Welcome to Sheridan Memorial Hospital
1401 West 5th St. Sheridan, WY — 307.672.1000
SMH Friendly Faces

This month’s W.O.W Employee of the Month is Welch Cancer Center Pharmacist, Sarah Opitz. As a mom to three young girls, Sarah was motivated by her family to start her wellness journey.
“Family is huge for me. I wanted to set a good example for my family and show them what it looks like to maintain overall good health,” said Opitz. “I wanted to be active, exercise, and maintain a healthy weight so that I can be there for them.”
A few months ago, Sarah was motivated to make positive changes after experiencing what many mothers go through after nursing.
“Having young girls, I was nursing for a long time, and I used it to justify eating whatever I wanted because I could do it without gaining weight. Now that stage is over and I realized very quickly that my clothes were fitting tighter,” said Opitz. “Once I noticed I was putting on a few pounds I realized I needed to be more conscious of what I was eating and that I needed to be more active. Once I realized I could do better and should be better, I started to make a few changes.”
Sarah started by making small changes, including exercising and monitoring her portions.
“It wasn’t big and I didn’t really change my diet, I just started being more conscious of the amount I was eating. I also started going to the gym more often,” said Opitz.
She started making sure she had veggies and fruits with meals and paying attention to what was going on her plate.
Before she started making changes, Sarah relied on the activity she got around the house and with her family. She started by creating an exercise routine that fit her schedule.
“I had to find times in my schedule that would work for me. I go to the gym on weekends and Wednesday mornings when my girls are at daycare,” said Opitz.
After she started making time for the gym she started noticing the positive benefits of exercise.
“It helps my mood and my energy, it definitely perks me up,” said Opitz.
Like many others, Sarah’s wellness routine has been interrupted by COVID-19, but she’s found ways to adapt.
“Looking on the bright side, we know that Spring is just around the corner. With the warmer weather we can spend more time outside doing things,” said Opitz. “You’re supposed to stay at home, but that doesn’t mean you have to stay in your house. Bryan, the girls, and I have been able to get out a lot, going for walks, bike rides, and taking the girls on their scooters.”
When asked what advice she would give to others starting their wellness journey she discussed the importance of making time for yourself and simple changes.
“My advice would be that if you’re feeling overwhelmed, or you want things to be better, or you need more structure, just stop and think about simple changes you can make. Find a few minutes to relax or go to the gym,” said Opitz. “The hardest thing for me was just deciding to do it and start. Once I made the choice to start doing it, I found it wasn’t as hard as I thought.”
Sarah uses the MyFitnessPal app to log what she eats and to calorie count. The app has helped her keep her wellness routine.
“Just taking the time to do those entries was daunting. I use the MyFitnessPal app because it’s user-friendly, quick, and slick. It helps make time not a factor. The thought of having to make a change was difficult. “I like routine and liked the way things were so I was lax and I ate whatever and did whatever. I didn’t have a routine and I needed one,” said Opitz
“I have to make sure that I have time for myself, even if it’s just a few minutes, it helps me relax,” said Opitz. “I really enjoy reading but since we had kids time is short and hobbies have fallen by the wayside. I’ve made time to read again and I also read with my daughter before she goes to bed and I really enjoy it.”
As a mom, Sarah knows the impact of making time for yourself and the benefits that a healthy lifestyle can have.
“These changes haven’t made me the perfect mom but they have definitely helped,” said Opitz. “I still struggle with the everyday challenges of being a mom, but it has helped and I can tell a difference.”
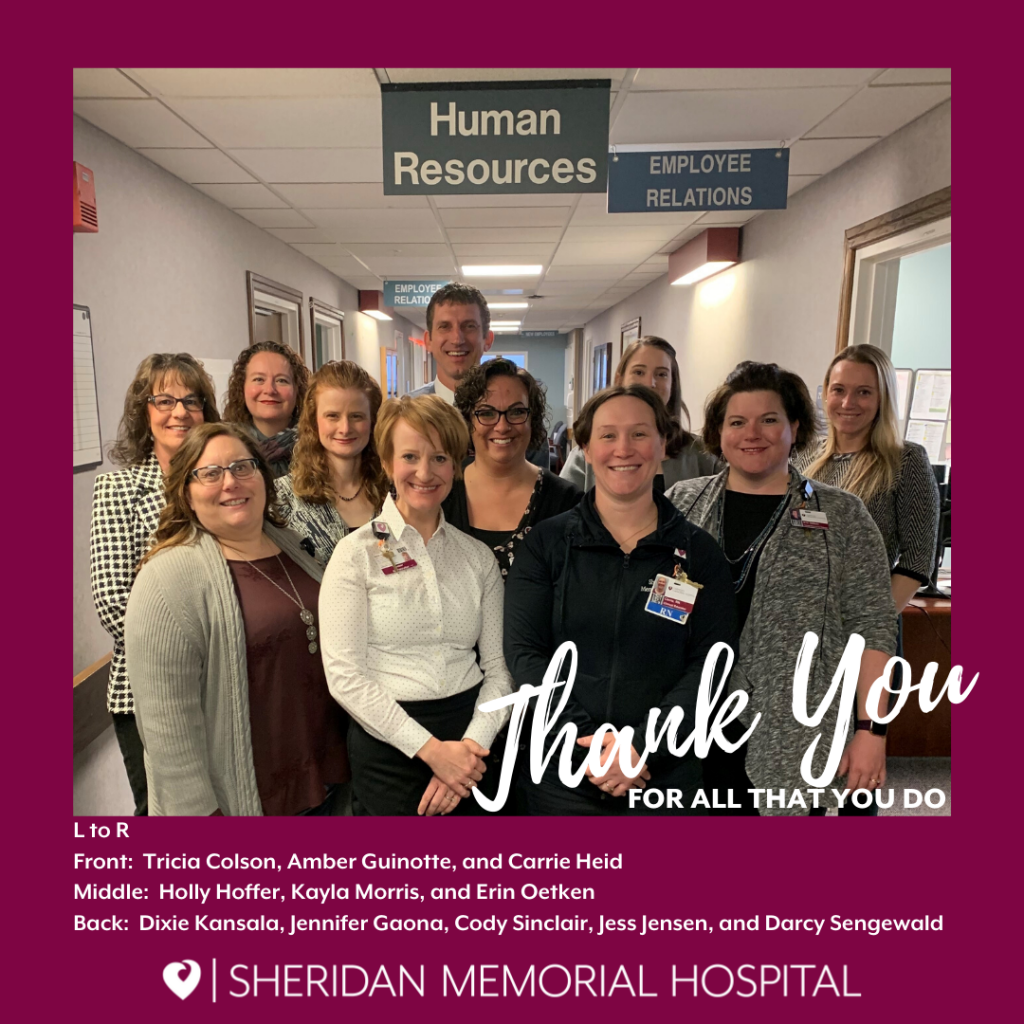
A heartfelt, THANK YOU to our Human Resources department. Healthcare Human Resources Week–the third week of March–is designated to recognize human resources professionals in healthcare organizations for their important role. We salute our HR department for the many ways they care for our employees so they can keep taking care of you!

March is National Nutrition Month and a great opportunity to recognize our incredible Registered Dietician Nutritionists at Sheridan Memorial Hospital. Our RNDs are experts in food and nutrition and are qualified to support a variety of patient needs including meal planning, nutritional counseling, assessments, progress tracking and much more. To learn about the common reasons to consult an RND, check out the link below:
If you’re interested in seeking the expert, science-based advice of our RNDs, contact your primary physician for a referral today.
On March 11th we celebrated Registered Dietitian Nutritionist Day and we were able to learn some fun facts about each of our RNDs. Get to know them below!
Jordan McCoy MS, RDN, LD (Outpatient/Dialysis Dietitian)
Q: Favorite way to spend a Saturday afternoon?
A: Fly fishing on either the Big Horn River (MT or Thermopolis) or the North Platte with Trinity, my
Boyfriend.
Q: What was the last thing you took a photo of?
A: A rainbow trout at the North Platte in Casper.
Q: Does pineapple belong on pizza?
A: Of course….as long as there is lots of cheese to go with it.
Q: Favorite pie?
A: No pie, only cake!
Q: Summer, Winter, Spring or Fall?
A: OHHH hard to pick! How about SUMMALL a mix of Summer and Fall.
Q: Morning person or night person?
A: Morning! Bring on 4 a.m.
Megan Sexton MS, RDN, LD (Clinical Dietitian)
Q: Favorite way to spend a Saturday afternoon?
A: Hiking in the Big Horns with my two fur-babies.
Q: What was the last thing you took a photo of?
A: The walk-in shower we just remodeled ourselves.
Q: Does pineapple belong on pizza?
A: Absolutely not! No warm fruit for me.
Q: Favorite pie?
A: Doesn’t really matter, I’m in it for the crust.
Q: Summer, Winter, Spring or Fall?
A: Fall for all the hiking, fishing, hunting, and crisp air I can get.
Q: Morning person or night person?
A: Morning, my bedtime keeps getting earlier.
Sarah Sommers RDN, CDE, LD (Outpatient Dietitian/Diabetes Education Coordinator)
Q: Favorite way to spend a Saturday afternoon?
A: Cross country skiing in the Winter or canoeing the Tongue River in the Summer.
Q: What was the last thing you took a photo of?
A: A snow-covered landscape with the Bighorns in the background.
Q: Does pineapple belong on pizza?
A: The more veggies on the pizza the better…but I don’t want fruit on my pizza.
Q: Favorite pie?
A: Do brownies count?
Q: Summer, Winter, Spring or Fall?
A: Definitely Winter – I love the crisp cool mornings and the snow! But ask me in the Fall and I might say then too.
Q: Morning person or night person?
A: Morning without a doubt.
Sheridan Memorial Hospital is very proud of our RNDs and the amazing work that they do to provide our community with excellent patient-centered care.

This month’s W.O.W Employee of the Month is Wyoming Rehab Physical Therapist, Darrin Goyn. Wellness has been a part of Darrin’s life from a young age and running was and continues to be, one of his favorite activities.
“I grew up outside of town and we would ride bikes all over the place. My two older brothers had bikes and for whatever reason, I didn’t have one so the only way I got to go with them was to run. I think that’s where I got my start in running,” said Goyn.
Darrin was involved in athletics throughout school including track, cross country, and wrestling. He also had the opportunity to compete in track at the college level but decided not to. After high school, he still enjoyed running and continued to do it throughout his life for leisure as well as competing in races.
“I started out with 5ks, then 10ks, and then a few half marathons. I’ve never done a full marathon. In the last 4 – 5 years I started doing trail running which I enjoy a lot more and the trails are easier on my legs,” said Goyn. “I’ve done the Big Horn Trail run: the 18 mile and the 52 mile. I trained a while for it and everything went well and I enjoyed it.”
Outside of running, Darrin enjoys woodworking, remodeling homes, and gardening with his wife. It’s also important for him to stay active at home and he’s not someone who can’t sit for very long. Along with staying active, he also prioritizes a healthy diet.
“My biggest motivation is general health and stress reduction. I just eat a healthy well-balanced diet. I try to eat more fresh food, watch the sugars and the carbs, but I still indulge. Just a good overall general healthy diet. My wife is a good cook so that helps,” said Goyn. “My wife and I both eat wild game so we don’t buy a whole lot of other meat because we know how it’s processed. We do a lot of fresh vegetables and fruits and don’t buy too many canned items.”
The advice he would give to others who are ready to make lifestyle changes is to focus on consistency and to know your limitations.
“The biggest part for anyone is the consistency of doing it. We’re all creatures of habit that have a tendency of getting out of the habits that we have worked to get into. The consistency of stressing the body and making sure you’re not injured is important to maintain a general fitness level and staying active,” said Goyn.
He also emphasizes the importance of eating a healthy diet and avoiding certain foods.
“Number one: stay away from fast-food restaurants and avoid eating out too much. Especially when you’re going out and spending money, you feel like, oh I have to eat all of this because I bought it,” said Goyn. “Focus on quantity and portion control and avoid carbonated drinks as much as you can. Just focus on eating fresh food and good lean meats.”

By Cassie Mullins, RN Cardiopulmonary Rehab Supervisor at Sheridan Memorial Hospital
In Sheridan, we are lucky to have many services to support heart health, from the cardiology team at the Heart Center, to our Cardiac Catheterization Lab and state of the art ICU at Sheridan Memorial Hospital. After having a heart attack, being diagnosed with heart failure, or after a heart procedure like a coronary artery bypass, coronary stent placement, or valve replacement, Sheridan Memorial Hospital’s nationally accredited Cardiopulmonary Rehab program provides support to help you recover.
According to the Centers for Disease Control and Prevention, someone has a heart attack every 40 seconds in the United States, and heart failure was a contributing cause of 1 in 8 deaths in 2017. After a major cardiac event, many are scared or uncertain of what to do to get themselves back on track. This fear and uncertainly can come from both being told something went wrong with your heart and from trying to learn a whole new set of “rules” to follow. New foods, new medications, new appointments, and new recommendations regarding physical activity can lead some to feel overwhelmed and underprepared for living a healthy life as a heart disease survivor.
Cardiac rehab plays a huge role in reducing the potentially devastating effects of heart disease. It is here that patients are given guidance and structure to help develop the necessary skills to face their new reality.
In cardiac rehab patients see other people like themselves exercising, socializing, and learning how to manage their heart disease with help from nurses, pharmacists, and dietitians. The foundation of cardiac rehab is physical activity. We monitor your heart rate and rhythm with a heart monitor that you wear during exercise, and check your vital signs before, during and after exercise. This information ensures that staff has the ability to see how your heart is reacting to physical activity in real-time. We work with patients to encourage a slow and safe increase in physical activity. In addition to exercise, at Sheridan Memorial Hospital’s Cardiac Rehab program we also provide education on cardiac disease, exercise safety, a heart-healthy diet, stress management, and medications.
Cardiac rehabilitation is recommended by the American Heart Association and covered by Medicare and many insurance companies. Studies have shown that participating in cardiac rehab substantially reduces the risk of death for individuals who have received a qualifying diagnosis or cardiac procedure. People who attend cardiac rehab programs live longer, are less likely to have a heart attack, and are less likely to be hospitalized. Yet most eligible patients don’t participate at all, let alone complete the recommended number of sessions.
Cardiac rehab has three phases. The first phase is the time immediately after a heart attack or procedure. The second phase is the monitored exercise phase. During this time your doctor can order 18, 24, or 36 closely monitored exercise sessions for you to complete. We encourage our patients to work up to exercising 3 times a week with us. After graduating from the second phase, we encourage our patients to continue to exercise! During the third phase, we provide the opportunity for our patients to continue exercising in our gym with less monitoring. The ultimate goal is for our patients to feel safe and confident participating in whatever kind of exercise they enjoy doing, whether that is in a cardiac rehab setting, at home, or in the community.
If you have had a heart attack, heart failure, or a heart procedure, ask your doctor if you could be eligible to be enrolled in cardiac rehab. For more information call Cardiopulmonary Rehab at Sheridan Memorial Hospital (307) 672-1062.

By Megan Sexton, RND
Which came first: the junk food or the memory decline? This question is being investigated currently by researchers and has revealed a strong correlation between a diet high in sugar and saturated fat with decreased memory function. The mounting evidence points to the significant impact a Western pattern diet likely has on the neurocognitive functions of our hippocampus (a small region in the brain). Our hippocampus is thought to be the control center that regulates motivation, emotion, learning, and memory. Bottom line: as saturated fat and sugar increase presence in a person’s diet, memory function declines.
The term Western pattern diet has been used interchangeably with the standard American diet and is defined as a high intake of red meat, processed meat, pre-packed foods, fried foods, high-fat dairy, refined grains, high-fructose corn syrup, and high-sugar beverages. Additionally, as these food-types increase, the amount of whole fruits, vegetables, fish, legumes and whole grains consumed decreases. Consuming a standard American diet carries other proven complications such as the increased risk for diabetes, heart disease, stroke, constipation, and weight gain. In other words, the evidence for people of all ages to move away from a standard American diet is very compelling and has been long-standing. But the rapidly growing evidence for the negative impacts of an American diet on memory function should make older adults prioritize evaluating their personal diet.
When I ask older adults why they depend on pre-packaged foods, fast-foods, and convenience foods for the majority of food choices, several explanations emerge. The decrease in energy and mobility, flavor and texture changes, dental issues, income restraints, and emotional life events (such as moving homes or loss of partner/loved-one) are the most common reasons. While these are valid reasons to seek out ways to ease the burden of food choice, we can’t ignore the probable impact these foods are having on memory decline.
There are several ideas that can be implemented to help consume high-quality foods for older adults. Sheridan has wonderful resources in Meals-on-Wheels and Designing Dinners that offer homemade meals that can be brought home for reheating. Grocery discount days, grocery delivery and a variety of grocery price-points all help to alleviate some of the cost burdens. I also encourage older adults to think outside of the box; quality food items don’t have to be combined into a whole meal to be beneficial. Having nutritious foods that require minimal assembly can make up the bulk of your calorie intake. Foods such as eggs, packaged tuna or salmon, low-fat cottage cheese, low-fat cheese sticks, low-fat Greek yogurt, hummus, nut butters without added sugar, mixed nuts, microwaveable frozen vegetables, low-sodium canned beans, sunflower and pumpkin seeds, whole-grain bread, microwaveable brown rice, and more.
The social and emotional aspects of mealtimes need to be addressed as well. Older adults have experienced significant changes to where and with whom they dine, and when these changes happen, the effort of grocery shopping, meal planning, and meal preparation can often be extremely daunting. My suggestion: don’t force old habits. Instead, attempt to establish new routines, keep nutritious snacks nearby and keep yourself on a schedule that includes sleep, activity, socialization, and eating. It can be helpful to reach out to various friends/family for reoccurring group meals, attending a community lunch, or rethinking the size and frequency of your in-home meals.
The aging process is difficult for numerous reasons, and to this point, I think we ought to arm ourselves with as much research-based knowledge as possible. While the research is concerning for the standard American diet and memory decline, it also informs us of some nutrition habits that can directly be addressed. Use the resources in our community and in your personal life to decrease the saturated fat and sugar you consume, by reducing the amount of pre-packaged foods, fast-foods, and convenience foods. Your brain will thank you.

Sara Smith Maguire, M.D. FACS
It may not be the most glamorous subject, but talking about colorectal cancer saves lives. Among cancers affecting both men and women, it is the second leading cause of cancer-related death in the US. Unlike many cancers, we have effective tools to help decrease the development of colorectal cancer and identify its presence at an earlier stage.
The risk of colorectal cancer increases with age, with more than 90% of the cases we see being diagnosed in people age 50 or older. There are many factors that are associated with an increased risk of colorectal cancer. Some of these risk factors are related to lifestyle choices and are therefore modifiable. Maintaining a healthy weight, being physically active, not using tobacco, avoiding heavy alcohol intake and eating a balanced diet that limits intake of red or processed meat can all help decrease your risk. Some risk factors can’t be changed; these include increasing age, a family history of colon cancer, inflammatory bowel diseases and belonging to certain ethnic groups.
Colorectal cancer may cause symptoms as it grows. These symptoms include seeing blood in or on your stool, unintentional weight loss, a change in bowel habits and weakness or fatigue caused by a low blood count.
Screening is the practice of looking for cancer or pre-cancer in individuals without symptoms. Screening is incredibly effective when it comes to colorectal cancer because, from the time the first abnormal cells start to develop, it takes on average 10-15 years for those cells to become cancer. Screening is one of our most effective tools for preventing colorectal cancer because it allows us to identify precancerous polyps and identify small cancers that aren’t yet big enough to produce symptoms.
There are several screening tools for colorectal cancer, including colonoscopy which allows us to both find polyps and remove them. Talking to your doctor about your risk factors can help identify the most effective and appropriate screening test for you. In general, screening is recommended between the ages of 50 and 75, though there are reasons to start earlier or stop later for some people. Every year, about 140,000 people in the US will be diagnosed with colorectal cancer and 50,000 people will die from it. Our best tool to decrease both of these numbers is screening. Talk to your doctor today.
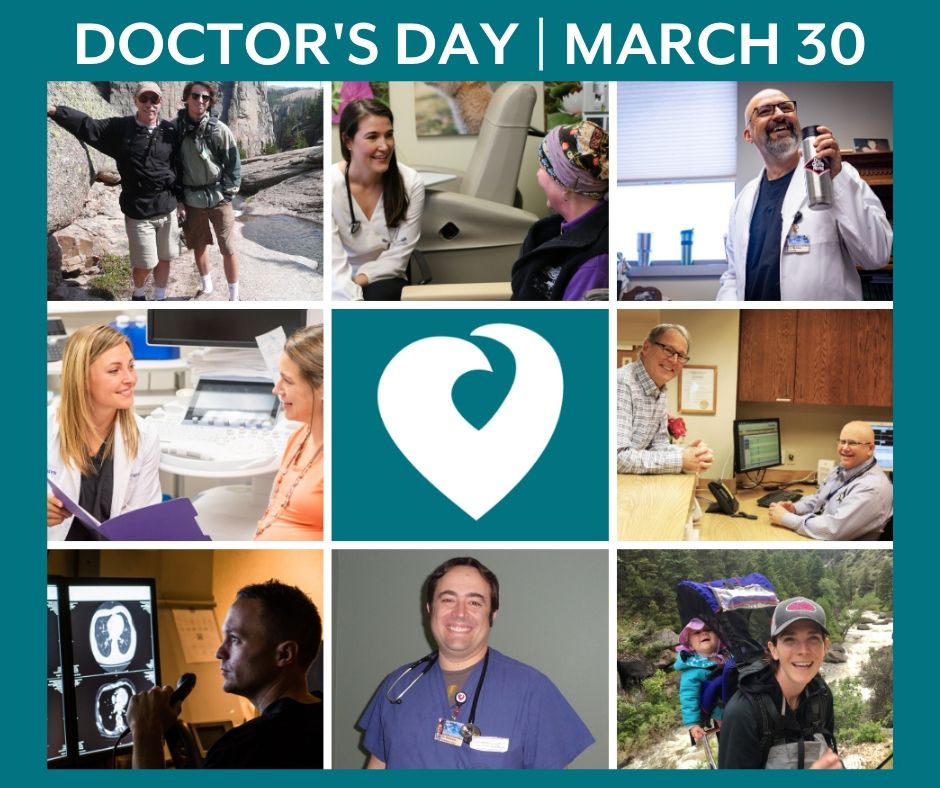
Why do we celebrate Doctor’s Day each year? Learn more about celebrating Doctors in our community and how you can contribute a message of thanks from the comforts of your own home.
National Doctors’ Day falls every year on March 30, and it is our time to say thank you for the passion, dedication, commitment, and excellent healthcare doctors offer to our community. It is a day to celebrate the contribution of physicians who serve our country by caring for its’ citizens in all areas of medicine.
Living in a rural community, we are lucky to have doctors who will work tirelessly better themselves to ensure patients receive medical excellence – right here at home. From the certifications, they continue to renew and receive; to the advancements in medicine and technology, our Doctor’s study and practice, their profession demands constant innovation to better the lives of one’s patients.
This Doctor’s Day, share a Thank You with your Doctor as they keep our community safe and healthy. Be it a smile at your next appointment or comment here, let the Medical Staff of Sheridan Memorial Hospital and this community know that we appreciate their hard work and dedication.

This Month’s Working on Wellness Employee of the Month is
Internal Medicine’s Hannah Hall, MD! Hannah prioritizes her health not only for
herself, but for her family, patients, and staff as well. She discussed the
importance of priorities, a healthy lifestyle, and preventative health.
Health has always been an important part of Hannah’s lifestyle and she’s taken
many of the things she gained from an active childhood into her adult life.
“As far as staying healthy I was raised that way. My parents got me involved in lots of activities like tennis, basketball, and soccer,” said Hall. “Growing up we did a lot of outdoor activities like hiking, camping, fishing, hunting, sailing, and water skiing. I had exposure to a lot of activities, including lifelong sports like golf.”
Hannah went on to play tennis in college for a few years and
also participated in intramural sports. She was also a big runner until a knee
injury 5 years ago. Since then, she’s had to find new activities to keep her
healthy and one of those activities is hockey.
“My newest thing is hockey, I started a few years ago as a novice at the rink.
I ice skated a little growing up but not a ton, and I wasn’t very good. Novice is
great and I enjoy it because it’s a lot like soccer and basketball. You get
that same sports feel and its competitive. It satisfies the competitive nature
in me and It’s really fun. I have a smile on my face the whole time I’m out
there,” said Hall.
Along with hockey, Hannah does weight lifting at the hospital’s employee gym
and enjoys using her Pelton bike at home.
When asked what motivates her, she discussed the importance of balancing priorities and making time for self-care.
“You have to figure out a balance in your priorities and for
me that’s taken awhile. You come out of school and your priority is work and
that’s probably not the healthiest to have. For me, I figured out it’s faith,
marriage, family, and then work,” said Hall. “To have those lined out I have to
be healthy and I have to make time for self-care. That’s what motivates me. I
have to take care of myself in order to be available for my family, patients,
and staff.”
For Hannah self-care means exercising, eating healthy, and making time for the
outdoor activities she enjoys. After seeing how health has always been a
priority in her life, it’s easy to see why Hannah is passionate about
preventive health for her patients.
“In my job a lot of issues are related to weight and lifestyle. It’s a big
thing that I talk to people about and I always ask what motivates them. If you
can find out that people are motivated to work on lifestyle changes, I think
that’s the best thing. If you can motivate people to make those lifestyle
changes early on you can prevent things like diabetes and heart disease,” said
Hall.
The advice she would give others who are ready to make a lifestyle changes is to set small goals and to find things you enjoy that you know you can do for a long time.
“Don’t expect that you’re going to go from not exercising ever, to doing an hour a day. Start with small goals and don’t get discouraged if you start a change and you don’t see results right away,” said Hall. “You’re doing something great so give yourself credit. I always ask what works for you? What have you seen success with? Pick something you think you can do for a long time.”

By Joseph Garcia, MD – Cardiologist from Sheridan Memorial Hospital’s Heart Center
February is Heart Month and it is particularly fitting that Sheridan Memorial Hospital has accomplished Accreditation by the American College of Cardiology (ACC) for the treatment of congestive heart failure.
What exactly does this mean?
It means that Sheridan Memorial Hospital has made management and treatment of congestive heart failure a major priority to improve patient quality of life, improve survival rates, reduce hospitalizations, keep patients employed (or doing as much of their daily activities as possible) within the limitations of their heart.
Congestive heart failure occurs when your heart muscle is unable to pump blood efficiently because the heart pump is either too weak or too stiff to be able to function. When the heart is unable to pump efficiently, the pressures inside the heart start to rise and the circulation starts to back up to the point where, in severe cases, you develop fluid in your lungs as well as swelling of your lower extremities.
Persons who start developing heart failure usually begin with symptoms such as shortness of breath on exertion or inability to breathe comfortably while lying flat ad having to prop themselves up to breathe better. Most persons develop fatigue, weakness, a faster than normal heartbeat, reduced exercise tolerance and increased urge to urinate at night. As heart failure symptoms worsen, persons may experience swelling of the abdomen and lower extremities, resulting in rapid weight gain from fluid retention.
Major conditions, which can result in heart failure, include significant obesity, poorly controlled high blood pressure, poorly controlled diabetes and coronary artery disease. Excessive alcohol and tobacco use also contribute to heart disease. Some medications, both prescription and over the counter, can also result in heart damage.
Not all conditions that lead to heart failure can be reversed, but there are treatments that can improve the signs and symptoms of heart failure and help you live longer. A person can undergo lifestyle modifications such as not smoking, controlling diabetes and blood pressure, staying physically active, eating healthy foods, maintaining healthy weight and controlling stress. By reducing these risk factors or undergoing necessary surgical options, heart failure can be minimized. The stronger your heart pump is, the longer the overall life expectancy will be for the patient.
The ultimate goal for diagnosing and managing heart failure is early recognition and intervention. Patients that receive a new diagnosis of heart failure in our facility leave the hospital with a heart failure specific bundle. This bundle consists of a scale, pulse oximeter, blood pressure cuff, a calendar, a recipe book for heart heathy cooking, and an education booklet on living with heart failure. By increasing heart failure education and providing useful tools for success, patients will have a greater awareness and appreciation for their health.

L-R – Nicole Opitz, RN; Brandie Neufer, RN;Lacy Slusser, RN; Angel Vielhauer, RN; Teara Leibee, RN and Megan Perkins, RN.
Six new registered nurses successfully completed the hospital’s six-month Nurse Residency Program. Their graduation ceremony was held last week. This is the seventh cohort to graduate from this unique program designed to support the transition of new RNs to the practice environment.
Key areas of focus in this program are not only clinical competencies necessary to care for patients and families, but the confidence needed to translate their learning and knowledge into clinical practice.
This year’s group was selected from a large number of applicants. Each participant is granted the opportunity to work one-on-one with an experienced nurse preceptor. They complete additional specialized training using a systems based approach to reinforce their education with real world hands-on nursing.
Clinical Educator Tricia Colson and Director of Nursing Lacey Johnson congratulated the cohort and welcomed guests. Tricia expressed the hospital’s excitement about welcoming the new nurses, “Working with this group has been such a wonderful experience for the education staff. As educators, we work hard to provide these RN’s with the skills they will need to be successful and provide great patient care. We thank the managers, supervisors and preceptors for all their work to ensure the success of these residents. We also want to recognize and thank their families for supporting them during the past 6 months.”

Two years ago, Lori was chosen as one of our first W.O.W employees of the month after starting her health and wellness journey. One of her biggest motivators has been to keep up with her son Sean. After becoming a runner and calorie counting she lost over 40 pounds. We recently sat down with Lori to learn what she’s been up to and see where her lifestyle changes have taken her.
Lori’s journey hasn’t been without trials. After losing over 40 pounds she ended up gaining some of the weight back.
“I did the bounce back, I did the yoyo. After I lost the 40 pounds I went on a two-week vacation and I gained back the weight and I was so disappointed. I knew I had to get back again,” said Lori.
That’s when Lori’s mom introduced her to HealthyWage, a website and app that uses cash prizes as a motivator for weight loss. It’s not a weight loss program but an incentive program where individuals bet on themselves.

“In my case I said I would lose 50 pounds in 6 months and I did $65 dollars a month. I didn’t quite reach my goal in 6 months so it let me extend another 6 months. I did reach my goal and at the end I received a sizeable check. My mom and I both did this and we both came up with the best return on investment. It was a huge incentive and for me it was motivation to keep going. It was the fact that it helped motivate me to lose weight,” said Lori.
Strategy and timing are a huge part of Lori’s wellness journey and along with using resources like HealthyWage and the LoseIt app to calorie count, she also incorporates fitness into her everyday life including when she goes on vacation.
“This year we went to Europe and there was no calorie counting there. Sean and I had a goal that we wanted to do a run in every country. We ran in the Alps, Germany and Austria,” Lori said.

After 4 years in the Airforce and 10 years in law enforcement where she was told she had to run, for the first time in her life Lori is really enjoying running. This year Lori will do the 10-miler run again that she’s done since she first started her health and wellness journey. Her family friend, Marv who helped train her for the police academy also does the race every year.
“I’ll do it every year until Marv stops doing it. He’s in
his 90’s and as long as he’s doing it I’m going to do it,” said Lori.
Lori’s story is inspiring and proof that although there may be ups and downs in
your health and wellness journey, the most important thing is to never give up
and that may mean starting over.

New Family Nurse Practitioner
December 2019
Jeff Shideman is a new Family Nurse Practitioner (FNP) at Sheridan Memorial Hospital’s Internal Medicine Practice, but he’s no stranger to Sheridan or Wyoming.
Originally from Minneapolis, Shideman moved out West for a position in Buffalo. Utilizing his first degree in wildlife biology, he took a job doing seasonal field work. While in Buffalo Shideman was introduced to his wife through a mutual friend and has been in Wyoming ever since.
“It’s my 14th year in Wyoming and my family and I have bounced around,” said Shideman, “We’ve lived in Sheridan, Pinedale, and we’ve been in Cody for the past 10 years.”
Healthcare has always been an interest to Shideman. He took first aid classes in high school and college, and had the opportunity to turn it into a career in Wyoming.
“While working in Pinedale I had the opportunity to volunteer with an ambulance service and fell in love with healthcare at that point,” Said Shideman. “I turned it into a fulltime job and went back to school to be a paramedic, then to nursing school, and it worked out to me being a nurse practitioner.”
Shideman recently graduated from the University of Wyoming with his Nurse Practitioner degree and before that he graduated with his second Bachelors degree in nursing. Before going back to school for nursing, he was a paramedic for 10 years in Cody. He then did primary care nursing at a clinic for 3 years in Cody. Shideman did his Nurse Practitioner internship at Sheridan Memorial Hospital this past Summer and was immediately drawn to the culture.
“I really liked everyone I worked with and the culture here. Everyone was very friendly and supportive of me when I was here as a student. The way the staff worked really well together isn’t something you see everywhere,” Said Shideman. “That was one of the big draws for me.”
A father to two boys, he loves spending time with them in the outdoors. Whether it’s hunting, fishing, or camping. As both a family man and an outdoor lover, Shideman is excited to be in Sheridan.
“I’m excited to able to spend time with my family, and to live in an area where we can do everything we enjoy as a family,” Shideman said. “Sheridan offers a lot of what we like to do and it’s a good place for my boys to grow up and go to school.”
***
Jeff A. Shideman
Undergraduate, BS Wildlife Biology: University of Minnesota – Minneapolis, MN
St. Anthony’s Hospital Paramedic Academy, Cycle 85 – Denver, CO
Undergraduate, BS Nursing-BRAND: University of Wyoming – Laramie, WY
Doctorate of Nursing Practice, Family Nurse Practitioner – University of Wyoming – Laramie, WY

Thanks for all you do!
October 2019
This month, Sheridan Memorial Hospital has spent time celebrating with some of the wonderful teams that exhibit excellence in their work every day. Join us in thanking them for their hard work and dedication, all year round, to healthcare in your community.
In an organization of clinical and non-clinical staff alike, folks often forget the thanks that are due to all the team members that make it possible for us to provide excellent care every single day. Sheridan Memorial Hospital is made up of dedicated employees, serving in over 50 departments that contribute to excellent patient-centered care and a Culture of Kindness at your community hospital.
Join us in thanking them for their hard work and dedication, all year round, to healthcare here in Sheridan.




by Nina Beach, Advanced Oncology Certified Nurse Practitioner at Sheridan Memorial Hospital’s Welch Cancer Center
September 2019
Cancer screening and preventive care is an important aspect for overall health. Screenings look for cancer before a person has symptoms. Many cancers, if caught early are much more treatable and potentially curable the sooner they are discovered. Wyoming has a particularly low rate of cancer screening. Sadly Wyoming is ranked 49th in breast cancer screening with mammography, 47th in colon cancer screening, 44th in cervical cancer screening and last in HPV vaccination coverage which isn’t screening per se but another form of cancer prevention.
Many people have the philosophy that they don’t need to see their healthcare provider unless they do not feel well. I have often asked patients if they get their oil changed in their vehicles. The majority of folks say “absolutely”. When I ask them why, they say they want to prolong the life of their vehicle or prevent their engine from having problems and to keep their vehicle in good working order. Caring for our own bodies really is the same, we often can prolong our life and keep our organs in good working order if we are more preventive and proactive in our care.
There are many screening tests available. Research is continually being done to determine if screening actually prolongs life. We know that finding some cancers before they spread or metastasize increases the chance of successful treatment and potential cure. The recommendations for each particular test are weighed out regarding risk and benefit, and some tests are not without risks. Screening tests are not routinely recommended unless the benefit outweighs the risk. Additionally, people are living longer with cancer today than they used to – both because of screening techniques and the fact that treatments continue to improve.
We have seen patients who have metastatic cancer (stage IV) at the time of their diagnosis. They say they could not afford to be tested or see a physician. Paying for screenings should not be a deterrent. There are a number of funding options for those who qualify. The Wyoming Cancer Program reimburses participating providers for some screenings for the uninsured. Sheridan Memorial Hospital’s financial advocates work with people who need assistance paying for cancer screenings and/or have questions about services. Some of the assistance comes from funds raised each October at the hospital Foundation’s: The Link ~ Partners in Pink run/walk.
To set up an appointment for assistance through an SMH Patient Financial Advocate call 307-675-4620.

June 17, 2019
Serving others is evident in Rebekah Montgomery’s approach to healthcare. She is a new Family Nurse Practitioner at Sheridan Memorial Hospital Internal Medicine.
When you work in healthcare, many important factors must be in place to choose this life. Helping people is at the center of it all. When you talk to Rebekah Montgomery, new Family Nurse Practitioner (FNP) at Sheridan Memorial Hospital Internal Medicine (SMH), it is very evident she has a heart for service.
“I always wanted to be a healthcare provider,” Montgomery said. “I love helping people and want to help them lead healthy lives doing what they love to do. I just love serving others.”
A perfect example of this is the medical mission she went on to Kenya in 2013 and an upcoming mission she plans to join in 2020 to Uganda.
“These mission trips are a perfect opportunity to increase access to healthcare for vulnerable populations,” she said.
Montgomery began her tenure recently with SMH on May 27 and began seeing patients on June 4. When asked about her choice to work for SMH, she was very clear about why she chose SMH.
“SMH offers a lot of different specialties you don’t often find in communities our size,” she said. “There is a lot for patients to access right here in Sheridan and I want to help our patients have even easier access to these specialties.”
Prior to accepting the position at SMH, Montgomery was practicing in Cody, WY when an opportunity in Washington state presented itself, but Montgomery said it didn’t feel right, “It seemed like a great opportunity, but we really missed Wyoming. Especially the people, who are so kind and compassionate. My husband and I see this as a place we can raise a family and enjoy the lifestyle we prefer.”
“The school system is amazing, the weather is great and there isn’t much wind,” she added with a smile.
Montgomery will have a primary care focus in her role with the SMH Internal Medicine office, however she has a special interest in mental health and obesity medicine.
“It is important to me to treat the whole person and I really enjoy collaborating with my patients to come up with a plan together,” she states. “There is a stigma with mental health and we need to work together to break it.”
When not in the office, Montgomery and her husband, Luke, love to hike around the mountains and find new places to explore. They love wildlife watching and being outside with their border collie/Australian shepherd named Gypsy. When the colder weather forces her inside, Montgomery says she is an avid reader, but can’t help but pick up a crochet needle or paintbrush for a creative outlet.
Rebekah Montgomery, FNP-C
B.A. Anthropology (concentration in Biology) – University of California, San Diego – La Jolla, CA
B.S. Nursing – BRAND Program: University of Wyoming – Laramie, WY
Doctorate in Nursing Practice, Family Nurse Practitioner – University of Colorado, Colorado Springs

March 20, 2019
Clay Smith, MD picked up a few shifts in the Sheridan Memorial Hospital Emergency Department in December of 2018. As of February of this year, he has permanent status and is the most recent addition to the SMH Emergency Department medical staff.
Dr. Smith comes to SMH from Rapid City Regional where he worked for over five years. He joins Luke Goddard, MD; Jacob Lieb, MD; David Nickerson, MD; William Selde, MD; Erik Smith, MD, Steve Bischoff, PA-C; and Kelly Lieb, PA-C.
Originally from the Rapid City area, Dr. Smith attended Sturgis High School. He earned his undergraduate degree from the University of South Dakota and attended Sanford Medical School before undertaking his residency at East Carolina University in Greenville, NC. He and his wife, Sheereene, an ICU Hospitalist with Rapid City Regional, have a three-year-old daughter.
When asked what attracted him to Sheridan, he says he was looking for something different and really liked what he saw from SMH.
In his free time, Dr. Smith likes to be outdoors. “I’m an avid cyclist and was fortunate enough to be able to participate in the Dead Swede 100 mile bike race last year in Sheridan,” he said. “My family and I also enjoy being outdoors, especially hiking.”
A career in Family Medicine caught Dr. Smith’s attention back in junior high and high school. However, after some time spent in medical school, he knew emergency medicine was more for him.
“Being a doctor has always been my plan,” he said. “I enjoy the variety of emergency medicine and dealing with all aspects of acute care medicine. I guess you can say I like the breadth of the coverage it requires.”
The staff at SMH are excited to welcome Dr. Smith to the Emergency Department. If you see Dr. Smith in the community or in the hospital, be sure to give him a warm welcome to Sheridan.
Clay Smith, MD
High School: Sturgis High School
Undergraduate: University of South Dakota
Medical School: Sanford School of Medicine – Vermillion, SD
Residency: East Carolina University – Greenville, NC