After local attorney Deb Wendtland saw the moving SMH video asking our community for their help to slow the spread of Covid-19 by wearing a mask, she had an idea to support frontline healthcare staff. Deb went to work with her close friend Julie Gerlach to raise these funds and
SMH’s Own Megan Ripley, RN Shares Her Journey of Wellness & Diabetes
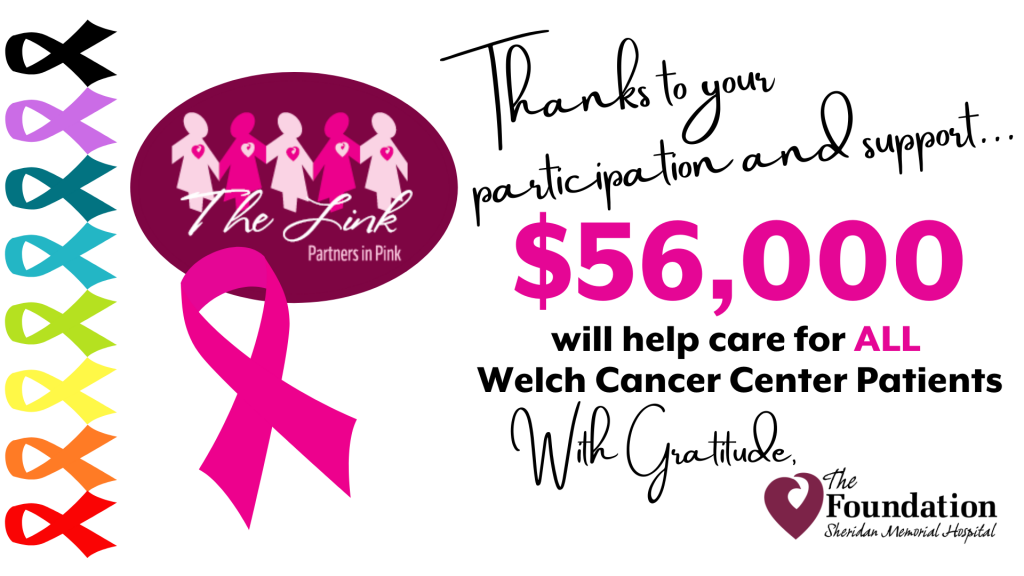
$56,000 Raised Through Hospital Foundation’s Virtual Link - Partners in Pink Event
We are excited to welcome Dr. Elise Sylar to the staff at Sheridan Memorial Hospital Internal Medicine. She is now accepting appointments for adults and adolescents 16 and over. Please call 307.675.2650 Option 4 to schedule your appointment today.
Celebrating Physical Therapist at Sheridan Memorial Hospital's Wyoming Rehab
Taylor Wendtland came to Wyoming Rehab after living with moderate to severe low back pain for nearly 10 years. The pain affected his ability to participate