Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
Health and Wellness

By Dr. Christopher M. Prior, DO, FAAFP – Physician at Sheridan Memorial Hospital’s Internal Medicine Practice
June is Men’s Health Month, and according to studies, 60% of men don’t consult their physician regularly and 33% are less likely to visit the doctor than women. But one area of men’s health is seeing a surge in activity.
Use of testosterone hormone as well as natural testosterone level boosting supplements has skyrocketed in recent years with people looking for treatment of fatigue, poor cognition, difficulty losing weight or gaining too much weight, and erectile dysfunction. The most common cause of low testosterone is age related low testosterone. Most adult males lose 1-2% testosterone annually after their mid-thirties. Chronic diseases such as obesity, sleep apnea, drug and alcohol abuse, hemochromatosis (harmful levels of iron in the body), as well as exposure to radiation or chemotherapeutics are potential causes of low testosterone. Rarely do genetic disorders lead to hypogonadism (a failure of the gonads, or testes, in men).
Treating potential causes of hypogonadism before starting testosterone supplementation would be the most common recommendation. Many people, however, seek over the counter supplements first. Unfortunately, some over the counter supplements can worsen symptoms or have adverse side effects. For example, there has been an increased number of young men in their 20’s and 30’s diagnosed with secondary hypogonadism caused by taking testosterone boosting supplements or illegally using testosterone hormone. Inappropriate use of testosterone can worsen sleep apnea, cause polycythemia (increases red blood cell count), elevate prostate specific antigen, increase cholesterol, as well as increase risk for stroke and heart attack.
Many urban areas have seen an increased number of low testosterone retail clinics. Most of these are cash only, with no insurance coverage for medications, lab tests or the prescription supplementation frequently recommended. Expensive blood work, estrogen blocking medications, pituitary stimulating hormones as well as testosterone supplementation can be cost prohibitive for most. While some users claim to feel better, think better, sleep better, and lose weight, there is very little evidence to support these claims.
Recently, the two largest medical organizations in the United States, the American Academy of Family Physicians and American College of Physicians agreed that the only clear reason to treat low testosterone is erectile dysfunction. While testosterone has been used to help bone density, cognition, anemia, overall well-being, and infertility—there are no articles suggesting benefits in these areas with testosterone supplementation.
Routine screening of testosterone levels is not recommended for asymptomatic males. When a patient has symptoms that may be related to hypogonadism they may be screened for low testosterone in addition to the previously listed chronic causes of hypogonadism. If testosterone levels come back low, testosterone replacement therapy can be initiated, with appropriate monitoring regularly with blood tests and clinical symptoms. This is generally a mutually agreed upon decision by the patient and provider after a review of risks and benefits.
Talk to your primary care provider about your healthcare concerns. If you don’t have one, check out Sheridan Memorial Hospital’s Internal Medicine practice or call: 307.675.2650
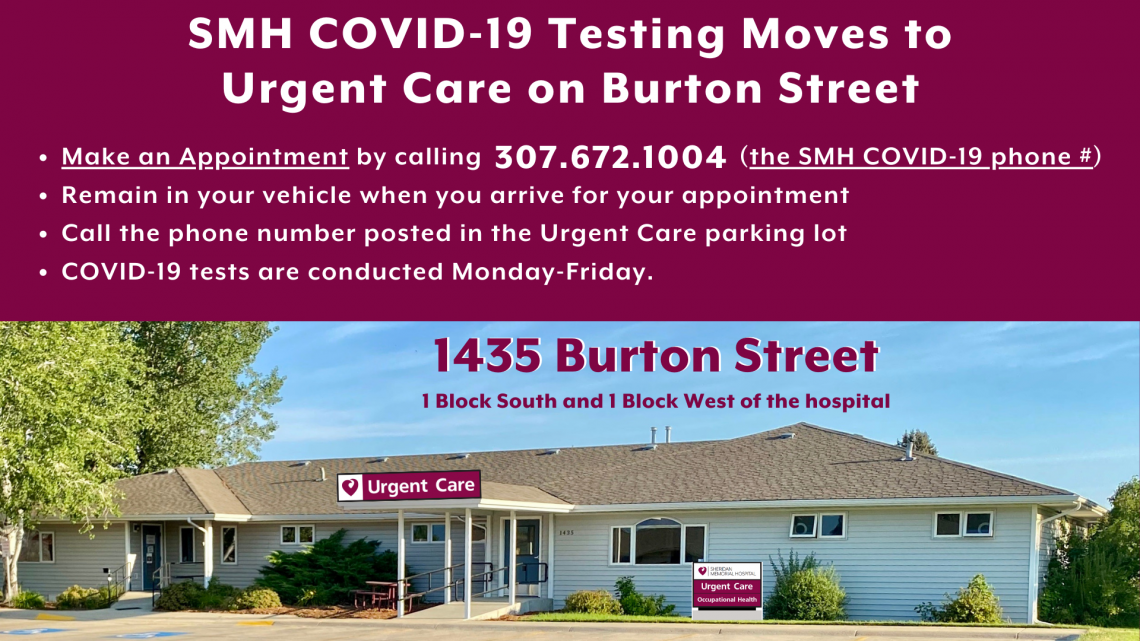
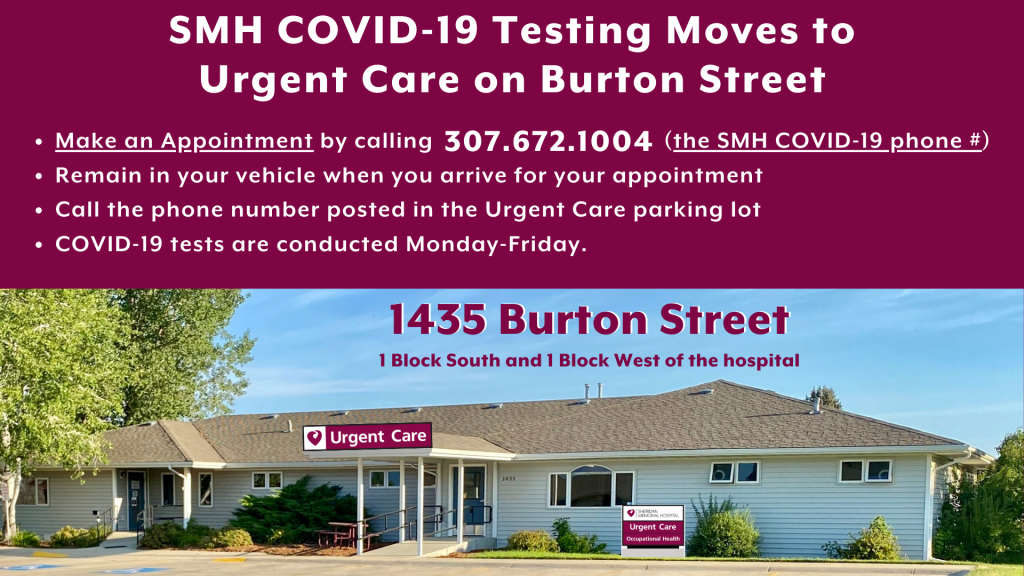
Sheridan Memorial Hospital’s Covid-19 testing is now being done at the hospital’s Urgent Care – located at 1435 Burton Street – one block south and one block west of the hospital – follow signage to Urgent Care.
Persons wishing to be tested for Covid-19 do need an appointment and should still call the hospital’s Covid-19 phone number: 307-672-1004. When a staff member calls them back to schedule their appointment, they will help the caller select the most appropriate test for their needs.
When people arrive for their appointment, they should remain in their vehicle and call to let the staff know they are there. The notification phone number is posted in the Urgent Care parking lot. Covid-19 tests are conducted Monday-Friday.
More information about Covid-19 can be found at https://www.sheridanhospital.org/community/coronavirus/
Dr. Jason Ackerman has been practicing medicine in Sheridan for the past 8 years and has been a mainstay in the Sheridan Memorial Hospital Internal Medicine Clinic. He is excited about opening an Addiction Medicine Clinic here in Sheridan. We sat down with him recently to get his thoughts on this new adventure in his career, why he is taking this leap into addiction medicine and what it means for the Sheridan community.
Q: Dr. Ackerman, tell us why you felt it was important to get this certification and open this clinic in Sheridan.
A: I started treating opiate addiction while I was in residency and continued that when we moved to Sheridan after residency. It was initially a very small part of my practice, but it began to grow more rapidly the last few years. I came to realize how underserved and undertreated patients with addiction are in our community. When I had a chance to get boarded in Addiction Medicine it seemed like a good opportunity to broaden my knowledge base and start helping more patients with a variety of addiction problems.
While it’s been needed in Sheridan and our surrounding communities for a while, it’s also been one of the most rewarding aspects of my practice. Not only is it a chance to improve patients’ health, in many cases it is truly giving people a second chance at life. I have had homeless patients find housing and start working. I have had patients go back and get college degrees and others start new careers. Parents who have lost their children due to addiction have been able to get their kids back home. They see successes that they never thought were possible and it’s amazing to be a part of that.
Q: What does it mean to see a doctor/physician who specializes in addiction? Aren’t most internists focused on physical health?
A: That certainly is our primary training and focus. But internal medicine spans a broad range of specialties. One of the great things about practicing here is that we can find our niche and develop skills in our area of interest. There is a big component of mental health in addiction, but as research progresses in the field we are learning more and more that this is a true disease process and not simply a series of bad choices. The good news is that means there are medications and therapies that we can use to help people recover and succeed.
Q: Is this a pain management clinic? What services are offered through the new clinic?
A: This is not a pain management clinic, although we have certainly helped people taper off of pain medications. Our focus is treating the disease of addiction, whether it is opioid pain medications, heroin, alcohol, stimulants, gambling – it really runs the gamut of substances and behavioral addiction.
Q: Can you talk about medication assisted therapy and what exactly is suboxone?
A: Just as some people are able to treat their diabetes with diet and exercise while others need insulin and other medications, there are a number of ways to approach the disease of addiction. Some people do well with counseling or groups like Alcoholics Anonymous. But when we start looking at the process of disease, there are some medications that can significantly improve people’s chances of recovery. Medication assisted therapy is using evidence-based, targeted medications to help people achieve that recovery. Suboxone is probably one of the best known and most effective medications. The primary component of it is buprenorphine, which is a partial opioid agonist. That’s essentially a fancy way of saying a medication that hits all the same receptors as opiates like pain medications or heroin, but turns on those receptors just enough that people do not have cravings or withdrawal symptoms. That allows people to not only remain clean and sober, but also increases their ability to incorporate all the important tools from other aspects of treatment – groups, counselors, etc. – and substantially increases the chances of long term sobriety.
Q: Are there specific areas of addiction on which you concentrate?
A: Not really. Part of that is that addiction is a broad field that seems to be evolving fairly rapidly at this point. The other part is that addictions don’t always come packaged quite as neatly as we used to think. Many people are able to get off of pain pills, only to develop an alcohol problem or a meth problem. There seems to be a genetic component and it can definitely run in families. Some people just seem to be wired to have problems and addictive tendencies with whatever substance crosses their path. I will say treating opiate addiction is very satisfying. We all see the headlines about skyrocketing fatalities from opiate overdoses. In clinic we see patients that have been using for years and cannot function without massive, potentially lethal doses of opioids in their system. They are literally a bad night or a tainted batch of pills away from dying. But when we can find the right doses and combinations of medications they are able to get clean relatively quickly. The patients frequently tell us that they feel “normal” for the first time in years.
Q: Do prospective patients need a referral to this new clinic? How does the process work?
A: We are always happy to take referrals, but you certainly don’t need one to get an appointment. People can just call us at 307.675.2674.
Q: If I have concerns about a family member or friend who may be addicted, how can I best help them?
A: That’s an incredibly difficult position to be in. Ultimately, patients with addiction need to be ready to get better. Sometimes that readiness comes with the urging of friends and family, sometimes it happens spontaneously, and sometimes a person has to hit bottom before they see that change needs to happen. I think being supportive and encouraging them to get help is really important. And if they’re just not ready at this moment, don’t give up – they will need your support when they are.
Q: Tell us a little about the partnership with Northern Wyoming Mental Health (NWMH).
A: A few years ago we realized how much better our treatment for opiate addiction would be if we teamed up. At the time I was treating opiate addiction with suboxone, but had no real links with counselors. Meanwhile they were treating a number of patients with opiate addictions but nobody to prescribe suboxone or other medications. Since then the partnership has really expanded and blossomed and covers all aspects of addiction. We have been fortunate enough to secure grant funding that can help some patients with the cost of medications and visits. We are able to have an amazing peer specialist (an addiction counselor who has recovered from addiction partially with the help of our program) and a wonderful case manager in our clinic on our main addiction treatment days. The partnership also opens up all the resources of NWMH to patients going through our program, including various group therapies, relapse prevention groups, individual counselors, and vocational rehab. I think a lot of our success stems from being able to align ourselves with their team.
Dr. Ackerman and the team at the SMH Addiction Medicine and Recovery Clinic are ready to serve the Sheridan community. If you have questions or need to schedule an appointment, please call 307.675.2674. For additional information please click here.

By Lynn Grady, RN, BSN – Sheridan Memorial Hospital Emergency Department and Intensive Care Unit Manager who also heads up the hospital’s Stroke Program
Every 40 seconds in the United States, someone experiences a stroke. Stroke is a debilitating and deadly injury to the brain that causes a death every 3.5 minutes in this country. Often the death follows a lengthy illness that limits a person’s participation in the daily activities of life.
Fortunately, there are several things you can do to minimize the risk factors of experiencing a stroke. Managing health conditions such as atrial fibrillation, high blood pressure, high cholesterol, diabetes, and eliminating lifestyle risk factors such as smoking can significantly decrease your risk of experiencing a stroke. Other lifestyle changes one can make to decrease the risk of stroke include maintaining a healthy weight by eating a healthy diet and engaging in regular exercise regimens, minimizing alcohol consumption, reducing personal stress levels, and maintaining regular appointments with one’s healthcare provider. Despite the best efforts of the healthcare industry in providing education and resources, stroke remains the 5th leading cause of death in the US since 2015.
If you do experience signs and symptoms of a stroke, such as sudden numbness in the face, arm, or leg, especially on one side of the body, or sudden confusion, difficulty speaking, or loss of coordination, call 911 immediately or immediately get to the Emergency Department. If someone you know is experiencing these symptoms, a quick and easy way to determine if this person may be experiencing a stroke is the F.A.S.T. mnemonic.
F – Face: Ask the person to smile. Does one side of the face droop?
A – Arms: Ask the person to raise both arms. Does one arm drift downward?
S – Speech: Ask the person to repeat a simple phrase. Is the speech slurred or strange?
T – Time: If you see any of these signs, call 911 right away.
As a stroke can happen in several different areas of the brain, a patient may experience varying degrees of speech and motor symptoms. This is why it is important to immediately seek medical attention if you are experiencing even one of the symptoms above. Acting F.A.S.T is key to minimizing long-term effects that may be experienced due to a stroke. A quick diagnosis is critical to ensure that a patient receives the treatment and medication they need in order to regain as much function as possible.
At Sheridan Memorial Hospital, we are able to offer our community rapid brain imaging and access to a neurologist by using our Tele-Stroke services provided through Wyoming Medical Center. This provides our staff and patients direct access to stroke experts and optimal treatment options that would otherwise not be available in a community in the size of Sheridan. One of the potential treatment options is a medication called TPA, a powerful anticoagulant (blood thinner) that can be used to help dissolve the clot that is causing the stroke. We are able to provide this particular treatment in Sheridan so that our patients can stay home in their community alongside their families while receiving care. TPA, however, must be administered within 4 hours of the initial onset of symptoms — another reason why time is of the essence if you think you may be experiencing a stroke.
After the initial treatment of the stroke, our patients can then go on to receive physical and occupational therapy services offered by Sheridan Memorial Hospital’s Wyoming Rehab to ensure that they can regain as much strength and function as possible prior to being discharged. If TPA is not an option for the particular type of stroke a patient is experiencing, a treatment plan can be quickly determined between our physicians at Sheridan Memorial Hospital and the neurologists through Wyoming Medical Center.
If you have any questions regarding your potential stroke risk factors, you are highly encouraged to schedule an appointment with your primary care provider to address these concerns. If you don’t have one, check out Sheridan Memorial Hospital’s Internal Medicine practice or call: 307.675.2650

Sheridan Memorial Hospital Foundation is working to connect the community with the Transitional Care expansion project. This expansion ensures our family, friends, and neighbors have a comfortable, private environment to heal and regain their strength and confidence to return home safely following a serious illness, injury, or surgery. The message has connected with so many people who understand the importance of having this care close to home.
The $8 million dollar project got a kick start toward the end of 2021 with a $2.1 million dollar grant from the State Loan and Investment Board (SLIB) to complete demolition and infrastructure work. Since then, The Foundation has steadily worked on raising the $4.4 million dollars that will allow Sheridan Memorial Hospital to start the final phase of construction to repurpose the 2nd and 3rd floors of the hospital for the 20 private Transitional Care rooms.
Due to the generous contributions over the past seven months, The Foundation is nearing the finish line of the campaign. A matching challenge in March was exceeded and The Foundation board stepped in to ensure that every gift received was matched. This opportunity helped The Foundation raise nearly $700k in March.
To date, gifts and pledges from our community of over $3.8 million dollars have been made to the Transitional Care expansion. This means the goal of raising the $4.4 million dollars by June 30, 2021, is within reach. Approximately one year from now, Sheridan will have a new Transitional Care Unit.
Foundation Board President and Campaign Co-Chair Richard Garber expressed his gratitude to our community and welcomed everyone to come see the vision for Transitional Care saying, “We appreciate the generous response from our community. Sheridan is a place where people take care of each other and share in a vision to ensure our community is a great place to live well into the future. This project will do just that and encourage everyone to come see the original 1954 hospital space that will soon be transformed for Transitional Care.”
To get the most up to date Foundation information and get involved in the Transitional Care Expansion Project, visit sheridanhospital.org/foundation.

Some of life’s biggest moments are spent with a nurse. National Nurses Week provides the perfect opportunities to celebrate the nurses who care for us, our friends and our families. They have an important job to do, and we are grateful to them for being there for us. We put out a call to our community to share with us how an SMH nurse or nurses have been there for them. Now we share their words with you and the nurses with gratitude. Do you have a great nurse story to tell? Click HERE to tell us about it and recognize the nurse who made a difference in your life.

The Centers for Medicare and Medicaid Services (CMS) has announced that Sheridan Memorial Hospital (SMH) has earned an Overall 5-Star rating. This comes only two years after SMH garnered overall 4-Star status and places SMH as one of only two 5-star hospitals in Wyoming.
“Attaining 5-Star status puts us in the top 13.56 percent of hospitals nationwide and shows the efforts we are putting into improving our processes are working,” said Barb Hespen, Chief Nursing Officer. “It really is a testament to the hard work and dedication put in by our physicians and staff every day.”
Since the start of the star rating system in 2015, CMS collects and compiles data from hospitals and uses that information to assign ratings from 1-5 stars. Much of the data comes from surveys of actual patients assessing their specific experience. CMS uses the rating system to measure multiple facets of over 4,000 hospitals across the country to drive systematic improvements in care and safety for patients. The specific performance indicators in the CMS Star Rating system include measurements related to five areas: Mortality, Safety of Care, Re-Admission Rate, Patient Experience and Timely and Effective Care. The ratings are published on the CMS Care Compare website.
Hespen added that improvement in readmission rates and patient length of stay was a major factor in earning a 5-Star rating.
“Our number of 30-day readmissions continued to be lower than the national average; in addition to the low number of excess days patients spent in acute care,” Hespen said.
In a memo to SMH physicians and staff members, CEO Mike McCafferty stated, “Thank you all for your commitment to our mission and your dedication to strive for perfection in all that we do. The road to excellence is a journey that requires all of our team members to embrace our principles and standards of behavior to deliver the best possible experience and value to our patients. Let’s continue to support one another to sustain this level of excellence for years to come.”
When you think of excellent health care, you think of Sheridan. This not only applies to your Emergency Room visits or the birth of newborns but when you need additional time to recover from your injury or illness. That is Transitional Care.
Many think of the Transitional Care Unit (TCU) for rehab following a total knee or hip replacement. These patients make up only 5% of whom we treat in the TCU. In actuality, 95% of our TCU patients need our services after an unexpected hospitalization due to severe injury, illness, or urgent medical conditions like those listed below.
- Respiratory illness – pneumonia, COPD, influenza, COVID-19
- Cardiac conditions – congestive heart failure, post bypass surgery
- Urinary tract infections
- Multiple falls at home caused by an underlying medical condition
- Diabetes
- Complex wound care management
- Fractures – especially hip and leg
- General decline and weakness complicated by one or multiple medical conditions
- Long-term IV antibiotics due to complex infections
If you and your doctor plan for you to go home but your recovery is slower or more extensive than expected, you may require short-term rehab to ensure the best possible outcome. A transitional care stay is tailored to your needs based on the extent of your injuries or medical condition, your overall health, and your ability to live safely upon discharge. On average, the length of stay is 14 – 18 days, but patient needs vary from as little as a week to others requiring a few months.
Think about how hard it is to go on vacation and get back into a routine. When the body is fighting any of the above medical issues, patients are surprised at how rapidly their physical abilities deteriorate. Being ill or injured and out of your routine can cause you to lose the ability to perform daily tasks, stay mobile, and provide the level of self-care necessary to return home safely. Transitional Care helps patients relearn functions like how to properly reach into a closet and dress after their injury, ensure optimal breathing after a bout with pneumonia and being bedridden for a week, or navigate rugs and other trip hazards at home with their new walker.
Most don’t plan on needing an additional rehab stay, but we are here to get you back to your house and your life when the unexpected happens, and you need it most.
To learn more about Transitional Care talk to your provider or Click Here (https://www.sheridanhospital.org/medical-services/transitional-care/) today.

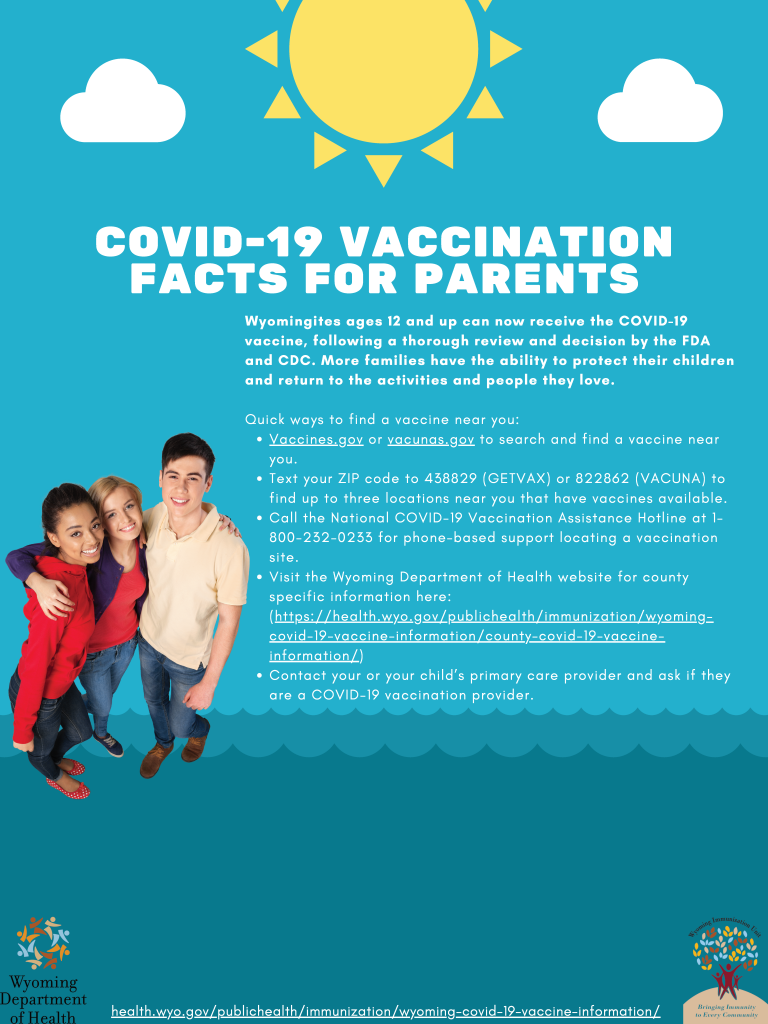
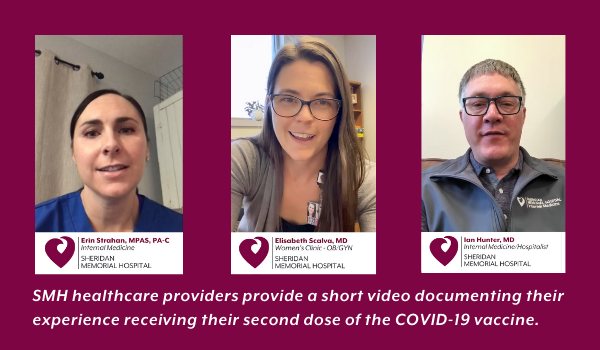
With the COVID-19 vaccines becoming more and more available to everyone, we asked some of our health care providers why they got the vaccine and what their thoughts are for our community.
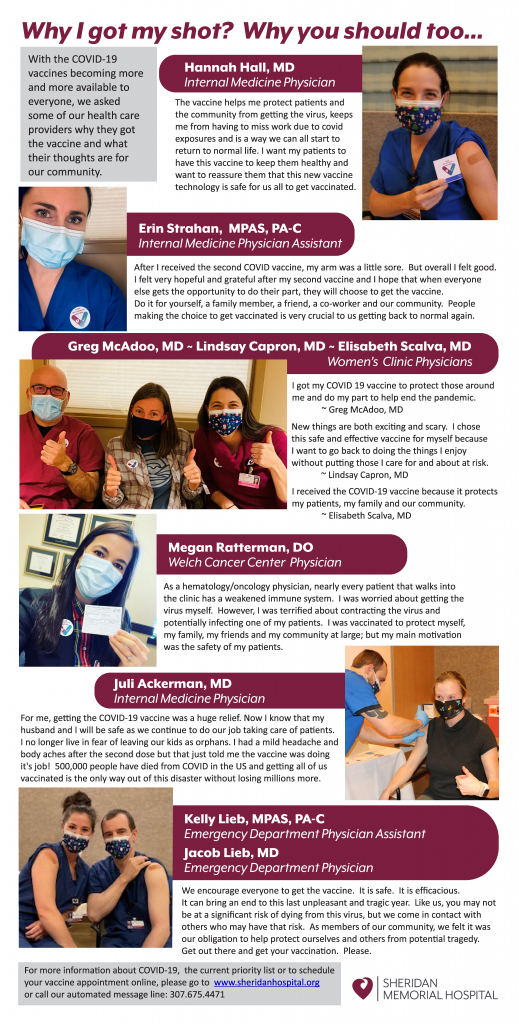
For more information about COVID-19, the current priority list or to schedule your vaccine appointment online, please go to sheridanhospital.org or call our automated message line: 307.675.4471.

It may not be the most glamorous subject, but talking about colorectal cancer saves lives. Among cancer affecting both men and women, colorectal cancer is the second leading cause of cancer-related death in the United States. Unlike many cancers, we have effective tools to help decrease the development of colorectal cancer and identify its presence at an earlier stage.
The risk of colorectal cancer increases with age, with more than 90% of the cases we see being diagnosed in people age 50 or older. There are many factors that are associated with an increased risk of colorectal cancer. Some of these risk factors are related to lifestyle choices and are therefore modifiable. Maintaining a healthy weight, being physically active, not smoking or chewing tobacco, avoiding heavy alcohol intake, and eating a balanced diet that limits intake of red or processed meat can all help decrease your risk of colorectal cancer.
Some risk factors cannot be changed. For one, colorectal cancer is more common as we age. It is also more common in people with a personal history of a certain type of colon polyp, called adenomatous, or a previous colon cancer. Being diagnosed with an inflammatory bowel disease, particularly ulcerative colitis, increases your risk. Most colorectal cancers are diagnosed in people who do not have a family history of colon cancer, but nearly 1 in 3 people who are diagnosed with colon cancer do have a family history of the disease. Only about 5% of cases of colorectal cancer are related to an inherited predisposition, but the rate of colorectal cancer is much higher in these individuals than in the general population, and it tends to develop at an earlier age. Two of the more common genetic predispositions are familial adenomatous polyposis (FAP) and hereditary non-polyposis colorectal cancer (Lynch syndrome). Although we don’t understand why, African Americans have the highest colorectal cancer incidence and mortality rates of all ethnic groups in the US.
Colorectal cancer may cause symptoms as it grows. These symptoms include seeing blood in or on your stool, unintentional weight loss, a change in bowel habits and weakness or fatigue caused by a low blood count.
Screening is the practice of looking for cancer or pre-cancer in individuals without symptoms. Screening is incredibly effective when it comes to colorectal cancer because, from the time the first abnormal cells start to develop, it takes on average 10-15 years for those cells to become a colorectal cancer. Screening is one of our most effective tools for preventing colorectal cancer because it allows us to find and remove precancerous polyps and identify people who would benefit from more frequent screening. Screening can also identify small cancers that aren’t yet big enough to produce symptoms.
There are several screening tools for colorectal cancer, including tests done on your stool, radiographic studies and colonoscopy. The stool studies either look for evidence of trace blood that isn’t enough to be seen by the naked eye or look for altered DNA that can be associated with abnormal cells in the colon. Stool studies that look for blood need to be repeated every year if negative. A negative stool DNA test needs to be repeated every three years. A CT or virtual colonoscopy is a radiographic study that involves cleaning out the colon at home and then coming into the hospital for a CT scan. If any abnormalities are seen, the study needs to be followed up with a colonoscopy at a later date. If the study is negative, it should be repeated every five years. Stool studies and virtual colonoscopy are only appropriate for patients with an average risk of colorectal cancer. A colonoscopy is a procedure that is done using a small fiber-optic tube and air to examine the lining of the colon after a prep has been completed the day before. Colonoscopy allows for the identification of polyps and removal, or biopsy if too large, at the same time as the procedure. Depending on the findings during the procedure and individual risk factors, colonoscopy may be repeated every year for high-risk individuals to a more typical range of 3-5 or 8-10 years.
Talking to your doctor about your risk factors can help identify the most effective and appropriate screening test for you. In general, screening is recommended between the ages of 50 and 75, though there are reasons to start earlier or stop later for some people. It is estimated that only about two-thirds of adults in the US are up to date with their colorectal cancer screening. Every year, about 140,000 people in the US will be diagnosed with colorectal cancer, and 50,000 people will die from it. Our best tool to decrease both of these numbers is screening. Talk to your doctor today.
Talk to your primary care provider about your risk factors. If you don’t have one, check out Sheridan Memorial Hospital’s Internal Medicine practice or call: 307.675.2650
By David Nickerson, MD – Medical Director of Sheridan Memorial Hospital’s Urgent Care
Navigating the healthcare system can be difficult. Even in a small town like Sheridan, there are multiple options for care and it may not always be clear where to start. Sheridan Memorial Hospital offers three different points of access for general medical care.
Internal Medicine
The Internal Medicine Clinic is located in the Outpatient Center at 1333 W. 5th Street and is the best location for treatment of chronic medical problems, such as high blood pressure or cholesterol, and diabetes. There is also a focus on health maintenance and prevention. The Internal Medicine Clinic uses the team model, meaning that you will have a primary doctor or advanced practice clinician but can also see one of the colleagues with whom they work closely if they are not available. In addition, patients can also be referred on to the appropriate specialist, if needed.
For the safety of patients and staff, patients with symptoms that could represent COVID-19 (Fever, chills, body aches, cough, runny nose, sore throat, vomiting, diarrhea, headache, or changes in the sense of smell or taste) are currently being referred to the Urgent Care or Emergency Department.
To make an appointment at the Internal Medicine Clinic, patients may call 307.675.2650.
Urgent Care
Sheridan Memorial Hospital’s Urgent Care recently moved to 1435 Burton Street, the former location of Bighorn Mountain Medicine. It is the ideal location for immediate treatment of new medical problems, such as colds, flu, ear/nose/throat issues, musculoskeletal injuries, skin issues, urinary problems, stomach issues, and headache. It is also the best place to be seen for non-life threatening COVID-19 concerns.
Laboratory and x-ray equipment are onsite and common prescription medications can be dispensed during your visit through local pharmacies. Finally, if you have a medical problem and are unsure where you should be seen, the Urgent Care is an excellent starting place and can refer you to a specialist or transfer you to the Emergency Department.
No appointment is necessary at the Urgent Care and you may walk in or visit www.SheridanUrgentCare.com to save your spot. The Urgent Care may also be reached at 307.675.5850.
Emergency Department
The hospital’s Emergency Department is located at 1401 West 5th Street. It is the best place for treatment of life-threatening medical problems and injuries such as heart attack, stroke, abdominal pain, dislocations, severe fractures, and severe pain. Patients are prioritized based on the severity of their condition. Onsite consultations from surgeons, cardiologists, internists, pediatricians, orthopedists, OB/GYNs, and other specialists can be obtained as appropriate, as are admissions to the hospital and transfers to larger facilities if needed.
When medical issues arise, knowing the most appropriate location to seek care can save you time and money. We wish you the best of health, but Sheridan Memorial Hospital’s outpatient services are here and ready to serve you when needed.
For more information visit Urgent Care vs Emergency Room.

By Sierra Gross Stallman, MD – Medical Director of Sheridan Memorial Hospital’s Internal Medicine Practice
We have all been affected by Covid-19, which is why we look for safe and effective ways To protect our families, communities, businesses and mental health by reducing disease burden, keep us from getting Covid-19, and allow us to resume social functions: Vaccines.
Pfizer-BioNTech and Moderna have been successful in developing Covid-19 mRNA vaccine. Researchers have been studying mRNA vaccines for decades, refining and accomplishing a standardized process for safe and timely production. Having this technology readily available to use allowed for rapid response to the pandemic in developing a safe and effective Covid-19 vaccine. Even though scientists promptly replied to demand with scaled, standardized vaccine development, mRNA vaccines have been held to the same rigorous safety and effectiveness standards as all other types of vaccines to get approval or emergency use authorization from the Food and Drug Administration (FDA).
What is mRNA? It is a messenger that provides information to our immune system. Once recognized, our immune system uses the information as a template to produce antibodies that can detect and destroy the virus causing Covid-19 for future infections. This takes the body a few weeks to complete, so it is possible that a person could be infected with the virus and get sick from Covid-19 just before or just after vaccination because the vaccine has not had enough time to provide protection. Covid-19 mRNA vaccine does not contain live virus; rather, it has harmless protein pieces found on the virus’s surface. The vaccine is given as an injection into the upper arm muscle in two doses separated by ~21 days for Pfizer and ~28 days for Moderna. This two-dose regimen conferred 95% protection against Covid-19 in persons age 16 or older. Side effects from the vaccine are similar to that of other types of vaccines and largely consistent with the appropriate response of the body’s immune system. Transient and mild local reactions such as injection site tenderness, redness, fever, fatigue, headache, and joint pain can occur. The CDC is monitoring reports of allergic reactions, and as of December 23, 2020, there were 21 cases of anaphylaxis out of 1,893,360 doses given. Anaphylaxis is a life-threatening allergic reaction that can occur rarely after vaccination, with onset usually within minutes. All reactions were treated and recovered. Worldwide there have been over 44 million vaccine doses administered in over 50 countries.
Who should get vaccinated? The goal is for everyone to get vaccinated against Covid-19 as soon as enough vaccine is available. Covid-19 can have severe complications, including hospitalization, admission to ICU, intubation or mechanical ventilation, or death, particularly to those at-risk. At-risk persons include any adult older than age 65 and adults of any age with certain underlying conditions such as obesity, type 2 diabetes mellitus, and smoking.
Due to the limited supply of vaccines around the country, Wyoming has a phased approach to ensure equity in vaccine allocation and distribution. The prioritization list can be found here and on the WY Department of Health website. Sheridan County is currently in phase 1b, including people who are 65 years of age or older. Sheridan Memorial Hospital is working closely with Public Health to distribute vaccines to our community as quickly and efficiently as possible. We anticipate it will take about two months to get through this current phase based on allocation supply.
If you fall into this category, call 307.675.4471 to schedule a vaccination time.
As always, reach out to your healthcare provider with questions or concerns regarding your health and the Covid-19 vaccine. Thank you, Sheridan, for sticking together, supporting our community, and doing your part to reduce the spread.
By Kristi Ramsey, RN, BSN, RCIS, CVRN – Sheridan Memorial Hospital Cath Lab Manager
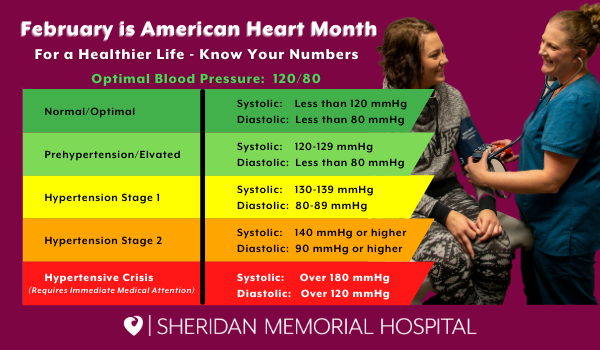
Did you know that nearly 1 in 2 Americans have high blood pressure and many people don’t even know they have it? That’s because there are often no warning signs. Having high blood pressure (also called hypertension) makes a stroke or heart attack much more likely.
High blood pressure is the force of your blood moving against the walls of your arteries. So when your blood pressure is too high, your heart is on overdrive. Over time, elevated blood pressure can weaken your heart, blood vessels, kidneys and other parts of your body.
There are many steps you can take to lower your blood pressure. It’s important to work together with your health care team to set your blood pressure goal, the reading you’d like to consistently see when your blood pressure is taken—and how you can best reach it.
We’ve gathered this information from the American College of Cardiology:
Living with High Blood Pressure
The goal of any treatment plan is to prevent or reduce the impact of high blood pressure and the onset of complications, including stroke, heart attack, heart failure and chronic kidney disease.
Lower is Better
Know your numbers! Your healthcare professional may talk with you about setting a “target goal.” A normal blood pressure reading is less than 120/80 mmHg.
Research shows that lower blood pressure goals improve heart health.
Lifestyle Changes are Key
Lifestyle changes are the main treatment for those with elevated or stage 1 high blood pressure. They are also important in treating individuals with stage 2 high blood pressure (>140 mmHG/>90 mmHG) and for good overall health. Healthy choices can go a long way in helping to lower your numbers and include:
- Getting regular physical activity
- Maintaining a healthy body weight
- Focusing on healthy eating (follow the Dietary Approaches to Stop Hypertension diet, limit salt and eat potassium-rich foods)
- Limiting alcohol (no more than one drink per day for women, two drinks per day for men)
- Smoking cessation
It’s important to cut back on the amount of salt (sodium) you consume, particularly if you are already eating a diet that is high in salt. The latest Dietary Guidelines for Americans recommend people consume no more than 2,300 mg of sodium per day—less than a teaspoon of salt. However, for people with high blood pressure or at risk for it, less than 1,500 mg of sodium per day is often the goal.
Stress also can cause your blood pressure levels to spike, so make sure to do things that help you relax and reset. Some examples include: listen to your favorite music, go for a walk, or take a yoga class.
Medications Play a Role
Some common medications used in treating high blood pressure include thiazide-type diuretics, calcium channel blockers, ACE inhibitors, aldosterone antagonists and beta-blockers, which may be considered specifically if the person has coronary artery disease after a heart attack or heart failure. You may need multiple medications, especially if your numbers are significantly above your goal.
It’s critical to take medications exactly as prescribed and report any side effects. Be sure to share a complete list of all the medications you take, including over-the-counter drugs and supplements.
The new guidelines lower the threshold for when treatment is needed. If you’re already being treated for high blood pressure, it’s a good time to review your treatment plan and decide with your care team whether your target blood pressure numbers should be lower. You might need to step up your lifestyle changes or medication, or both.
Track Your Blood Pressure
Tracking your blood pressure is a key part of managing it. Find out how often you should take and keep a record of your blood pressure readings. Having this information in hand can help your health care professional know what is working and when to adjust your treatment plan.
Other conditions, sometimes called secondary causes, might be triggering high blood pressure and should be taken into consideration. These conditions include sleep apnea, chronic kidney disease, certain medications, and adrenal or thyroid disorders.
Talk to Your Care Team
It’s important to talk with your healthcare professional about your blood pressure and any other factors that put you at risk for heart disease. Knowing your numbers can help you take steps to either prevent or lower high blood pressure.
If you don’t have a primary care provider, give our Internal Medicine practice a call at 307.675.2620 and they can set you up with a care team.

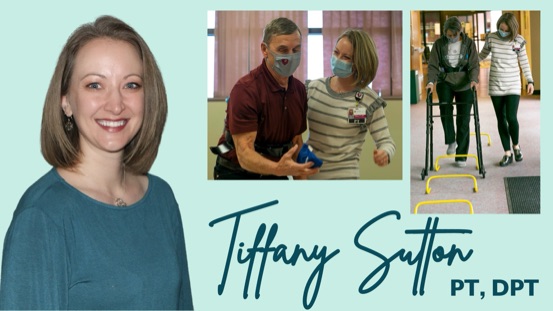
By Charlotte Walter, PT, DPT, ATC – Wyoming Rehab
If there’s one thing we can all agree on, it’s that 2020 was not the year we expected. Increased stressors and disrupted schedules are often accompanied by decreased exercise consistency and other poor health habits. Once bumped off the wagon, it can be difficult to dust ourselves off and clamber back up. If 2020 knocked you off your fitness routine or reminded you of the importance of starting one, read on.
A common barrier for individuals wanting to start an exercise routine is joint pain or stiffness. Luckily, exercising the right way has actually been shown to decrease these symptoms. To avoid flaring up joint pain, it is important to start smart. Take an honest assessment of your current exercise levels – if you are not currently exercising at all, jumping into a six-days-a-week-60-minutes-a-day high-intensity exercise program will cause a significant increase of joint loading. Instead, start by incorporating low-impact cardiovascular activities such as walking, dancing, cycling, swimming, cross-country skiing, or rowing with gradual increase in duration.
Strength training is another joint-friendly activity that strengthens the muscles surrounding the joint, which in turn will support the joint and reduce joint stresses. Good news is you don’t need a full gym set-up to get a good workout! Using bodyweight, resistance bands, or free weights can still load muscle groups enough to induce strength gains. No free weights around the house? Get creative with empty milk or water jugs filled with water, sand, or rocks.
Flexibility exercises are an excellent complement to aerobic and strength training activities. Moving a joint through its full available range of motion encourages circulation of joint fluid and helps to reduce joint stiffness. Gentle stretching or yoga routines are a great way to work this in.
Keep in mind, exercise is just a piece of the fitness puzzle. An effective workout is hard to achieve if you are short on sleep, hydration, or nutrition. Start smart and make small, sustainable changes that will have a long-term positive impact on your health. Additional sources of information about physical activity can be found from the CDC, the American Heart Association, the Department for Health and Human Services, and others.
Does all of this sound great, but you’re unsure of where to start? As with any new exercise program, you should consult your doctor to address any medical concerns that could limit exercise before beginning. If you have medical clearance but are stumped by persistent pain, previous injury, or balance concerns, take advantage of your knowledgeable sports medicine and orthopedic therapy team at Wyoming Rehab! Our therapists offer FREE screens and treatment recommendations on non-emergent physical impairments or injuries. Don’t let those aches and pains hold you back. The therapists at Wyoming Rehab can help guide you in the right direction to get your 2021 on track.
Armed with the right knowledge and a desire to improve our levels of health, there’s no reason to not make 2021 the comeback year we all need.
Find out more about what Wyoming Rehab can do for you: https://www.sheridanhospital.org/medical-services/rehabilitation-services/
Through January 22, Sheridan Memorial Hospital (SMH) has provided COVID-19 vaccinations to approximately 1,000 people in Sheridan County. That includes SMH employees and the priority populations of essential workers and people over the age of 70.
The side effects from the second dose of the vaccination received can include arm soreness at the injection site, minor swelling, chills, fever, fatigue and headaches. A few SMH providers have provided a short video documenting their experience receiving their second dose.
“I’m feeling hopeful, and very grateful,” said Erin Strahan, PA-C with the SMH Internal Medicine Clinic. “This is one chance to get back to normal life.”
“I have a little soreness in my arm but nothing that kept me from seeing my full complement of patients,” explains Dr. Elisabeth Scalva, with the SMH Women’s Clinic. “I’m feeling grateful to be protected and to protect my family, my patients and mostly this community.”
“Initially, I had a little bit of a sore arm,” said Dr. Ian Hunter, Sheridan County Public Health Officer. “Later that night, I woke up and had a fever… I just didn’t feel good for about eight hours, then that resolved.”
Currently, all doses of the vaccine SMH has received or is scheduled to receive is already spoken for. This includes 975 doses of the Pfizer vaccine scheduled for delivery on January 25 or 26.
SMH is accepting calls to place essential workers and people over age 70 on a wait list. Once more information is available regarding additional vaccine, SMH will be working through the wait list to conduct call backs and schedule additional vaccination appointments.
If you have been designated an essential worker or are over the age of 70 and you want to receive the vaccine, please call 307-675-4471 and leave your name, date of birth and phone number. You will receive a call back within the next business day to be placed on the wait list.
Click here for more information on the COVID-19 vaccine in Sheridan County
Click here for the Wyoming Department of Health Phase 1a and 1b COVID Vaccination Priority List

To date, Sheridan Memorial Hospital (SMH) has received approximately 970 doses of the Moderna COVID-19 vaccine. That includes 700 doses in late December and 270 doses in mid-January.
Another 975 doses of the Pfizer vaccine are scheduled to arrive January 26, and Dr. John Addlesperger, SMH Chief Medical Officer, says appointments are currently being scheduled to administer those doses as well.
“We have scheduled appointments for every dose of vaccine we have received so far or are scheduled to receive,” said Addlesperger. “Currently, demand is outpacing the supply chain for the vaccine. It’s good to see so much interest. This vaccine will be a big help in allowing us to return to life as we remember it before all the COVID protocols we have been following the last 10 months.”
Even though the vaccine schedules are currently full, SMH is still accepting phone calls and putting eligible people on a waitlist to be scheduled at a later date when the next vaccine shipments arrive in February.
“Our process for developing the waitlist and getting people scheduled is simple, but it takes a while to execute due to the high volume of calls we are receiving versus the supply of vaccine we have received,” said Tim Grollmes, SMH Internal Medicine Practice Administrator. “We don’t know what quantity of vaccine we are going to receive from month-to-month. That makes it tough to schedule.”
In making vaccine appointments, SMH is following a phased priority list established by the CDC and Wyoming Department of Health. Phase 1a is primarily essential workers and Phase 1b includes essential workers as well as people from the general public over 70 years of age. Click here – Phase 1a and 1b COVID-19 Vaccination Priorities – to see the complete priority list.
“Right now, we are scheduling vaccinations for essential workers and people 70 years of age and older,” Grollmes said. “Once we get through those two populations, we will move on to the rest of the priority list. It could take a couple of months depending on how many people want the vaccine.”
Since each of the vaccines requires a booster shot follow up (Moderna at four weeks and Pfizer at three weeks), SMH is scheduling patients for their booster shot immediately after receiving their first shot, before they leave the clinic.
Those who have been identified as essential workers or are 70 years of age or older and want to receive the vaccine, please call the SMH COVID Vaccination Clinic at 307-675-4471. More information is also available at the Sheridan County Public Health website – https://www.sheridancounty.com/covid-19/covid-19-vaccines/.
“Until we can get the majority of our community vaccinated, it is important that we remain diligent in following the COVID protocols set forth by the CDC,” Addlesperger added.
Those protocols still include: staying home when ill, wearing a mask, socially distancing, washing your hands and disinfecting high traffic surfaces.

Wyoming Rehab’s Licensed Physical Therapist Charlotte Walter describes her approach to creating individualized treatment plans to help each patient achieve their goals. In this video, she highlights a treatment plan she created for Pat Hall, who came to Wyoming Rehab with concerns of balance and mobility.
Do you have a condition or impairment preventing you from reaching the recommended amounts of physical activity? Don’t continue to put your health at risk. Find out how physical or occupational therapy may help. Reach out to Wyoming Rehab at 307.674.1632 if you would like to schedule a FREE Screen/Treatment Recommendation for a Non-Emergent Physical Impairment or Injury.

Connie Bachel, a longtime employee of Sheridan Memorial Hospital (SMH), contracted COVID-19 in mid-September.
Bachel and six of her co-workers at the SMH Urgent Care tested positive for the coronavirus, each exhibiting different symptoms. For the next two weeks, they recovered, checking in on each other’s progress and offering words of encouragement.
In early October, Bachel was feeling better, if not fully energized. But by mid-October, COVID-19 reasserted itself in full force, even worse than before. Bachel, suffering from gastrointestinal symptoms, did not immediately want to go to the emergency room.
“It was so embarrassing — I didn’t want to do that in my own sandbox,” she said. “But my husband said, ‘No, you’re going to have to be a patient.’”
Bachel was immediately admitted and placed in a COVID-19 isolation wing.
SMH has two dedicated wings for COVID-19 patients: one in the Intensive Care Unit for critically ill patients and the other on the Med Surg floor for those like Bachel who need to be admitted but don’t need ventilators. Experts across SMH departments have worked together to ensure these wings are as safe as possible for patients and staff.
“It’s very scientific,” said Lacey Johnson, the Med Surg Manager at SMH.
Because COVID-19 is an air-borne disease, Johnson explained, one of the most important elements of the isolation wings is the air flow. Partitioned off from the rest of the hospital, the hallways and rooms have negative air pressure. Instead of filtering, cleaning, and recirculating the air like in most buildings, the mechanics of the hospital bring in air and then send it directly back outdoors, without returning to the hospital. All doors and windows must remain closed to maintain the seal.
In addition, the few dedicated staff members who are allowed into the wings must be in full PPE: gown, gloves, booties, N-95 mask, eye cover, and hair bonnet or a capper.
The cleaning staff for the COVID-19 wings uses “terminal cleaning” agents and gear, the same used in Operating Rooms, a lengthier and more involved sterilizing process.
Perhaps most importantly, the medical team must be conscientious of the time spent in the wings.
“If we go in to deliver medications, we get them all at once,” Johnson said. “We bathe patients, change the bed, etcetera, all in that time frame.”
While crucial for safety, the COVID-19 isolation wings can be just that — isolating.
At the time, Bachel’s daughter, Megan Perkins, was a registered nurse at SMH. Due to the strict safety protocols, even she could not enter the room — only the dedicated on-duty nurse could be admitted.
Perkins herself had worked in the COVID-19 wing. She had seen family members’ frustration at being kept apart and knew the importance of lifting patients’ spirits when at their most ill.
“As a nurse, it’s hard to see your patients struggle that way,” Perkins said. “I saw how much it dropped their mood and their affect. It hurts people’s sense of well-being when they’re so isolated. But I knew why we were doing it and that it had to be done. Just from taking care of previous COVID patients, I knew what my mom was going through.”
So, like many of her patients’ family members, Perkins found a safe way to engage with her mom. Bundling up against the October snowstorm, Perkins headed to the window outside of her mom’s room.
“I called her on the phone, and we sat by the window and drank coffee and pretended the window wasn’t there,” Perkins remembered.
Over the next few days, these chats meant the world to Bachel. And the support continued to flow. Friends, family, and co-workers visited — even her daughter’s friends popped by to throw snowballs and wave an encouraging sign out of the window.
“It means more to the people in that hospital bed than you know,” Bachel said, choking up.
After four days of treatment, Bachel showed improvement, tested negative for the contagious antigen, and was released to recuperate at home for another week. She gradually started working again, building up her hours and strength slowly.
Today, Bachel feels “100% completely better.” When she looks back at the fall, she realizes just how ill she was.
“After about a month and a half of being so sick, when you do finally feel good, you realize just how terrible you felt,” she said. “I’m so glad I went in because I don’t know what would have happened. They took great care of me.”
Back at work, Bachel — already a compassionate person — feels even more empathy for patients and family members after her experience. She sees the same change in her co-workers who also recovered from the disease.
“I know how they feel,” Bachel said. “I feel it. It’s real. We all need to wear our mask and practice hygiene. It’s just here. It’s here all the time.”
Her daughter agrees.
“I just hope that people understand what these regulations are for and what the mask mandates mean for certain people,” Perkins said. “Until it becomes personal for you, you don’t really take it to heart. Until you realize one of these patients is a mother or a grandmother — because one was your mother — you just don’t realize the detrimental effects. I think all the people who make a stink about our mask mandates need to take a step back and realize it’s about being a good person.”
In this new year, we want to remind you to take care of yourself. With all of the talk and concern about the COVID-19 virus, it’s a very confusing time. One important thing you can do is to pay attention to your health.
January is Thyroid Awareness Month. What an appropriate time to call attention to the various health concerns connected to the thyroid. We’ve gathered information in this column to help you learn more about the most common thyroid conditions. Most of us have heard about the thyroid, but we may not realize its importance. If you have questions about thyroid diseases or any other concerns, we urge you to visit your healthcare provider.
What Is The Thyroid?
The thyroid gland is located in your neck just below the Adam’s apple. It may be small, but it has a significant impact on your health, controlling your metabolism and creating new proteins. This butterfly-shaped gland is part of the endocrine system, directly affecting almost every organ in the body. It is responsible for regulating skin integrity, menstrual cycles, calcium levels, and the nervous system, heart and cholesterol levels. In addition, it controls brain development, your body temperature, respiration, metabolism and fat production.
Thyroid problems begin to occur when the thyroid gland produces too much hormone or not enough. There are several illnesses and diseases related to the thyroid, including hyperthyroidism, hypothyroidism, Hashimoto’s disease, Graves’ disease, goiter and thyroid cancer. We will address the two main thyroid conditions: hypothyroidism and hyperthyroidism. Each has an opposite set of symptoms.
Hypothyroidism, when the thyroid is working more slowly than it should, is most common in patients over 60, and the incidence of this disease increases with age. People with hypothyroidism tend to experience weight gain, irregular menstrual cycles, slow heart rate, muscle aches, constipation, voice changes and the loss of body hair.
Conversely, Hyperthyroidism is where your thyroid works more actively than it should. Hyperthyroidism is most common in patients under age 50 and is marked by an enlarged thyroid gland, plus insomnia, a rapid heart rate, anxiety, weight loss, increased appetite, emotional instability, increased nervousness and anxiety, excessive perspiration, and diarrhea. The senior hypothyroidism patient may only have one or two of these symptoms. Although hyperthyroidism is associated with more energy, the body breaks down after a while, leading the person to feel more tired.
What causes the thyroid to malfunction?
Most thyroid malfunctioning is caused by an autoimmune response. The immune system of someone with hypothyroidism sees the thyroid as a threat and begins to attack it, causing inflammation and damage, leading to a decrease in hormone production. The immune system of someone with hyperthyroidism compels the thyroid, unnecessarily, to over-produce hormones.
A prevailing theory behind why women are more susceptible to thyroid disorders is because the female immune system is more pliable than the male immune system, capable of revving up or winding down in response to certain biological events, specifically pregnancy. When a woman becomes pregnant, the baby is seen as a foreign object in the body. To prevent the growing fetus from being damaged, the mother’s immune system must be suppressed.
The only way to know for sure if you have thyroid disease of any type is to have a blood test that measures your thyroid hormone levels. To confirm whether there is a thyroid concern, your physician may perform a thyroid-stimulating hormone test. This blood test measures whether the gland is working properly. It is highly recommended to get tested if you are a senior over 60, have family members diagnosed with the disease or believe you have symptoms.
Diagnosing thyroid disease in seniors can be difficult because some of the symptoms are also associated with aging or other medical conditions. It is natural to assume symptoms such as memory issues, constipation or weight gain are part of the aging process. However, these can also be signs of thyroid disease.
Causes & Treatment Of Thyroid Diseases
There are several causes, but some common causes can be attributed to autoimmune disease, certain types of medications, thyroid surgery or radiation therapy. Anyone can develop thyroid problems, but women age 60 or older seem to be more susceptible.
Hypo- and hyperthyroidism can be treated with medication, iodine, or hormones, and the other conditions can be addressed with therapy or surgery. Luckily, thyroid prescriptions can usually get symptoms under control. It is important to keep abreast of new symptoms that may occur because medications may need to be changed or dosages increased or decreased. It is also critical to be sure to take medication at the same time every day.
The nonspecific nature of symptoms can make thyroid conditions challenging to diagnose. If you feel you may be having problems with your thyroid, your best option is to bring your concerns to your primary care physician’s attention.
If you have questions, the healthcare professionals at our Internal Medicine Practice can help.
Call 307-675-2650 to schedule an appointment today.