 testing is now being done at the hospital’s Urgent Care
Certified Nursing Assistants (CNAs) provide intimate, hands-on healthcare to patients. A day in the life of a CNA might include taking patients temperature, blood pressure, and other vital signs,
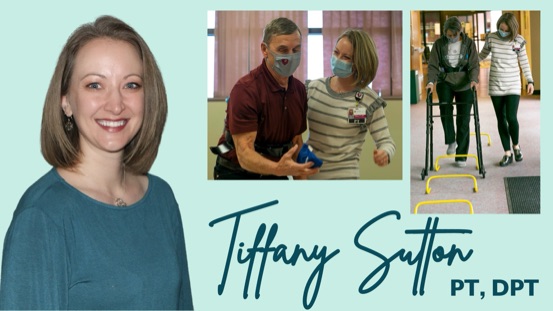
Having a comfortable, private environment to heal and regain strength and confidence for a safe
The Sheridan Memorial Hospital Foundation is matching all gifts in June to finish the Transitional Care Expansion Campaign. All gifts and pledge
Wyomingites ages 12 and up can now receive the COVID-19 vaccine, following a thorough review and decision by the FDA and CDC. More families have the ability to protect their children and return to the activities and people they love.
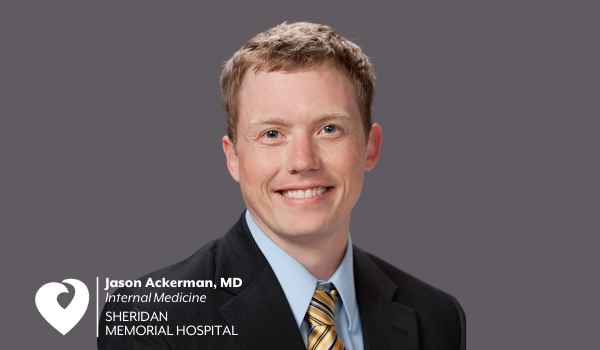
Dr. Jason Ackerman has been practicing medicine in Sheridan for the past 8 years and has been a mainstay in the Sheridan Memorial Hospital
Thanks to generous gifts from planned giving and The Link annual event participants and sponsors, the Sheridan Memorial Hospital
In our country, someone experiences a stroke every 40 seconds. This debilitating and deadly injury to the brain causes a U.S. death every 3.5
Due to the generous contributions over the past seven months, The Foundation is nearing the finish line of the Transitional Care Expansion Campaign.
Some of life’s biggest moments are spent with a nurse. National Nurses Week provides the perfect opportunities to celebrate the nurses who care for us, our friends and our families.
The Centers for Medicare and Medicaid Services (CMS) has announced that Sheridan Memorial Hospital (SMH)
When you think of excellent health care, you think of Sheridan. This not only applies to your Emergency Room visits or the birth of newborns
The Sheridan Memorial Hospital Foundation Staff and Board of Directors are pleased to announce
Upon your initial introduction to Dr. Marty Lucas, you may notice that she carries a unique
When Mary Skretteberg severely broke her ankle in September 2019, the prescription of a prolonged hospital stay felt like insult added to