In November 2020, as the world reeled from the effects of the COVID-19 pandemic, Laura Holsinger’s life changed in a far more personal way. Just days after discovering a small, rapidly growing lump in her breast, she underwent a mammogram, ultrasound and biopsy at Sheridan Memorial Hospital. Soon after, Holsinger’s care team confirmed her worst fear: stage two breast cancer.
Up until that point, Holsinger had never faced any major health concerns.
“I’d never spent a night in the hospital or broken a bone, and my family had no history of breast cancer,” she said. “And then boom — all this craziness happened.”
Holsinger had a lumpectomy with Dr. Sara Maguire, MD, FACS, to remove the lump. After surgery, part of the tissue was sent to a lab for an Oncotype DX test — a genomic test that examines the activity of specific genes within cancer cells to estimate how aggressive the cancer might be and how likely it is to spread. Based on the test results, patients receive a score that helps determine whether the potential benefits of chemotherapy outweigh its side effects. For women younger than 50, a score of 25 or lower suggests a low risk of recurrence, meaning chemotherapy is unlikely to provide significant benefit. For women older than 50, a score of 20 or lower indicates the same.
Holsinger’s score was 67.
“Dr. Maguire said it was the highest score she’d seen since joining the hospital,” she recalled.
Holsinger started chemotherapy at the Welch Cancer Center on Feb. 1, 2021. Due to COVID-19 restrictions at the time, patients were not allowed to have visitors or loved ones accompany them to appointments.
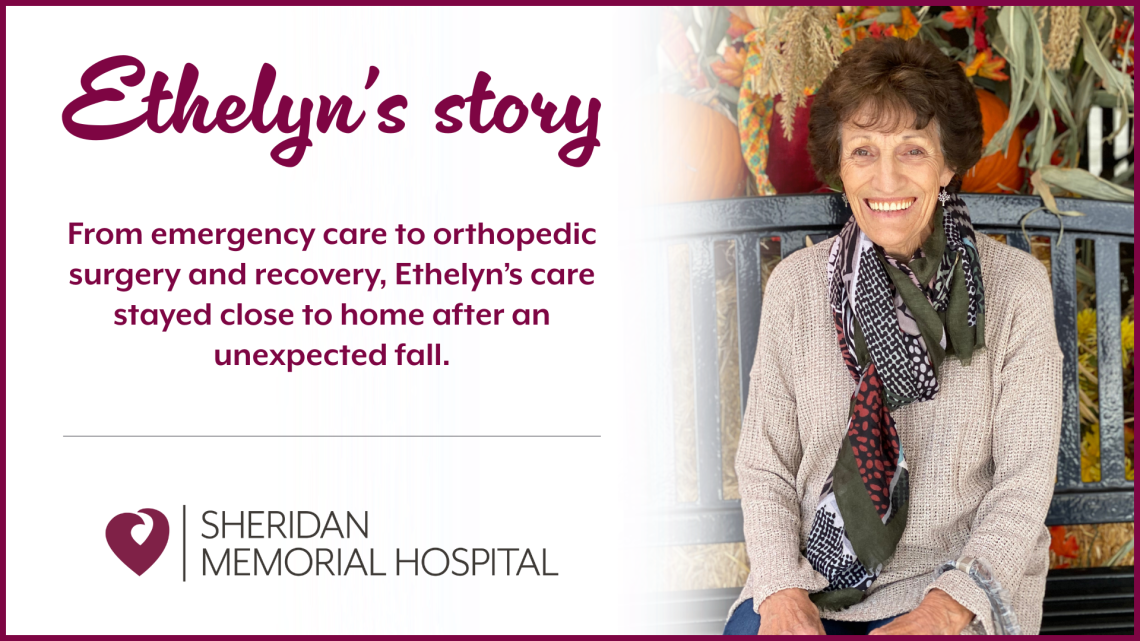
“I drove myself to and from appointments,” Holsinger explained. “I was grateful I could get treatment here in town, so then I didn’t have to drive out of town by myself while I wasn’t feeling well.”
Although Holsinger felt grateful to receive care close to home, the experience proved far from easy.
“The only appointment I could bring my husband to was the one where we decided my course of treatment,” Holsinger said. “I can’t tell you how terrified I was the first time I went in for chemo, being surrounded by nurses in what looked like hazmat suits because the medicine was so strong, and realizing they were about to put it in my body.”
Compassionate care team
Despite her initial fear, behind those layers of protective equipment were compassionate caregivers ready to comfort and reassure her every step of the way.
“I appreciate the nurses at the Welch Cancer Center so much,” Holsinger reflected, tears welling in her eyes. “I can’t even describe how comfortable they made me feel, especially knowing I was there alone. They knew I was going through probably the most awful period of my life up to that point, and they were focused on making it the best experience they could despite everything. And they did a really, really good job at that.”
Providing comfort during a patient’s most vulnerable moments is something the nurses at the Welch Cancer Center understand deeply. One nurse reflected on how meaningful it is to support patients through those first, often overwhelming days of treatment.
“I’ve always enjoyed being a patient’s nurse on their first infusion day, so I can give them a sense of security and genuine compassion,” said Lori Karajanis, RN, Oncology Nurse Navigator at the Welch Cancer Center. “It’s what we would all want if it were us in that chair. That is the best part of nursing, in my opinion.”
That compassion made a lasting impression on Holsinger. One of Holsinger’s favorite memories happened on her very first day of treatment. A nurse asked what her favorite colors were, and Holsinger said she preferred “true” colors—more natural, earthy tones.
The nurse disappeared for a few minutes and returned with several other nurses, each holding a handmade quilt donated by a local quilting club. Holsinger chose the quilt that matched the earthy colors she described earlier, and the nurses laughed. It turned out that the nurse who asked about her favorite colors had a knack for picking patients’ favorite blankets—and, as the others joked, she always “won.”
Smiling at the memory, Holsinger added, “That was really nice. Really fun. I didn’t tattle on her. I let her have her glory.”
Her appreciation extended well beyond that single moment and beyond the nursing staff. Holsinger spoke highly of the entire Welch Cancer Center team and the way each person contributed to her care.
“The physicians were always reasonable,” she said. “You’re not just a number to them. You can express your concerns to the providers at the Welch Cancer Center and they listen to you. They talk it out with you and reason on it. Dr. Megan Ratterman, DO, was very good at that. Even over the phone, her voice is so caring and concerned. It’s like talking with a family member.”
That sense of compassion is no accident. It’s woven into the culture of the Welch Cancer Center—something in which the team takes immense pride. Welch Cancer Center Manager Megan Ripley, RN, OCN, explained how deeply teamwork and empathy shape the patient experience.
“Our team demonstrates exceptional compassion for patient-centered care, and teamwork is at the heart of everything we do,” she said. “Patients can truly feel the positive impact of a cohesive and positive work environment when they receive care in our facility.”
Treatment & path forward
Holsinger received chemotherapy from early February through the end of April 2021, followed by 20 rounds of radiation throughout May. Through it all, she worked hard to stay positive.
“My family was terrified,” she admitted. “I was terrified, but I tried really, really hard the whole time to stay positive, because I truly believe the mind can help the body heal.”
Now, five years after her diagnosis and recovery, Holsinger still faces moments of uncertainty. A recent blood test and mammogram have raised concerns that she and her care team continue to monitor closely. Yet even as she faces these challenges, Holsinger does so with remarkable resilience.
“I’m not trying to be paranoid, just proactive,” she said. “And if I have to go through it again, I’m glad I’m here and can go back to the Welch Cancer Center, because I trust them completely. It’s convenient that they’re right here in town, and they’re the best people I know for the job.”
Today, Holsinger is part of Sheridan Memorial Hospital’s Environmental Services and Laundry teams. Recently, she had the opportunity to clean the Welch Cancer Center for the first time since her treatment.
Inspired by the compassion she experienced firsthand at the Welch Cancer Center, Holsinger now gives back by donating a portion of her paycheck to support care there as an Employee Partner of the Sheridan Memorial Hospital Foundation.
“It’s my little way of giving back,” she said.
For Holsinger, being a cancer survivor means more than overcoming an illness. It means gaining a new perspective on life.
“This experience gave me so much empathy,” she explained. “And things aren’t as earth-shattering as they used to be, because you’ve already been through the earth-shattering part. You know you can handle everything else.”
Holsinger has also found purpose in supporting others going through similar experiences.
“I’ve sat with a friend during her first day of chemo because I know how scary it is,” she said. “I was able to encourage her and tell her, ‘You’re going to be OK. I’ve been through this, and I’m still here.’”
For those currently fighting cancer, Holsinger offered simple but powerful advice:
“Just fight, stay positive and kick cancer’s butt.”
For more information about the Welch Cancer Center, visit welchcancercenter.org or call 307.674.6022.