Two generations, one calling: Mother and daughter Jessica Heil and Emileigh Bettles build a legacy of care at Sheridan Memorial Hospital
Sheridan Memorial Hospital invests in the next generation of healthcare professionals—those who live, grow and serve right here in our community. For Med/Surg Manager Jessica Heil and her daughter, Emileigh Bettles, “growing our own” isn’t just a philosophy—it’s a shared journey.
Emileigh, a senior at Sheridan High School and a part-time certified nursing assistant (CNA) at Sheridan Memorial Hospital’s Transitional Care Unit (TCU), didn’t always plan to follow in her family’s footsteps. But everything changed after she enrolled in a high school CNA course. During the class, she shadowed nurses in the hospital’s Med/Surg unit, and that’s when her passion for healthcare blossomed.
“It was originally just another class to take,” Emileigh explained. “But once we started clinicals, I realized how much I actually liked it. My mom, my dad, my grandma—they’re all in the healthcare field. I loved coming to the hospital and seeing what my mom did and how much of a difference good healthcare workers like her can make for patients. So, I wanted to be like them.”
Jessica also hadn’t expected Emileigh to choose the same path.
“Emileigh just liked other things when she was younger. Both her dad and I are in healthcare, but neither of us saw it coming,” Jessica said. “But I’m super, super proud of her, and I love seeing her with patients and hearing from patients about how caring she is.”
Emileigh’s first job was as a CNA at Sheridan Green House, but she transitioned to the TCU shortly after Sheridan Green House became part of Sheridan Memorial Hospital in the summer of 2024. In the TCU, she finds great fulfillment in building meaningful connections with patients.
“I really love working in the TCU because you don’t see a different patient every time,” Emileigh said. “You have the same patients, and you get to build connections with them while helping them get better. You learn their life stories—where they came from, why they came to Wyoming. It’s nice to know that when one of my patients goes home, they’re leaving better than when they came in.”
While Emileigh gained experience on the TCU floor, Jessica offered guidance from behind the scenes.
“I quizzed Emileigh on her CNA skills as we drove to Denver for her certification test,” Jessica said. “It was a refresher for me, too, because what you learn in class can be so different from real-life situations. We also have interesting conversations at home, where I help her work through things like her first patient death.”
Emileigh appreciates her mother’s support—she occasionally texts Jessica with questions about patient charts or the hospital’s ongoing construction—but she also values the independence she and her mother work hard to maintain at work.
“It’s hard to call her ‘Jessica’ at work,” Emileigh laughed. “But I want my coworkers to like and respect me for who I am and not just because I’m her daughter. I want to prove myself as a good coworker.”
Emileigh and Jessica do occasionally cross paths at work. One rainy day, Jessica and Emileigh worked side by side to help a patient who needed assistance getting from his car into the hospital.
“Emileigh had floated down to Med/Surg from the TCU, so I asked her to help me get the patient out of his car,” Jessica recalled. “It was raining, and the patient’s wife, who was sick, too, was trying to help us, but her husband had a hard time following directions. He couldn’t really stand or get out of the car on his own. We reassured her and got him into the wheelchair, but his wife couldn’t come in because she was sick too. We got him settled into his room, and I called his wife to let her know he was safe and comfortable. She started crying and thanking us. I told her, ‘Please, don’t worry. You take care of you. You get to rest now.’”
A few weeks later, the patient’s wife called again.
“She asked if I was Emileigh’s mother. When I said I was, she told me I should be proud of my daughter for following in my footsteps,” Jessica said. “The best part was that I didn’t even have to coach Emileigh in that moment. She immediately just took over and knew what to do and how to talk to him. But that wasn’t anything out of the usual. That’s just who she is and what she does for all her patients.”
Emileigh’s passion for healthcare extends beyond her workplace. In April 2025, she traveled with Sheridan High School’s SkillsUSA team to the Wyoming State Leadership and Skills Conference in Casper. There, she placed third in the Nursing Assistant event and helped her team earn second place in the Health Knowledge Bowl. The competition, which included both a skills test for CNAs and a quiz-based knowledge bowl, gave Emileigh the opportunity to put her training and experience to the test.
“During the Bowl, they described some symptoms of a condition, and as we talked about it, the face of one of my patients from the TCU popped into my head,” Emileigh said. “I suddenly knew the answer was chronic heart failure. It was great to draw from actual experience and use that to answer the question.”
Sheridan Memorial Hospital proudly supports young healthcare workers like Emileigh by hiring high school students as CNAs and offering flexible schedules to fit school and seasonal commitments.
“If you can only work weekends, great—let’s schedule you then,” Jessica said. “If you can work full-time in the summer, we’ll make that happen. We know some will leave for school, but we don’t turn them away because of that.”
Jessica sees that investment as long-term.
“Our hope is that they come back because they had a great experience. Because they felt welcomed and safe here,” she said. “Our goal is to get them trained here and make them great nurses. Then, even if they do leave for a different, bigger facility, they will be a standout nurse and people will ask when where they learned it all. And they’ll say Sheridan Memorial Hospital.”
As Emileigh prepares to graduate, her sights are set on nursing school. She recently applied for a clinical scholarship from the Sheridan Memorial Hospital Foundation and hopes to begin Sheridan College’s nursing program soon.
“It’s a bit scary,” Jessica admitted. “Because everything’s moving so fast, and she’s my kiddo. But I know who Emileigh is and I know what kind of person she is, so I know that wherever she goes, she’ll be fine.”
Inspired to make a difference?
Join the dedicated team at Sheridan Memorial Hospital and be part of a mission that spans generations. To explore current opportunities, contact our Human Resources Recruiter, Darby Hamilton, at 307.672.1091 or email recruiting@sheridanhospital.org.
Discover what’s possible: sheridanhospital.org/about-us/careers




























 There are encounters, big and small, with our volunteers that make a difference to those who walk through any of our hospital doors. As an organization, we strive to live our mission “to provide our community with excellent patient-centered care.” Patient-centered care includes the obvious – our patients. However, with a patient at the center of something, there must also be something, or someone, to surround them. At SMH, we strive to care for the whole patient by supporting visitors, families, caretakers, friends, and all others who make up any patient’s team.
There are encounters, big and small, with our volunteers that make a difference to those who walk through any of our hospital doors. As an organization, we strive to live our mission “to provide our community with excellent patient-centered care.” Patient-centered care includes the obvious – our patients. However, with a patient at the center of something, there must also be something, or someone, to surround them. At SMH, we strive to care for the whole patient by supporting visitors, families, caretakers, friends, and all others who make up any patient’s team. It is the conversation with a volunteer that goes from talking about the weather to discussing the latest books they like to reach to sharing photos of their grandkids and/or pets, momentarily forgetting a loved one is in surgery.
It is the conversation with a volunteer that goes from talking about the weather to discussing the latest books they like to reach to sharing photos of their grandkids and/or pets, momentarily forgetting a loved one is in surgery. Our volunteer’s actions reflect the true essence of community care, and we are proud to have such dedicated individuals as part of our team. Whether decorating the hallways during the holidays, helping a patient feel at ease during a difficult time, or supporting a family member in need, our volunteers go above and beyond to make a positive difference with all they encounter in our hospital hallways.
Our volunteer’s actions reflect the true essence of community care, and we are proud to have such dedicated individuals as part of our team. Whether decorating the hallways during the holidays, helping a patient feel at ease during a difficult time, or supporting a family member in need, our volunteers go above and beyond to make a positive difference with all they encounter in our hospital hallways. One of our SMH volunteers who, in many ways, supports SMH and efforts to grow for our community, contributed to the transformed Transitional Care Unit completed in the fall of 2022. Fast forwarding eight months, I got a call from her letting me know that she wouldn’t be in for a “little” bit to volunteer as she wasn’t feeling her best. She had been rushed to emergency care and later found out she had pneumonia and needed to have a “little” procedure for a partially collapsed lung. I know she was trying not to worry everyone, but a “little” bit? Two weeks later, she was transferred to SMH’s Transitional Care Unit (TCU), where she would stay for the next six weeks. During one of our visits, I distinctly remember her saying, “I couldn’t make it to the TCU open house, and you kept telling me to come get a tour when I was volunteering. I’m so glad it’s here, but this sure wasn’t how I planned to see it.” At that moment, she reaffirmed to me that volunteering made her feel connected to the patient care our community hospital staff and volunteers provide right here at home. To her, this was our mission in action and that SMH is there when we least expect it but need it most.
One of our SMH volunteers who, in many ways, supports SMH and efforts to grow for our community, contributed to the transformed Transitional Care Unit completed in the fall of 2022. Fast forwarding eight months, I got a call from her letting me know that she wouldn’t be in for a “little” bit to volunteer as she wasn’t feeling her best. She had been rushed to emergency care and later found out she had pneumonia and needed to have a “little” procedure for a partially collapsed lung. I know she was trying not to worry everyone, but a “little” bit? Two weeks later, she was transferred to SMH’s Transitional Care Unit (TCU), where she would stay for the next six weeks. During one of our visits, I distinctly remember her saying, “I couldn’t make it to the TCU open house, and you kept telling me to come get a tour when I was volunteering. I’m so glad it’s here, but this sure wasn’t how I planned to see it.” At that moment, she reaffirmed to me that volunteering made her feel connected to the patient care our community hospital staff and volunteers provide right here at home. To her, this was our mission in action and that SMH is there when we least expect it but need it most.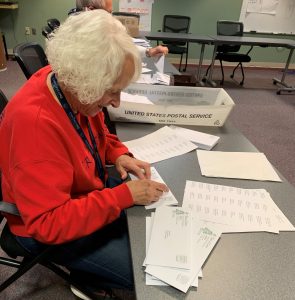 As organizations celebrate Volunteer Appreciation Month nationwide, we want to extend our deepest gratitude to all the volunteers who serve Sheridan Memorial Hospital. To the hundreds of volunteers our visitors have encountered, your efforts make a significant difference in the lives of our patients and their families, and we are incredibly fortunate to have you as part of our team. Thank you for your unwavering dedication, compassion, and commitment to caring for our community. Your service is a testament to the power of community and the difference you make through selfless giving. We couldn’t do it without you.
As organizations celebrate Volunteer Appreciation Month nationwide, we want to extend our deepest gratitude to all the volunteers who serve Sheridan Memorial Hospital. To the hundreds of volunteers our visitors have encountered, your efforts make a significant difference in the lives of our patients and their families, and we are incredibly fortunate to have you as part of our team. Thank you for your unwavering dedication, compassion, and commitment to caring for our community. Your service is a testament to the power of community and the difference you make through selfless giving. We couldn’t do it without you.




 Wyoming Rehab’s
Wyoming Rehab’s Daniel’s gait analysis revealed key insights into his running form. Video footage showed a pelvic drop of more than six degrees, suggesting reduced lateral hip strength. This kind of asymmetry commonly contributes to running injuries. To address this, Lindsay recommended exercises to strengthen the gluteus medius and hip rotators, as well as targeted training to help Daniel maintain a level pelvis while running.
Daniel’s gait analysis revealed key insights into his running form. Video footage showed a pelvic drop of more than six degrees, suggesting reduced lateral hip strength. This kind of asymmetry commonly contributes to running injuries. To address this, Lindsay recommended exercises to strengthen the gluteus medius and hip rotators, as well as targeted training to help Daniel maintain a level pelvis while running.