Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
Health and Wellness

At 91, Charlie Gibson faced some of the toughest challenges of his life all at once. A prostate cancer diagnosis led to the discovery of a malignant kidney, which was promptly removed, leaving him with healing stitches. To make matters worse, Gibson was hit with a severe urinary tract infection that left him bedridden and drained of energy.
But Gibson’s story doesn’t end there — it’s just the beginning of his remarkable recovery at Sheridan Memorial Hospital’s Transitional Care Unit. Gibson affectionately refers to his time in TCU as “the resurrection of Charlie Gibson,” and the team of physical therapists worked with him, pushing him to regain his strength and balance. But, they didn’t just put him through the paces — they made it fun.
Gibson said the highlight of his stay was undoubtedly the decathlon the physical therapists organized for him. Inspired by the Olympic Games that were on TV during his first two weeks at the hospital, Gibson joked that in his next life, he’d come back as a decathlete. The staff took him at his word and set up a series of challenges that included boxing, throwing a javelin (made from a pool noodle), bowling and more. For Gibson, this event wasn’t just a series of exercises; it was a testament to his resilience and spirit.
“I developed the decathlon for Mr. Gibson after being inspired by the fact that even at 91 years old he displayed an unwavering work ethic and determination to overcome any challenge life put in front of him,” said Dawson Eppe, a physical therapy assistant, who worked with Gibson. “I am a firm believer that everyone is an athlete no matter their mobility or age, and the therapy and exercises we choose for treatment should scale with the patient and reflect that.”
The decathlon wasn’t easy. With his recent surgeries and infections, Gibson found the challenges both taxing and exhilarating, but he didn’t back down. With determination and the encouragement of his therapists, Gibson completed every event, even managing to climb the podium at the end. His efforts were rewarded with a gold medal, a symbol of his triumph over adversity.
Throughout his stay, Gibson found the key to recovery was more than just physical therapy. It was about staying positive, listening to happy music, laughing and accepting challenges — even when they seemed insurmountable. These principles guided him throughout his life, from his career with the U.S. Forest Service to his passion for poetry and art in retirement.
Gibson’s story is one of courage, humor and an indomitable spirit. He’s now looking forward to returning home, where he’ll continue his recovery and resume the active life he’s always enjoyed. He knows it will take time to get back into his routine, but he’s ready for the challenge.
For anyone who might find themselves in a similar situation, Charlie has a simple message: “Don’t just lay around. You don’t get well doing that. You need someone to kick you in the butt every day and get you moving.” And if you’re lucky enough to be at Sheridan Memorial Hospital Transitional Care, you’ll have a team of people ready to do just that — with a smile, a laugh, and maybe even a gold medal to reward your efforts.
If you or a loved one have spent three nights in the hospital and still need additional care before returning home, ask your case worker or physician about Transitional Care at Sheridan Memorial Hospital. Our Transitional Care program offers a supportive environment where you can continue your recovery close to home.
Javelin (made from a pool noodle)
Boxing
Bowling
Receiving the Gold

Since the Welch Cancer Center opened its doors in 2013, partnerships within the community and nearby facilities have allowed Sheridan area residents facing a cancer diagnosis to receive excellent patient-centered care close to home. Those same partnerships will now ensure patients in need of radiation treatment will receive the same high level of care while the hospital replaces an essential piece of equipment at the cancer center.
In early September, the Welch Cancer Center will decommission its existing linear accelerator (LINAC), which is used to provide external beam radiation treatment for some cancer patients. In preparation for the project, as the LINAC aged, hospital staff began planning for its replacement, aiming to create the least disruption in care possible and developing a support system for patients who would travel for their radiation treatment.
As patients with new diagnoses are referred to the Welch Cancer Center during this project, they will continue to schedule consultation and follow-up appointments in Sheridan, but will receive the radiation treatment at another facility.
For years, Sheridan Memorial Hospital has had a contract with Billings Clinic for radiation therapy staff including providers, physicists and dosimetrists to provide care in Sheridan. Currently, the team from Billings travels to Sheridan one to two days per week to see patients. This will continue throughout the time the LINAC is being replaced, and patients who travel to Billings for radiation treatment will see the same care team.
“The goal is to create continuity of care by continuing to see patients for consult and follow up in Sheridan,” said Dr. Breanne Terakedis, one of the providers from Billings Clinic who with Dr. John Schallenkamp provides care at Welch Cancer Center. “Patients will continue to see familiar faces in either location in Billings or Sheridan during their treatment schedules.”
During a patient’s initial consultation visit with the Welch Cancer Center, if radiation therapy treatment is needed, the patient will be informed of the LINAC replacement project and options to coordinate care at an outside facility. While many patients opt to receive care in Billings, the Welch Cancer Center team will work with the patient’s facility of choice to coordinate care.
The Sheridan-based care team will coordinate with each patient to determine needs based on the length of treatment required, travel preferences and more. The Sheridan Memorial Hospital Foundation has dedicated resources to assist patients not only with care coordination, but with travel, lodging, meals and other assistance needed or desired. These resources will be offered during the initial consult to patients traveling for radiation treatment, but can be accessed by Welch Cancer Center patients at any time.
“We know any diagnosis can be difficult. Our goal is to support our community members by alleviating financial worries that arise due to travel to receive care,” said Cody Sinclair, chief development officer at Sheridan Memorial Hospital. “Our foundation has resources to ensure treatment and healing can remain the focus for our patients.”
Sinclair, who oversees the foundation, said Comfort Care funds utilized to assist patients during the LINAC project, have existed for several years. For example, in fiscal year 2024, which ended June 30, nearly $10,000 helped provide transportation, mastectomy supplies, wigs and lodging for Welch Cancer Center patients.
“We have an incredibly generous community that has continuously showed a willingness to care for their neighbors, friends and family,” Sinclair said. “The ongoing ability to support individuals fighting cancer is a testament to the longstanding partnerships with neighboring medical teams and our community.”
For additional information about the LINAC replacement project or the Welch Cancer Center, call 307.674.6022 or see https://welchcancercenter.org/.

By Charlotte Walter, PT, DPT, ATC – Physical Therapist at Sheridan Memorial Hospital’s Wyoming Rehab
Improve balance, core, cardio and endurance for the trail
With temperatures in the 100s this week, many locals are looking to the mountains or made plans to head to higher elevations – and therefore cooler temperatures. While some aimed to lounge by favorites like Park Reservoir or other lakes, others took to the trails.
Injuries in the outdoors are common, but there are some basic exercises you can do to help build your bonafides for outdoor recreation. Here are a few tips to reduce injuries, increase strength and feel more confident on the trails.
Improve your balance.
Hiking, even on trails, can sometimes mean crossing a creek on slippery rocks or navigating rocks large and small. In order to build a more stable base on uneven terrain, strengthen your balance. Try standing on a foam pad or uneven ground with your feet closely aligned under you. Lift one foot just off the ground in front of you and move it from side to side, relying on your balance to keep from tipping over. This exercise can help build stability on a single leg. Lunges and single-leg squats are other exercises you can use to build muscle strength and balance.
Build your core.
Conquering a trail often takes a combination of endurance and strength, but core strength is sometimes overlooked when heading outdoors. Having a strong core can provide additional stability as you travel uneven ground. Exercises like side planks, bridges and others can help you feel stronger.
Endurance is key.
While strength in major muscle groups like your legs, core, shoulders and back can increase your ability to climb hills and scramble up boulders, strength isn’t the only factor to consider for outdoor fitness. Ensure your muscles are both strong and have the ability to take you far. You can build endurance by cross training, working in swim or gym workouts alongside your regular trail outings. Staying active in the off-season will help you stay sharp, too.
Do your cardio.
Short bursts of exercise focused on strength may help build the muscles in your legs, but slowly lengthening the time of your cardio exercise helps build your heart and lungs to handle longer outings and require shorter recovery times. When your systems work together in harmony to deliver oxygen to your muscles, your ability to handle those hills on the trail will grow and allow you to go even farther.
If you’re new to the trails or have pain when exercising, contact your healthcare provider to make a plan for physical rehabilitation and a training plan. The views are worth it.
Learn more about Wyoming Rehab services by following the link sheridanhospital.org/medical-services/rehabilitation-services/ Specific exercises and stretches from a qualified professional at Wyoming Rehab will alleviate and can prevent common health problems. Call Wyoming Rehab today to set up a free screening for non-emergent physical impairments or injuries – 307.674.1632.

By Dr. Abigail Turnbough, physician at Sheridan Memorial Hospital’s Rheumatology
How knowing your risks can decrease falls
No one particularly likes to fall down. As children, when we fall, often we shed some tears, seek comfort and return to play. But as we age, a fall can result in significant injury with long-lasting consequences to health and independence.
There are many ways to prevent falls; here are some ideas to consider:
Understand your medical conditions
According to the National Institute on Aging, conditions such as diabetes, heart disease or problems with your thyroid, nerves, feet or blood vessels can impact balance. Worsening eyesight also contributes to falls. Knowing your health history and risk factors can raise your awareness to factors that can impair your balance and strength. If strength and deconditioning is a significant issue, consider asking your doctor about physical therapy. Physical therapists may also be helpful for people with vertigo.
Know your medications
If you take any medications regularly, it’s important to understand the side effects and be prepared for them. Many medications can cause dizziness so preparing yourself with tools to provide stability can reduce the risk of falling. Taking medications, when possible, at times you don’t expect to be active can also help reduce fall risk.
Properly utilize walking aids
If walking, standing or other mobility has become difficult, equipment such as a cane or walker can help you maintain independence. Ensure these aids fit you properly. For example, a cane should be long enough to reach the crease of the wrist when your arm is straight and you are standing. The hand grips on a walker should be at hip height or level with your wrists when your arms are slightly bent, when you have shoes on and are standing. Using a four-wheeled walker may not be best if you have balance issues; instead, I recommend using a two-wheeled walker.
Consider compression, TED stockings
Anti-embolism or compression stockings apply pressure across the leg to promote increased blood flow and therefore decrease risks of dizziness caused by low blood pressure.
Know your limits
If you experience dizziness or weakness, know when to slow down, pause or even stop what you’re doing. Understanding that our bodies change with time can be one of the most useful ways to prevent falls. Know what you are capable of and when to ask for help with riskier activities.
Check your home
Outfitting your home with items like nightlights to improve visibility, wearing eyeglasses if you need them and installing handrails to aid balance can help reduce the risk of falls. Ditching home décor like area rugs, ensuring cords are tucked away and decluttering can also remove tripping hazards.
For adults 65 and older, falls remain the leading cause of injury and injury-related deaths, but taking appropriate precautions and understanding your personal risks can help you lower your chances of falling and extend your ability to live independently.
SHERIDAN – Living in the West, most have become accustomed to the haze that fills the skies in the summer months. Over the last week, though, as people awoke to find ash on vehicles in Sheridan and neighboring communities, the conversations around wildfires and the smoke they produce have generated questions and concerns regarding the health implications.
You may first recognize the smoke in the air using your sense of smell or sight, but a more accurate way to check the air quality in your area is to look it up online. Most of the popular weather apps include an air quality report and websites like fire.airnow.gov allow you to check the air quality and see where the smoke is coming from and how far the smoke plumes stretch.
What you do with this information depends on several factors, including your personal risks and health history.
“While the smoke in the air can be an annoyance for all, those with chronic illnesses, older adults and children are most at risk for serious health concerns due to smoke inhalation,” said Dr. Juli Ackerman, a physician with Sheridan Memorial Hospital’s Internal Medicine Clinic.
Wildfire smoke can exacerbate respiratory conditions such as asthma and chronic obstructive pulmonary disease. Inflammation caused by breathing smoke can also affect individuals with chronic conditions like diabetes, kidney disease or heart disease. Those with underlying or chronic health conditions should visit with their healthcare provider to make a plan for dealing with poor air quality, managing symptoms and ensuring their safety.
“Living in the West where wildfires are fairly common, it’s important to have a plan in place for how you will keep yourself safe from potential impacts of wildfire smoke in our community,” Dr. Ackerman said. “It’s also important to note that even if the smoke seems to clear from the air, symptoms and health concerns arising from that smoke may linger or develop over several days, so it’s important to remain on guard throughout the fire season.”
Young children and older adults are particularly sensitive to smoke in the air. Children’s lungs are still developing, while older adults often have weakened immune systems – leaving both vulnerable to symptoms such as sinus irritation, shortness of breath, wheezing, headaches or coughing.
If air quality is poor, or if you have increased risk, limit your time outside as much as possible. In particular, keep activity levels like outdoor exercise to a minimum. If you do go outside, consider wearing a high-quality mask like an N95; surgical masks and wet bandanas or cloths are not very effective in keeping the smoke particles out of your airway. In addition, change your clothes when you get home to avoid bringing lingering smoke particles into your living space.
In your home, if possible, keep your windows and doors closed. Air purifiers can help filter out some of the particles from wildfire smoke. Air conditioners can also help, but ensure any window units have a tight seal around them, and if you utilize central air, consider switching the system to recirculate mode to avoid pulling in the smoky air from outside.
Contact your healthcare provider if you begin experiencing symptoms such as shortness of breath, trouble breathing or excessive coughing, and as always, call 9-1-1 or go to an emergency department if you are experiencing chest pain or if you think you are having a heart attack or stroke.
Talk to your primary care provider about your healthcare concerns. If you don’t have one, check out Sheridan Memorial Hospital’s Primary Care practice or call or text 307.675.2690.

National recognition cites high-quality care
Sheridan Memorial Hospital recently received recognition for its hospice services, recognizing the program among those across the nation that go above and beyond in providing high-quality care for patients and compassionate caregiver experiences.
HEALTHCAREfirst, a provider of survey programs for home health and hospice agencies, conducts the annual review of hospice programs, acknowledging the highest performing agencies by analyzing the performance on the Hospice Consumer Assessment of Healthcare Providers and Systems survey satisfaction and quality measures.
To be considered for this award, HEALTHCAREfirst considers survey respondent’s willingness to recommend the hospice program alongside 23 additional quality indicator measures. These scores are then compared on a question-by-question basis to a national performance score calculated from all partnering hospice programs contained in HEALTHCAREfirst’s database.
“We began our annual Hospice Honors Award program more than 10 years ago as a way to highlight those agencies that are truly leading the way in providing and demonstrating quality patient care,” said Jeremy Crow, head of RCM and CAHPS Survey, Home Health and Hospice. “We congratulate Sheridan Memorial Hospital on this recognition and are so proud and honored that they have chosen to partner with us in helping drive success for their agency.”
Sheridan Memorial Hospital’s hospice program includes basic medical care with a focus on pain and symptom control; medication, medical supplies and equipment as needed and appropriate; support with psychological, emotional and spiritual end-of-life experiences; respite care for caregivers, family and others; and bereavement support and counseling.
The SMH hospice program includes approximately 15 staff and nearly 40 volunteers.
To learn more about Hospice or becoming a Hospice Volunteer, please click HERE to visit the Sheridan Memorial Hospital Hospice page.

By Alaina Bergstrom, MSN, RN, CCRN-K – Emergency Department and Intensive Care Unit Manager at Sheridan Memorial Hospital
Safety preserves summer fun
Children have left the classroom for the summer. Families are spending more time outside. Implementing some basic summer safety measures will help reduce your risk of spending valuable sunny days in an urgent care, emergency room or doctor’s office.
Protect your skin
Summer means sunshine, but it also means bugs, so there are many ways you can protect your skin this season. Lather on sunscreen with an SPF 30 or higher, and reapply frequently if you plan to spend extended time outside. Unprotected skin can burn quickly, which can cause long-term and immediate damage.
If you’re spending extended time outside, you should also be prepped to protect yourself from bugs. Check yourself for ticks, which can spread Lyme disease, and if you have an allergy to bees or other insects, be sure you have your emergency treatment with you before leaving the house.
Drink plenty of water
There is no one-size-fits-all for daily water intake, as recommended levels typically depend on your activity level, health conditions and other factors. Basic recommendations, though, include drinking water throughout the day, and increasing intake based on how much time you spend in the heat, exercising or sweating. Knowing the signs of dehydration can also help you avoid danger — dry skin, headaches, dizziness, fatigue, muscle cramps and dark urine are among the symptoms. If you’re looking to add a little flavor to your water intake, eat foods that have high water content such as watermelon, cucumbers, celery, tomatoes and many others.
Wear your safety gear
Bicycle rides, rollerblading, boating, swimming and hiking — the recreational opportunities lure individuals and families outdoors all summer long. Safety gear helps avoid tragic incidents. Be sure you and your loved ones wear life vests, helmets, knee and elbow pads, shoes and other appropriate protective gear for each activity. Just as important is ensuring those safety measures fit appropriately. Oversized or improperly worn safety gear can reduce their effectiveness and create additional hazards.
Beat the heat, check the backseat
Whether you’re traveling with children or pets, be sure to check your car’s backseat at each stop. According to the National Weather Service, the temperature in a vehicle can rise 20 degrees in as little as 10 minutes, and 50 degrees in an hour. Each time you make a stop, follow the NWS advice: Beat the heat, check the backseat!
We were excited to have kicked off the Downtown Sheridan Association’s season of Third Thursday events on June 20. Representatives from Sheridan Memorial Hospital were on site, handing out sunscreen and life vests to help keep you and your family safe this summer. Thank you to all who stopped by, said hello, and learned more summer safety tips.

Classes, peer group offer resources for moms
What does labor and delivery look like? What is an epidural? How will I know how to help my baby breastfeed? These are all questions new and expecting moms find themselves wondering. In order to help answer those questions and the many others that arise during and after a pregnancy, Sheridan Memorial Hospital offers childbirth education classes to help expectant parents learn what is ahead of them.
“We want to help parents have the very best start with their baby. Parents may have an idea of what to expect, but attending these classes helps bring their birth plan to life – alleviating fears and misconceptions. The better-prepared parents are for the birth and the more they know what’s ahead of them, the more they will be able to relax and enjoy their new baby,” according to Josie Fagerland, Women’s Health Registered Nurse and Prenatal Class instructor.
Specially trained nurses teach two different classes year-round at no charge. They discuss common fears, concerns, problems and myths surrounding the wonder of childbirth. There is a specific focus on labor, birthing and breastfeeding. Since the classes are held throughout the year, expectant parents can attend a class whenever it is convenient for them. Often, they choose to attend when they are in the second or third trimester of their pregnancy. In addition, Sheridan Memorial Hospital staff have partnered with other community organizations to create a Moms Supporting Moms peer support group.
Prenatal classes
In the Prenatal Class, a nurse talks expectant parents through the stages of labor, vaginal and cesarean delivery as well as how to care for themselves after the baby is born. Some of the topics covered include: changes your body might go through, when to come to the hospital, what to bring, signs of labor, pain management, cervical exams, fetal monitoring and what to expect during labor. The class culminates with a tour of the hospital’s birthing unit, which provides an opportunity to meet the caring, compassionate staff in the Women’s Health Department.
The Prenatal Class is typically held on the first Monday of each month from 5:30-7:30 p.m. in the hospital’s Outpatient Center second floor conference room located at 1333 W. Fifth St.
Breastfeeding and newborn care class
In this two-hour class, a Certified Lactation Counselor (CLC) from the Women’s Health team talks through the basics of breastfeeding and care of the newborn. Though breastfeeding is natural it is not always naturally easy. Latching a baby onto the breast and caring for a newborn is learned and requires an immense amount of support early in the process. The CLC will provide clear and accurate breastfeeding and newborn care information for the “soon-to-be” mother and her support, allowing the baby’s family to feel better prepared and more empowered to care for themselves and their newborn(s). The class covers breastfeeding expectations, strategies for success and how to avoid or navigate complications. Topics include lactation processes, latch and latching techniques, nipple and breast care, breast pumps and pumping, diet considerations, transition of the newborn after delivery, newborn behavior, newborn screenings, elective procedures, diaper care and basic car seat safety.
The Breastfeeding and Newborn Care Class is typically held on the third Monday of each month from 5:30-7:30 p.m. in the hospital’s Outpatient Center second floor conference room located at 1333 W. Fifth St.
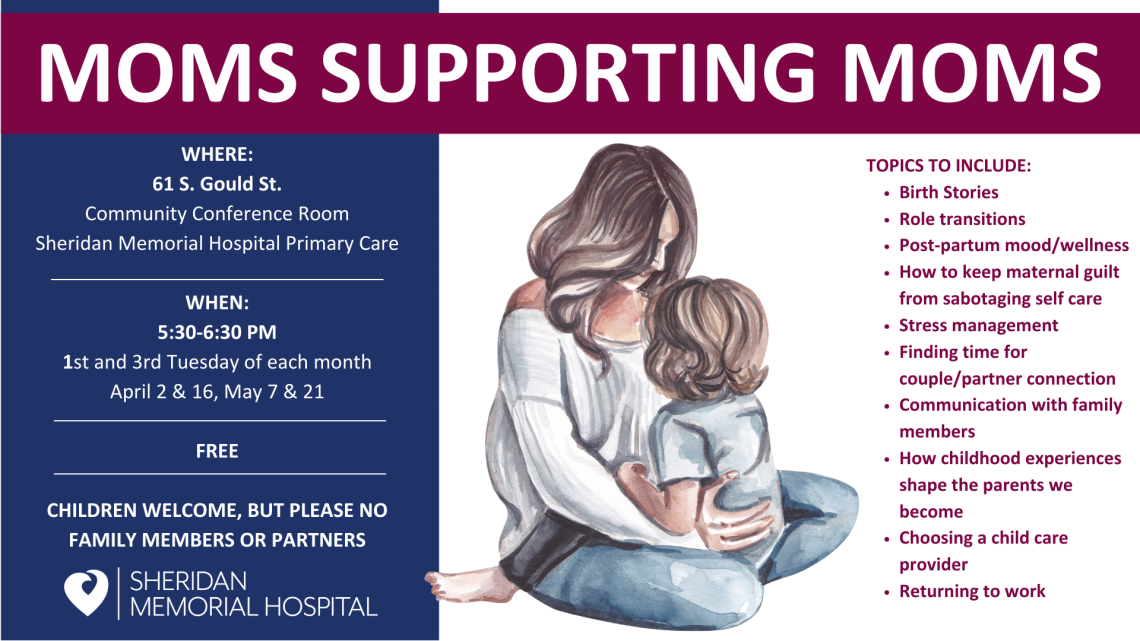
Moms Supporting Moms
Bringing home a new baby often brings joy, and sometimes new parents also experience feelings such as anxiety, sadness and being overwhelmed. These feelings can be isolating and difficult to manage.
In order to support new mothers, Sheridan Memorial Hospital has partnered with other community entities to organize Moms Supporting Moms, a facilitated peer group. Topics discussed include birth stories, role transitions, how to keep maternal guilt from sabotaging self care, stress management, communication with family members, choosing child care providers and returning to work.
Moms Supporting Moms meets the first and third Monday of each month from 5:30-6:30 p.m. at Sheridan Memorial Hospital’s Primary Care community conference room, located at 61 S. Gould St.
How to attend
Pre-registration for the childbirth education classes is required. To sign up online for either class, go to sheridanhospital.org and search for “I’m having a baby.” Once you sign up, an instructor will contact you via email before the class with instructions. Classes are free and recommended for parents expecting their first baby and as a refresher class for those parents expecting again. Both partners are encouraged to attend the classes, which are held in the Hospital’s Outpatient Center second floor conference room at 1333 W. Fifth St.
Learn more about our Women’s Health Department, take a video tour and sign-up for classes HERE, or by visiting https://www.sheridanhospital.org/medical-services/womens-health/im-having-baby/
Listen to what Dr. Emily Denny and Jazz Scott share about services available for new moms, including prenatal and lactation classes in a facilitated peer group.


Listen to what Dr. Emily Denny and Jazz Scott share about services available for new moms, including prenatal and lactation classes in a facilitated peer group.
Learn more about our Women’s Health Department, take a video tour and sign-up for classes HERE, or by visiting https://www.sheridanhospital.org/medical-services/womens-health/im-having-baby/

By Meghan Reinemer, RN – Diabetes Education Coordinator and Susan Kreager, RDN, LD, CDCES – Diabetes Education/Dietician Coordinator at Sheridan Memorial Hospital
Summer is officially here. Let’s check in with ourselves and do a refresh that can benefit all of us, regardless of our health history.
First, how much water are you drinking? How much should you be drinking? There are many factors to take into account: age, gender, activity level and energy expenditure. On average, men should drink 15.5 cups (3.7 liters) and women should drink 11.5 cups (2.7 liters) of water a day. This should increase with warmer temperatures and increased activity. Also, if you are someone who goes up to the mountains in the summer, our bodies lose water faster at higher elevations, so we need to drink more than we would in town.
If you don’t like water, you can always try iced tea, or having fruit infused water for a tasty treat. Drinks like Crystal Light, Mio or even Liquid IV are also options, just keep in mind, these products can have additives like sugar and salt.
Next, let’s talk about sleep. On average, adults need 7-9 hours of sleep each night. It’s not always about how much sleep you’re getting though, so also consider how restful your sleep is.
- Be consistent about when you go to sleep and when you wake up, even on the weekends. (I know! It’s hard.)
- Try and make where you sleep quiet, dark, relaxing and a comfortable temperature.
- Removing electronic devices such as TVs, computers and smartphones from where you sleep boosts sleep hygiene. Try charging your phone on the other side of the room to encourage positive sleep hygiene or putting your TV on sleep mode so it shuts off once you are asleep.
- Avoiding large meals, caffeine and alcohol before bed.
- Get some exercise. Ensuring you are active during the day can help you fall asleep more easily at night. Even if you don’t have an exercise routine, just move your body more than you normally would.
Lastly, let’s talk about fruits and vegetables. Research shows that only one in 10 adults get enough fruits or vegetables daily. What is enough? Five servings of fruit and/or vegetables offer the best amount of fiber and health benefits. Some research suggests dietary fiber can protect against colorectal cancer as well as lower risk of cardiovascular disease. Fruits and vegetables are also excellent sources of antioxidants and phytochemicals, which protect against cancer and support gut health. Produce can be expensive, so try grabbing frozen fruit and make a smoothie. You can throw in some leafy greens and you’ve already have two servings of fruits and vegetables done for the day. Trying to eat more fruits and vegetables can also help us to make other healthy changes in our lives, like starting a garden or going to the farmers markets every week and making friends. Plus, they taste great!
If you are interested in meeting with a dietitian, please call your provider and ask for a referral. A dietitian can help troubleshoot the changes we all face, help with quality of life, and increase longevity. It’s still possible to make changes!

By Erik Smith, MD – physician at Sheridan Memorial Hospital’s Emergency Department
For whatever reason, there has been a surge in patients seeking care for dog and cat bite injuries in the emergency department over recent weeks. Maybe it is the weather. Maybe it is the solar eclipse. Perhaps there is an organized movement to expand the doggie swimming days at Kendrick Park. Regardless, many of these kind creatures are coming after the hands that feed them and inspiring this review of prevention and treatment for animal bites.
Not-so-nice doggie
Domestic animal bites can range from mild to severe, and can even be fatal. Here are a few alarming statistics:
- 5 million dog bites are reported yearly in the U.S. (J Injury Epidemiology)
- 43 U.S. deaths per year are attributed to dog attacks (CDC)
- There are over 17,000 dog bite insurance claims yearly (Insurance Information Institute)
- The average insurance claim for a dog bite is $64,000 (Forbes)
Dogs and cats tend to bite when they feel threatened, however playful bites and herding instincts can also play a role. Dog bites are reported more than cat bites, but cat bites have a much higher rate of infection. The closest body part to the threatened animal will be their target. For adults, arms and legs will most often receive the bite. For children and toddlers, unfortunately, this tends to be the face. Bites to the lower face can result in major soft tissue injury, requiring extensive repair efforts.
Prevention
If you are a pet owner, it is important to control what you are able to before a bite occurs. This includes keeping rabies vaccinations up-to-date, securing fencing and socializing your animals. If you are a parent or grandparent, teach your children to ask for permission when petting animals, avoid animals that are feeding, and to never take toys from them. Do not leave children, especially toddlers, unattended around animals. If chased or bitten by an aggressive dog, yell directly at them and make threatening motions to challenge them to retreat. A short stick or pole can be very effective in preventing a bite by an aggressive dog.
Breaking up dog fights is a very common cause of bites. This often results in multiple bites to several locations. It is difficult to watch fights without intervening, however, keeping hands out of the scrum can help prevent significant injury. A gloved hand or stick could offer valuable protection.
What to do if bitten
If bitten by another individual’s animal, attempt to verify rabies vaccination status. This will be helpful to medical staff in determining risk for the deadly disease. If this is a stray or runaway animal, involve animal control.
If bleeding occurs, hold pressure to the wound. Early rinsing with tap water and gentle soap is a very important step to avoiding infection.
Do I need to go to a clinic or Emergency Department?
Evaluation by medical staff is advised if there is anything beyond minimal penetration of the skin or any concern for rabies exposure.
Treatment typically involves five items:
- Infection prevention. The wound will be cleaned, irrigated and dressed. Antibiotics are often prescribed to prevent bacterial infection.
- Injury repair. The wound will be assessed for depth and severity. Many wounds benefit from some type of closure (surgical tape, sutures, etc). Fractures typically require immobilization. Very deep or complex wounds may require surgery or more aggressive antibiotic treatment.
- Rabies prevention. Rabies is a rare disease that is universally fatal (99%). If there is uncertainty regarding the biting animal’s vaccination status (and certainly if the animal has rabies), a human vaccination series is given. Fortunately, this is very effective at preventing any progression to rabies disease if given early after exposure.
- Tetanus prevention. Any open wound can be a source of Clostridium tetani infection, leading to tetanus disease. Booster shots for tetanus prevention are given every 10 years, however for wounds (such as animal bites), a booster is given if the most recent vaccination period is greater than 5 years.
- Assistance with documenting/reporting. Animal bites often require involvement of outside agencies for which clinical staff can assist. This includes formal documentation of the event and injury, animal control reporting for at-large animals or ongoing safety concerns, workers’ compensation documentation and state rabies testing assistance.
Hopefully the animals you share your house and neighborhood with are loving creatures that would never think of inflicting harm on anything but mice and dog toys. Chances are, however, at some point we all will end up too close to the business end of a scared or aggressive animal.
Learn more about our Emergency Department and services by following the link: https://www.sheridanhospital.org/medical-services/emergency/

By Kelly Lieb, DMSc, PA-C – Director of Patient Experience at Sheridan Memorial Hospital
From a patient’s perception, patient experience is about connection at each interaction and the simplicity and ease of moving through a health care system or encounter.
When you think about your last visit to a hospital or health care facility, what stands out most to you? Do you remember the color of the patient gown? Or whether there were warm blankets and coffee? Do you remember how your care team treated you? Were you treated with courtesy and respect? Or did you feel like just another patient in the provider’s day?
As the patient experience director at Sheridan Memorial Hospital, I often find myself explaning that patient experience isn’t about hospitality – the warm blankets, coffee and treats. So what, as a patient, should you expect from your health care interactions?
Patient experience is about a partnership – one in which both the care team and the patient have responsibilities. The health care team is responsible for the patient’s experience and for every interaction they have during their stay. This entails every employee of a health care system listening to understand and following through on what they said they will do. It’s about welcoming patients into a facility when they may be experiencing fear or uncertainty. It’s about sharing intimate moments of life, death, illness, pain, trauma, cancer diagnoses, surgery, healing, growth and loss. It’s about the simple stuff — the basics — and doing them really well.
From a patient’s perception, patient experience is about connection at each interaction and the simplicity and ease of moving through a health care system or encounter. It’s about understanding a diagnosis, a medication or a care plan. It’s about communication, responsiveness, courtesy, respect and being treated as a unique human. It’s about trust.
Putting the responsibility for a patient’s experience in the hands of the health care system does not excuse patients from their own responsibilities, though. In order to ensure a positive experience, patients must be prepared to share their story completely, accurately and honestly. They must also ask questions of their health care professionals. Respect, too, goes both ways. Patients should expect courtesy and understanding , but that does not give those seeking care the ability to treat their health care team disrespectfully . For the health care partnership to succeed, both sides – patient and care team – must work together honestly, respectfully and transparently.
Patient experience isn’t a new priority in health care, but it is one that has taken on a larger role as consumers have more and more options for their care. When patients have a safe environment and the highest quality competent care, their expectations are met and exceeded. In addition, compassionate healthcare encounters are associated with shorter hospital stays, fewer readmissions, fewer medical errors and malpractice claims, as well as improved provider wellness and decreased burnout.
The Beryl Institute defined patient experience as “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care.” As health care organizations around the country celebrate Patient Experience Week April 29 through May 3, consider your experiences and what stands out most to you.
Click HERE to listen to Kelly Lieb, DMSc, PA-C, and Teara Leibee, BSN, RN, talk about patient experience and patient responsibilities.

Listen to what Kelly Lieb, DMSc, PA-C, Director of Patient Experience, and Teara Leibee, BSN, RN, and Emergency Department/ICU Supervisor, share about themselves, the patient experience, and patient responsibilities.
Click HERE to read Kelly’s article, “What is patient experience?”
By Emily Denney, DO – SMH Primary Care
When I arrived in Sheridan in January 2023, I quickly started seeing patients as a primary care physician. Fairly early on, I had several moms come into the office for evaluation. As I was looking for resources and support for them, I could not find a local group that provided support for postpartum women.
The women I met through my healthcare work were making it through, but wouldn’t it be lovely if there was a support circle of new or not-quite-new moms for them to talk with? The group could give them the opportunity to empathize, share experiences and feel seen. To me, such a group would provide a safety net as women enter or re-enter the world of caring for a new life.
The goal of the group initially centered around post-partum depression, but what I found among new mothers was a wide spectrum of anxiety, depression and overall stress.
Having a baby can be wonderful, but the physical and emotional changes it brings for a new mom, to marriage or partnership, and to other children in the home can be a lot. Then add in all of the other dynamics including financial stress, work stress, etc.
What our community needed was a circle of peers – women who could talk and make friends. In the process of exploring such a group, I was fortunate to find like-minded women in the community. They all agreed we needed such a group and offered to help develop a format and get the program started.
We have had several meetings since starting the new group in November.
We have talked about stress management, boundary setting, sleep and our birth experiences. Going forward, we plan to talk more about self-care, relationships with family and partners and how they change, returning to work, choosing a child care provider and how our own childhoods shape our parenting. We may have some guest lectures as well from community counselors, public health and others. Any and all topics are on the table as we go forward.
The experiences of the moms we have met so far have been wide and varied. There have been wonderful stories, inspirational stories and stories that made me want to cry. Several stories also allowed us to laugh.
What I have learned so far is that women are resilient and amazing, and my hope is that this group can support women to realize that as well. As I have participated in this group, I have reevaluated my own postpartum experiences in a new way, and found gems in the midst.
The free Moms Supporting Moms group will meet Wednesday, March 20, and then each first and third Tuesday of subsequent months at 5:30 p.m. at the Sheridan Memorial Hospital Primary Care community conference room.
Learn more about the hospital’s Moms Supporting Moms group at Moms Supporting Moms – Sheridan Memorial Hospital (sheridanhospital.org).

Each year, Sheridan County welcomes thousands of visitors, from families attending youth sporting events and tourists exploring the Bighorn Mountains to the passersby who spend a night in Sheridan on their way elsewhere. On occasion, those visitors encounter unexpected healthcare needs.
One such traveler, Bill Krieg, was driving home to California with a friend after visiting a ranch outside of Moorcroft. The friend’s wife had passed after a battle with breast cancer and the pair had driven east to the ranch to spread her ashes. Krieg and his friend had intended to make the road trip relatively quickly that October. Following the ceremony, they left Moorcroft and intended to spend the evening in Sheridan before continuing on their way.
“We had stopped for dinner in Sheridan and checked into the hotel about 6:30 p.m.,” Krieg said. “For about a week, I had a weird sensation in my abdomen. Kind of a dull feeling. I thought it was strange but dismissed it. By early evening, I was feeling nauseous and said to my friend that I had a feeling I’d be in the ER before the end of the night.”
Krieg was right. He tried to endure, but by about 12:30 a.m. his friend was taking him to the Emergency Department at Sheridan Memorial Hospital.
Upon arrival at SMH, care teams got to work assessing Krieg’s situation. They performed tests and scans, diagnosing Krieg with acute appendicitis. He would need surgery or face the possibility of his appendix rupturing.
By 6:30 a.m. that morning, Dr. Barry Mangus was in Krieg’s room introducing himself and talking Krieg through the surgery. That afternoon, Mangus performed an appendectomy. The surgery went well, and Krieg was on the mend.
“What stood out to me is that what was conveyed to me happened,” Krieg said of his experience at SMH. “I was not wondering. They didn’t overplay the situation. They were upfront and clear.”
In addition, Krieg said, the nursing care was extremely personable.
“The attention and how I was treated – I cannot commend enough the staff and the physicians who were assigned to me,” he said. “I couldn’t have asked for better care.”
Upon arrival at the hospital, Krieg had told the SMH care team that he was on a road trip, and that he and his friend wanted to get moving again as soon as possible. Dr. Mangus explained the risks, particularly of developing a blood clot due to sitting for extended periods of time post-surgery, but outlined a safe plan that would allow the duo to get back on the road and on their way to California.
By 6 p.m. that evening, about 16 hours after arriving at the SMH Emergency Department, Krieg had been discharged from the hospital and the next morning he continued the drive back to California.
Krieg has worked in the healthcare industry for 40 years, but he noted his experience in Sheridan far exceeded his expectations.
“I have gone through other surgeries elsewhere, and it was far more complex in terms of scheduling and processes,” he said. “The whole experience in Sheridan was extremely personal. You can tell they are all good, caring people who are not just doing their jobs, but being informative and communicative. It was pretty extraordinary.”
While few tourists visiting the Sheridan area expect to utilize the health care services provided by Sheridan Memorial Hospital, Krieg said visitors – and locals – are lucky to have such an exceptional hospital and care teams in the community.
Learn more about the hospital’s Emergency Department and Big Horn Surgical by visiting the respective links.

Meet Dr. Erin Henderson and listen to what she shares about
preventive healthcare and why it is essential to excellent health.
To learn more about Dr. Erin Henderson and Sheridan Memorial Hospital’s Primary Clinic, visit the respective links. To schedule an appointment with a Primary Care provider, call or text 307.675.2690.

By Dr. Allison Dawson, internal medicine physician at Sheridan Memorial Hospital’s Internal Medicine Practice.
If you could provide comfort to your loved ones in a time of pain or sadness, would you? Making decisions about your own health care and medical decisions now, you can prevent your children, spouses or friends from having to make big decisions that cause uncertainty and stress.
Allowing for peace of mind is a gift not given often in life and it is often not thought of by healthy individuals who feel “old age” is still years away. But the gift is one you can give by preventing thoughts such as, “What would they want?” or “We never talked about it.” But at any age of adulthood, you can prepare this gift by simply filling out paperwork and having a few conversations.
Every person has different values and wishes in regards to their medical treatment. No decision is right or wrong, as they are unique to each individual. There are many ways to document your preferences. The documents I believe are the most helpful are a Durable Power of Attorney for Health Care (DPOA-HC), a Living Will and Physician Orders for Life-Sustaining Treatment (POLST).
DPOA-HC
This form allows you to designate who should make medical decisions if you are not able to speak for yourself. This should be a person you are close to, and someone with whom you have discussed your wishes. If you do not designate a specific person, there is a pathway that will be legally followed. In Wyoming this pathway is as follows: a spouse (unless legally separated), an adult child, a parent, a grandparent, an older sibling then an adult grandchild. If this is not a reasonable decision maker pathway for you, a DPOA-HC is an important document.
For example, if your adult daughter is working as a climbing guide on Mt. Everest, she may not be a good option if you require medical decisions to be made in a timely manner. In this scenario, you may wish for your older sister, who happens to be a registered nurse and is knowledgeable about health care and your wishes, to make medical decisions on your behalf if you are unable.
Living will
This is one of the most commonly recognized forms of advanced directives. This is a document detailing specifics regarding medical treatments toward the end of life. One of the most common living wills you may have already heard of is known as “Five Wishes.” This format is written in plain language, and covers your personal, spiritual, medical and legal wishes.
POLST
This is a form that clarifies your wishes in regard to medical treatments, especially life-sustaining treatments, that are honored by health care professionals across settings, whether at home, in a hospital or an assisted living facility. This form includes preferences for attempts at resuscitation, medical interventions, artificial nutrition, medical conditions and patient goals. You may complete a POLST with a health care provider such as a physician, nurse practitioner or physician assistant. It is important to note, though, emergency medical services are legally required to attempt resuscitation unless they have access to your wishes. If it is your wish that EMS not attempt resuscitation, ID bracelets with your wishes can be worn to prevent medical treatment that is not aligned with your values.
While medical care toward the end of life can be stressful, there are things we can do now to make that process less painful for all involved.
I encourage you all to speak with your primary care provider about these documents and discuss them based on your individual health care needs.
Dr. Allison Dawson is a physician with the Internal Medicine team at Sheridan Memorial Hospital. She is trained in palliative care and hospice medicine. If you would like to make an appointment with Dr. Allison Dawson, call or text 307.675.2650.
While commercials often highlight allergy season by depicting an array of green grasses, flowers and pollen floating through the air, the timing of allergy season depends heavily on an individual’s specific sensitivity and can take place throughout the year.
For Sheridan resident, teacher and photographer Tim Doolin, allergy season centers primarily around the fall archery elk season.
“Starting in my mid-30s, I began to develop quite a number of seasonal allergies,” Doolin said. “As time elapsed, those allergies began to disrupt my way of life, causing me to wake up at all hours of the night, with my nose just streaming.”
Doolin said he realized his respiratory health was being affected by the allergies and decided to seek treatment.
He began his initial appointments in Billings, as he was unaware Sheridan Memorial Hospital offered allergy testing and treatments. Dr. Cheryl Varner’s team at SMH’s Ear, Nose and Throat Clinic administered the treatments regularly to allow Doolin to stay closer to home for his care. Eventually, Doolin opted to switch, putting the direction of his allergy treatments under Varner’s team at SMH.
“The relationship that I had developed with the office, Dr. Varner, and all of the nurses in Dr. Varner’s office was something that I didn’t want to disrupt or change,” Doolin said, adding that with the help of the SMH Ear, Nose and Throat Clinic, he petitioned Blue Cross Blue Shield to cover additional allergy testing. “I had that testing done recently with Dr. Varner‘s office and was quite impressed with how thorough and comprehensive the testing was. The tests done here at Sheridan Memorial Hospital were far more thorough and extensive than those I received initially through my treatment in Billings.”
“I have high hopes that this continued treatment with a more comprehensive and refined approach to the serums I will be receiving will actually improve my allergy response even more than the benefits I have already experienced,” Doolin added.
According to SMH’s Ear, Nose and Throat Clinic, an allergy is a condition in which the immune system reacts to something eaten or in the environment that doesn’t affect most other people. People often think of allergy symptoms as sneezing, runny nose, nasal stuffiness and itchy, watery eyes.
However, allergies can also cause symptoms such as postnasal drip, head congestion, frequent “colds,” recurring ear infections, hearing loss, dizziness, chronic cough and asthma. Even stomach and intestinal problems, skin rashes, chronic headaches and fatigue can be symptoms of an allergy.
Various treatments exist for those suffering from an allergy or multiple allergies. Avoiding the allergen is often a first step when possible, followed at times by medications and immunotherapy. Sheridan Memorial Hospital’s Ear, Nose and Throat Clinic works with each individual patient to develop an allergy testing and treatment plan.
Doolin said the staff at Sheridan Memorial Hospital treats patients with care and like an extended family.
“Every week throughout the year, there are quite a number of us who receive this allergy shot therapy, and without fail, the conversations revolve around grandchildren, children, holiday and summer plans, and life in general,” Doolin said. “It really is like a small knit little family and the community is quite positive and something I appreciate.”
To schedule an appointment with the Ear, Nose and Throat Clinic at Sheridan Memorial Hospital call 307.675.4646 or to learn more see sheridanhospital.org/medical-services/clinics/ear-nose-throat.
By Dr. Erin Henderson, internal medicine physician at Sheridan Memorial Hospital’s Primary Care Clinic
When is the last time you went to your doctor or primary care provider? Were you sick? Chances are you were seeking treatment for some sort of illness or injury, as data shows that less than 6 percent of Americans receive the recommended preventative services.
What are those preventative services?
There are a wide range of services you should check in with your health care provider about each year. These can include physician counseling on concerns like weight management, alcohol and tobacco use, blood pressure and cholesterol or screenings like mammograms, colonoscopies, pap smears, prostate screenings and immunizations.
Even if you’ve had a clean bill of health for years, it pays off to check in with your physician each year as it allows you to track your health over time.
Yearly visits mean you and your doctor can easily see changes in your health. Maybe your blood pressure is significantly higher one year. Or, perhaps you’ve lost a lot of weight without dieting. These can be signs of serious health issues. By conducting your annual wellness visit, your doctor can catch problems in their early stages, which is when they are usually easiest to treat.
Checking in with your provider once a year also allows you to share important health information. Whether this includes updates to any medications or supplements you’re taking or changes in your family medical history, all of the information can come in handy down the road for your health care team.
For example, if you only see your primary care provider when you’re sick, they have only seen you when your body needs treatment. It’s harder for physicians to treat illnesses if they only know your system when it’s under stress, ill, in pain, etc.
Seeing your physician regularly also allows you to build a relationship with the provider. This can help establish trust over years of care.
Most health insurance plans are required by federal law to cover a set of preventative services — like shots and screening tests — at no cost to you. While you should always check with your insurance company ahead of time, it’s likely your annual wellness visit and preventative screenings would be covered by your insurance plan.
As the new year begins, consider scheduling a wellness visit with your primary care provider. It never hurts to start the new year with a fresh conversation about your health!
To make an appointment with Dr. Henderson, call 307.675.2690. To learn more about the Hospital’s Primary Care team: https://www.sheridanhospital.org/medical-services/clinics/primary-care/.

Listen as Dr. Joshua Scott Highlights SMH’s 100th Robotic Surgery Milestone.
To learn more about Dr. Joshua Scott, the hospital’s Big Horn Surgical practice, and the Robotic-Assisted Surgery Program at Sheridan Memorial Hospital, visit the respective link or visit SheridanRoboticSurgery.com and Robotic-Assisted Surgery FAQs.